CONTENTS:
- DIC physiology
- 7 CONDITIONS THAT ARE HIGH RISK DIC
- 1. Severe PreE/HELLP
- 2. Amniotic Fluid Embolism (AFE)
- 3. Abruption
- 5. Hemorrhage
- 4. Acute Fatty Liver of Pregnancy (AFLP)
- 6. IUFD (retained fetal demise/stillbirth)
- 7. Sepsis
Disseminated Intravascular Coagulation in Obstetrics




DIC in Obstetrics article:
Disseminated intravascular coagulation – causes, symptoms, diagnosis, treatment, pathology
DIC in Pregnancy – Pathophysiology, Clinical Characteristics, Diagnostic Scores, and Treatments
7 CAUSES OF DIC


Mechanisms of DIC
- Massive hemorrhage with rapid loss and consumption of clotting factors in hemostasis attempt (Hemorrhage)
- Tissue Factor Systemic Activation (widespread, inappropriate cascade activation from TF entering maternal circulation) (abruption, AFE, IUFD)
- Liver failure —> failure to produce clotting factors (AFLP, HELLP)
- Microvascular endothelial inflammation & damage exposes collagen —> activation & consumption of PLT/factors (Pre-E, HELLP, Sepsis)
SEVERE HTN D/Os OF PREGANCY
Pre-E & HELLP
- PreE comes in mild-severe cases, whereas HELLP is ALWAYS severe, ALWAYS an emergency.
- DIC risk comes from widespread microvascular inflammation activating and consuming PLTs and clotting factors. Compounded, especially in HELLP, by liver dysfunction impairing clotting factor synthesis.
HELLP has 20-30% risk of DIC
H: Hemolysis EL: Elevated Liver LP: Low Platelets
H: Hemolysis and Low PLT: : as systemic inflammation of microvasculature activates PLTs—> activates coag cascade —> forms PLT plugs and then tiny fibrin clots along the microvascular endothelium, the RBCs floating through these micro vessels get damaged/sheared from scraping along these hardened fibrin clots. = schistocytes on blood smear = little sheared rbc fragments/damaged rbcs. This indicates profound widespread microangiopathic thrombosis and is considered a hematologic emergency. (HELLP, hemolytic anemia, TTP, HUS) Coags and TEG to measure ptt/PT/inR/Fibrinogen, clot speed, strength, and duration
The HELLP syndrome: Clinical issues and management. A Review
AMNIOTIC FLUID EMBOLISM (AFE)
- An Analyphyactoid reaction to amniotic fluid breeching maternal-placental interface and entering maternal circulation.
- Amniotic fluid contains cellular elements/other debris (lanugo hair & vernix). Mucin from meconium causes a particularly intense reaction in the pulmonary arterioles. DIC 2/2 AFE does not appear to depend on quantity of amniotic fluid that enters maternal circ or reaches pulm circ – therefore believed to be pt-dependent anaphylactic/anapylactoid response.
- This breech may commonly occur in normal pregnancy, but only SOME WOMEN have an anaphylactoid response to it.
- Other women can have “AFE” or small amounts to amniotic fluid enter their circulation and have no response.
- AFE cardiovascular collapse and DIC is believed to be an anaphylactoid reaction to unknown fetal antigen in amniotic fluid.
- rapid dyspnea, hypoxia —> CV collapse, then pt progresses into DIC
- Given clinical presentation resembling analphylaxis – massive histamine release from anaphylaxis/anaphylactoid reaction makes it prudent to give normal anaphylaxis meds too:
- 10-100mcg IV epi to response, hydrocortisone 100-200mg, famotidine, diphenhydramine, albuterol.
Up to Date – Great AFE Review:
RULE OUT:
- Total spinal
- L.A.S.T *
- Eclampsia/seizures
- Pulmonary Embolism
- Anaphlaxis
- Septic shock
DIC from AFE
- Widespread systemic inflammation causes PLT/clotting factor activation and consumption
- Also Amniotic fluid contains vasoactive and procoagulant products including PLT-Activating Factor, cytokines, bradykinin, thromboxane, and arachidonic acid. Tissue Factor concentrations in amniotic fluid are higher than in maternal circulation, and cause widespread coagulation cascade activation when it enters maternal circulation. THIS TF WILL ACTIVATE THE COAGULATION CASCADE THROUGHOUT her entire body —> mechanism for rapid consumption of clotting factors —> DIC
- Extrinsic pathway activation: [TF & F7a complex ]—>common pathway: [(F10 +F5)]—> F2(prothrombin) —> F1(fibrin) (+F13 (fibrin stabilizing factor)
- Possible maternal increases in endothelin when amniotic fluid enters vasculature. Endothelin has powerful bronchoconstrictive and pulmonary vasoconstrictive properties, which may contribute to CV collapse.
- Unknown why some women have anaphylactic response, where other women do Not.
- Possible prior exposure & sensitization to amniotic fluid may contribute in some cases.
Proposed Physiology of CV Collapse
- PLT activation & degranulation releases serotonin & thromboxane A2 (which normally are powerful vasoconstrictors to help hemostasis — but cause massive pulmonary vasoconstriction in AFE.)
- Pulm vasoconstriction/HTN leading to cardiorespiratory failure
- Causes severe RV dilation & failure. LV compromised from bulging RV –> pulm edema and LV failure
- CBP/V-A ECMO/IABP/RVAD
- Inhaled N.O.
- MTP/cryo/recombinant F7a for coagulation factor consumption/DIC
- Vasopressors/inotropes
- Causes severe RV dilation & failure. LV compromised from bulging RV –> pulm edema and LV failure
- Vagal reflex—> bradycardia & vasodilation.
- INTUBATION: PPV can worsen PVR and RV failure, of course we have to secure the airway, but pt may have full CV collapse after intubation and initiation of PPV.**
- ULTIMATELY PT MAY NEED VA ECMO, despite coagulopathy:
VA ECMO case report, and AFE review link:

A-OK Therapy for AFE
- Atropine 1mg : blocks ACH to inhibit vagal reflex
- Ondansetron 8mg : blocks serotonin : 5HT causes pulm vasculature vasoconstriction & PLT entrapment
- Ketorolac 30mg : blocks Thromboxane A2: thromboxane A2 activates PLT to recruit more PLT in pulm vasculature, worsening pulm HTN and RV strain
AOK-for-AFE-HANDOUTS-no-references
Atropine, Ondansetron, and Ketorolac: Supplemental Management of Amniotic Fluid Embolism
Amniotic Fluid Embolism Part 1: Clinical Presentation and Diagnosis
Amniotic Fluid Embolism Part 2: Management and the 3 B’s
SMFM: Amniotic Fluid-Embolism, Patient Safety, Maternal Morbidity, Maternal Mortality
INTRALIPID FOR AFE?
Two case studies have come out showing ROSC achieved after intralipid administered during suspected AFE, both in situations where the total amount of LA given was far below toxic levels.
- Effectiveness of intralipid hypothesized to have its own intrinsic inotropic properties and pulmonary vasodilatory properties, which would improve cardiac function in the setting of pulm vasoconstriction and resultant RV strain/failure that develops in AFE.
- When all else fails, can’t hurt to try intralipid adminstration!!
Podcast: ACCRAC Episode 216: Intralipid for AFE
Episode 216: Intralipid for AFE
Intralipid for Amniotic Fluid Embolism (AFE)
Lipid Emulsion Rescue of Amniotic Fluid Embolism-Induced Cardiac Arrest: A Case Report – PubMed
ABRUPTION


- A couvelaire uterus is a hemorrhage into the myometrium itself, where uterine muscle swells with blood & impairs contraction. Can be seen in concealed abruption hemorrhages. Can cause life-threatening hemorrhage if contraction impaired. Uterus has swollen purple appearance. Caused by: abruption, HTN, trauma, and intrauterine infection.
- DIC risk in Abruption stems from TF from the retroplacental clot entering maternal circulation. As the placenta pulls off the uterine wall and disrupts the normal maternal-placental interface where blood normally never mixes, embryonic Tissue Factor accumulating in the clot can enter maternal circulation and cause widespread systemic activation of the clotting cascade.
- The risk of DIC associated with abruption comes from potent, concentrated placental and fetal Tissue Factor (thromboplastin) flowing freely through maternal circulation.
- TF is present on the surface of cells (macrophages, endothelial cells, & monocytes) and is exposed to local, nearby circulation after endothelial injury to initiate the clotting cascade for hemostasis, however it does not normally float freely through circulation. This TF free-for-all causes a widespread, totally inappropriate activation of clotting cascade through all maternal vasculature, rapidly consuming clotting factors
- The risk of rapid development of DIC in these pts makes neuraxial high-risk.
- If pt has coags SINCE diagnosis of abruption
- if fibrinogen, coags, PLTs fine, then spinal is probably OK, and plan to convert to GA if severe instability/long case duration etc.
- If NO COAGS *SINCE* DIAGNOSIS – NO NEURAXIAL. GA for C/S in stat situation where we cannot wait for coags. (There will usually be fetal instability in abruption—> c/s)
- Expect maternal instability from concealed hemorrhage.
OR SETUP FOR ABRUPTION
- All GA Airway supplies: ETTs, glidescope, LMAs, induction meds: etomidate if HD instability
- TXA, Blood, FFP, PLT in room, cryo
- 2 large bore IVs.
- Fluid warmer & blood tubing
- A-line available
- If epidural catheter is in place from before abruption (from labor) LEAVE in place until stable coags/teg/PLT. DO NOT REMOVE catheter after c-section/delivery.
- OK to use to bolus for c/s if catheter already in place – watch for HD instability with sympathectomy. If already HD unstable – may be better to just go to GA as pt will not tolerate further sympathectomy.
HEMMORRHAGE
CAUSES OF HEMORRHAGE
4 Ts : Tone, Trauma, Tissue, Thrombin
- Tone: Uterine Atony
- Trauma: Lacerations
- Tissue: Retained placental tissue/ invasive placenta (accreta spectrum)
- Thrombin: coagulopathies (DIC: PreE, HELLP, abruption, AFLP)
INCREASED RISK OF ATONY:
- GA (sevo uterine smooth muscle relaxation)
- Uterine overdistention (twins or polyhydramnios)
- Prolonged labor, oxytocin use during labor (decreased receptor responsiveness)
- Uterine leiomyomas or fibroids (impaired contractility)
- Operative delivery and intrauterine manipulation
- Previous hemorrhage in the third stage of labor
- Uterine infection** Chorioamnionitis
- Extravasation of blood into the myometrium (Couvelaire uterus)
- Intrinsic myometrial dysfunction.
- Use of tocolytics: terbutaline, MgSo4-
- mag is NOT used as a tocolytic OR antiHTN – only used for seizure prevention in preE/HELLP and for fetal neuroprotection for preterm births, however tocolysis and HOTN are known side effects of Mag administration.
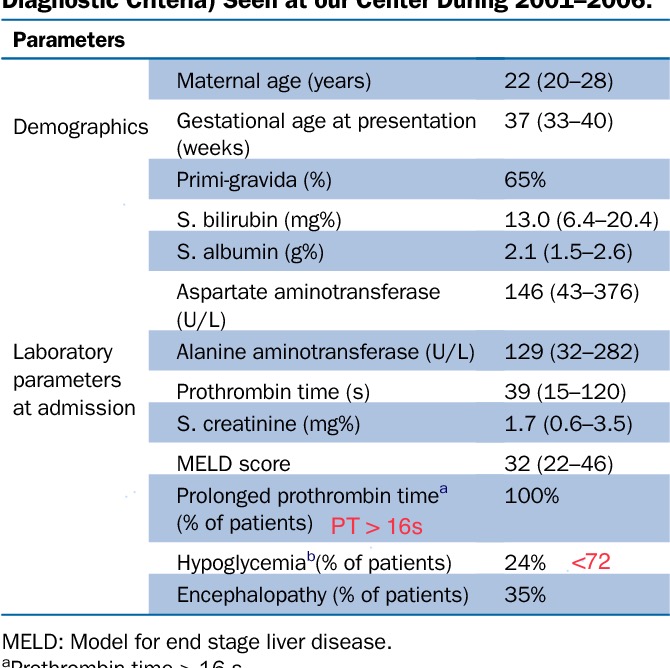
Acute Fatty Liver of Pregnancy
80-100% CHANCE of D.I.C
- AFLP – is a rare, potentially fatal complication
- Cause unknown – possible link to fetal fatty acid metabolism
- Difficult to diagnose d/t overlapping s/s w: PreE, viral hepatitis, cholestasis of pregnancy
- Occurs in 3rd TM – early postpartum period
- Supportive care & ASAP delivery critical.
- 80-100% go into DIC.
- DIC 2/2 fulminant hepatic failure
- Encephalopathy possible* pt “acting strange”
- Dx w/ H&P, labs, imaging – liver biopsy rarely indicated.
Acute fatty liver of pregnancy
Great podcast episode to better understand AFLP: A midwife had it and came on to talk about it – pretty wild..
Interview with an Acute Fatty Liver of Pregnancy Survivor and Midwife

IUFD (Intrauterine Fetal Demise)
- Fetal death after viability/stillbirth > 20wks
- ~20% chance of slow, chronic DIC (and chance of sepsis!) if fetus retained >3-4wks. Called a “Silent DIC” & difficult to diagnose bc it’s slow onset allows time for compensation.
- DIC occurs after 2-3 weeks of fetoplacental unit breaking down/macerating and slooowly releasing fetal/amniotic thromboplastic substances into maternal circulation —> cascade activation via TF extrinsic pathway, (similar to Abruption/AFE mechanism, but MUCH slower)
- Retained Fetus can also become a source of infection —> sepsis —> endothelial inflammation —> PLT activation and consumption (just like preE)
- Usually IUFD diagnosed much sooner and there is very unlikely DIC risk if managed early. (we still get coags on admission prior to neuraxial)
- Vaginal births usually. Epidurals fine as long as pt has normal PLT/coags during this admission. Do not need to trend or re-draw, unless abnormal.
- Earlier epidural beneficial bc sometimes with these small fetuses, mom isn’t uncomfortable until she about to push, and we can miss our chance to get an epidural in.
- Also Pre-term uterus less sensitive to oxytocin – methergine may be 1st line uterotonic if post-partum hemorrhage.
- Near-term IUFD may be delivered via c/s. These can be done under spinal if labs OK. GA can be offered as an option for maternal comfort, however high-risk obstetric airway applies to ALL parturients. Airway swelling and aspiration risk is not exclusive to obese/high mallampati/sub-optimal airway exam pts. Every parturient has increased risk of airway swelling and aspiration, especially closer to term.
- If patient does not wish to be awake/aware of procedure under spinal, timely versed administration on arrival to OR after quick time out, and versed +/- ketamine intra-op can be a safer alternative to GA. (no viable fetus to consider)
- Propofol inappropriate for sedation in pregnant pts. Fent can be used, but small doses and careful mixing with versed – watch for hypoventilation – FRC decreased in pregnancy – all rules of pregnant resp physiology and airway management apply here even though she may be pre-term at time of IUFD.
- If patient does not wish to be awake/aware of procedure under spinal, timely versed administration on arrival to OR after quick time out, and versed +/- ketamine intra-op can be a safer alternative to GA. (no viable fetus to consider)
SEPSIS
Maternal sepsis and ICU care SOAP online recorded ppt/ zoom webinar:
https://soap.mclms.net/en/package/8621/course/18189/view#course-content
Causes of Peripartum Sepsis
- Obstetric causes:
- Chorioamnionitis, Septic abortion/IUFD/stillbirth, Cerclage infection, C/S wound infection, Episiotomy infection
- Non-obstetric causes
- Pneumonia*, Pyelonephritis, Appendicitis, Cholecystitis
CMQCC Maternal Sepsis 2019 2-Step Diagnostic Approach
Step 1: Any Suspicion of Infection
(SIRS criteria modified for pregnancy)
- Oral Temp: < 36 or > 38
- HR > 110bpm
- RR > 24/min
- WBC > 15K or < 4K, or >10% bands
POSITIVE if 2/4 criteria met.
ACTION:
- Start ABT, IVF, increased surveillance
- MOVE TO COMFIRMATION EVALUATION:
STEP 2: Confirmation Evaluation
- Resp: new need for mechanical vent
- PaO2/FiO2 < 300
- Coags: PLT < 100k, INR> 1.5, or PTT > 60s
- Liver: bilirubin > 2mg/dL
- CV: SBP < 85, MAP < 65, or > 40 mmHg decrease in BP
- Renal: Creatinine > 1.2 or doubled from baseline.
- Mental Status: agitated, confused, unresponsive
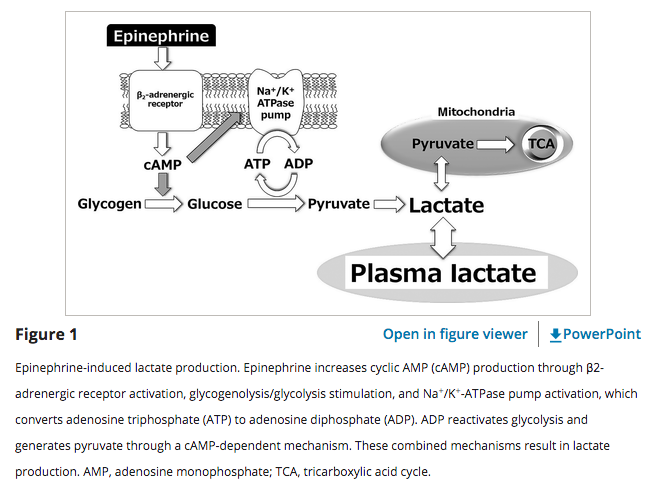
- Lactate: > 2mmol only in ABSENCE of labor.
CONFIRMATION IF 1 CRITERIA met
Lactate & Sepsis
- Lactate > 4mmol/L –> start 30cc/kg fluid bolus
- Lactate can reach 2-4 during NORMAL labor (usually does not exceed 4).
- Elective c/s, or pt not in labor with high lactate would be abnormal*
- DO NOT base resuscitation on lactate levels
- YOU WOULD FLOOD YOUR PATIENT.
- 2L IVF only decreases lactate 5.2%
- Ex: lactate 8, 2L ivf —> lactate still 7.5. Negligible response to fluid, and would require harmful fluid overload. Don’t focus on lactate.
- #1 cause of pulmonary edema in pregnancy is iatrogenic fluid overload
- Ex: lactate 8, 2L ivf —> lactate still 7.5. Negligible response to fluid, and would require harmful fluid overload. Don’t focus on lactate.
- SERUM LACTATE is NOT a direct measure of tissue perfusion.
- anything that increases glucose or pyruvate metabolism will increase lactate
- ex: catecholamine increases, epi gtt, Beta agonists (ie: LABOR)
Preferred vasopressors: Norepinephrine & vasopressin, with benefit shown in starting vasopressin early.
An Obstetric Sepsis Case Study
Online Lecture:
Diagnosis and Management of Shock States that can Complicate Pregnancy – OpenAnesthesia
TEGS
THROMBOELASTOGRAM (TEG) Review:
- Useful in cases where thrombocytopenia is complicated by liver dysfunction, other coagulopathy, or pseudothrombocytopenia.
- Useful in guiding resuscitation in severe hemorrhage/MTP/DIC
- Useful to determine DIC progression and appropriateness of neuraxial interventions or catheter removal.





http://www.emdocs.net/thromboelastogram-teg-five-minute-primer-emergency-physician/