Pulmonary Edema in Pregnancy
- Life threatening 2/2 hypoxemia from impaired O2 exchange at alveolar-capillary membrane.
- ~20% of cases reported IATROGENIC from IV fluid overload (probably much higher)
3 KEY POINTS:
- ANY NEW OR INCREASING O2 REQUIREMENT IN PREGNANCY IS ABNORMAL AND REQUIRES A CARDIAC & PULMONARY WORKUP.
- ANY NEW OR INCREASING O2 REQUIREMENT IN PREGNANCY IS ABNORMAL AND REQUIRES A CARDIAC & PULMONARY WORKUP.
- ANY NEW OR INCREASING O2 REQUIREMENT IN PREGNANCY IS ABNORMAL AND REQUIRES A CARDIAC & PULMONARY WORKUP.
- Pulmonary Edema is rarely “flash” edema, and instead usually develops and worsens slowly over hours, so initial assessment (CXR/Lung US) may look clear, but continued, repeat assessments are required to track changes, as pulmonary edema usually worsens over time.
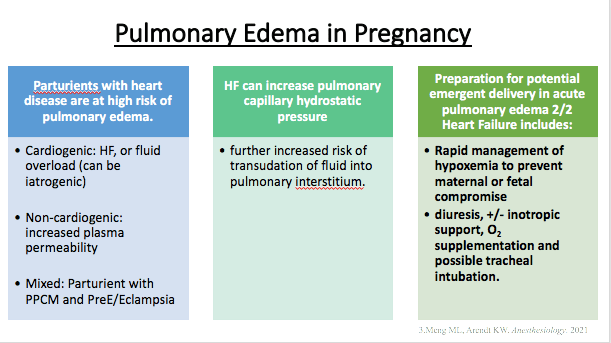
- Can be CARDIOGENIC from high hydrostatic pressure causing increased pulmonary venous congestion (fluid volume overload, high SVR (preE), PPCM, etc) or NON-CARDIOGENIC from capillary leak (PreE, sepsis)
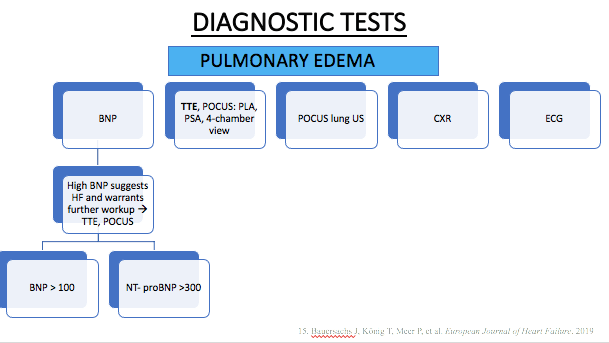
- BNP is a BASIC, EASY, FAST way to determine liklihood of cardiac etiology. Can also be trended and see rise as condition worsens.
- TTE is a BASIC, NECESSARY assessment tool for pulmonary edema to rule out cardiac causes and guide treatment. If TTE unavailable, at LEAST draw BNP to assess for cardiac strain/overload. Elevated BNP in pregnancy generally indicates cardiac etiology: PPCM. (BNP lab values are UNCHANGED in normal pregnancy.)
- New 2025 Pregnancy-specific Guidelines:
- BNP > 50 pg/ml = WORKUP (any trimester)
- Pro-BNP
- TM 1&2: > 200 pg/ml = CARDIAC WORKUP: TTE
- TM 3: >150 pg/ml = CARDIAC WORKUP: TTE
- Source: Dennis et al., ANESTHESIOLOGY 2025; 142:378-402
- New 2025 Pregnancy-specific Guidelines:
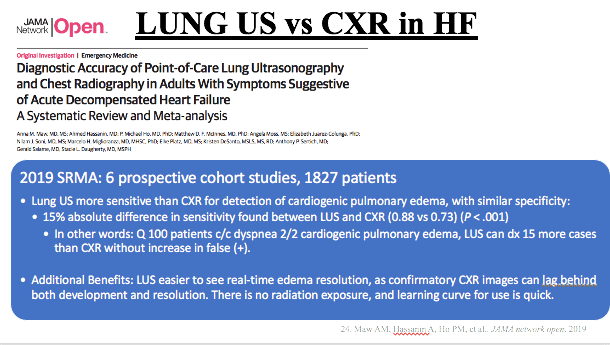
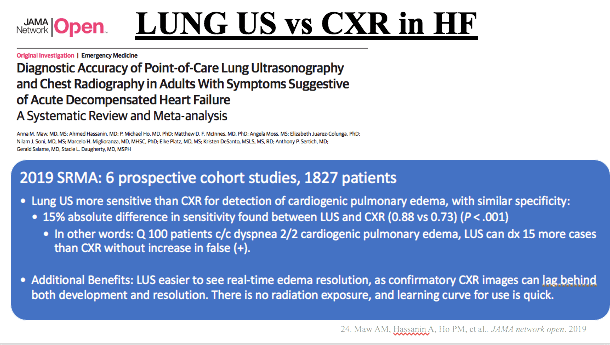
- Lung US technically is more sensitive than CXR to detect pulmonary edema and track progression or improvement, we’re still getting CXRs fam, but for initial quick diagnosis, LUS is faster, more accurate, and can better track resolution.
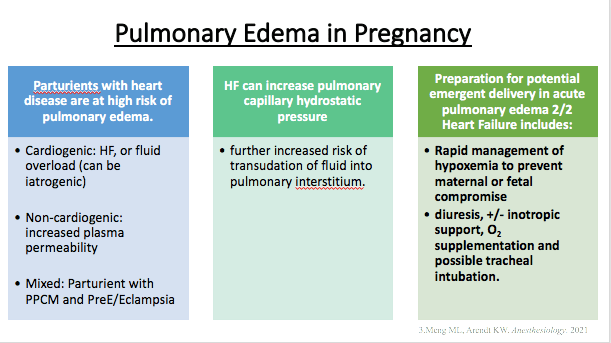
- Normal physiologic changes of pregnancy place parturients at higher risk, and are further compounded by PReE, sepsis, fluid overload and cardiac dysfunction:
- Plasma volume increases ~40% by 28wks, ~50% by 35wks
- Decreased serum colloid-osmotic pressure placing pregnant pts at higher risk of pulmonary edema:
- Compounded risk in setting of:
- Increased hydrostatic pressure 2/2:
- preload (IVF/autotransfusion), HTN d/o of pregnancy (PreE, HELLP, gHTN)
- Beta 2 agonist: terbutaline
- and/or increased membrane permeability:
- (PreE 2/2 endothelial damage, Mag sulfate direct cardiac depression and may cause direct capillary endothelial damage)
- Increased hydrostatic pressure 2/2:
- Compounded risk in setting of:
- Can occur at any time, most likely peripartum 2/2 fluid overload.
- Highest risk after delivery 2/2 autotransfusion & doubled CO …on top of fluid overload.
- High risk w/ diastolic dysfunction 2/2 cHTN (LVH) or PreE (placental inflammatory mediators also affect cardiac myocytes)
- impaired LV relaxation or contraction ^^ pulm venous pressure & disturbs normal Starling balance of hydrostatic/oncotic pressures.
- 24-48h post partum is highest cardiac output state. (80% above pre-delivery, 150% above pre-pregnant CO)
- Will need continuous management through postpartum period (when CO is highest and cardiopulmonary events/failure most likely – at least 72h post-partum, takes 2+ weeks to return to pre-pregnant levels.
RISK FACTORS:

SIGNS/SYMPTOMS:
- SOB, agitation/anxiety, cough, tachycardia, tachypnea, crackles&wheezes, SpO2 drop
TESTS: CARDIAC AND PULMONARY WORKUP
- IMAGE: CXR,LUNG POCUS, TTE,
- ECG
- LABS: BNP, ABG (PaO2)
TX:
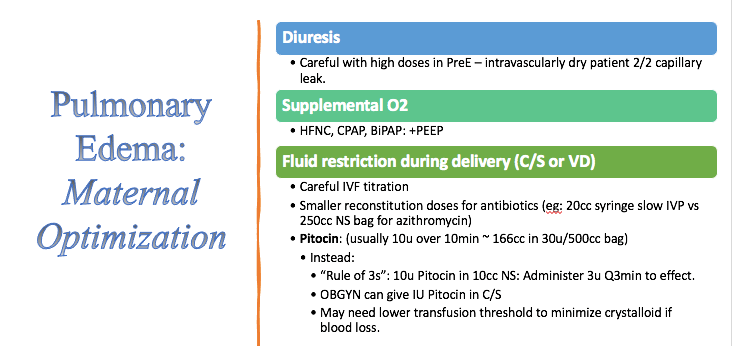
- Lasix to reduce fluid volume
- Nitroglycerin (if HTN – to reduce afterload, improve forward flow, and not impair contractility) – Heart failure may need inotropic support..
- O2: NC, HFNC, NRB, PEEP/CPAP/BIPAP, intubation
- fluid restriction
REVIEW OF PHYSIOLOGY
- Acute pulmonary edema 2/2 impaired CV function & fluid flow into pulmonary interstitium.
- Hydrostatic pressures, colloid osmotic pressures & capillary permeability determine fluid in pulm interstitium .
- Starling’s equation:
Transcapillary Fluid Filtration Rate ∞
Kf [(Pmv – Pt) – (COPmv – COPt)]
- Kf = ultrafiltration coefficient ~ capillary permeability
- Pmv = microvasculature Pressure (~ Parterial – Pvenous)
- Pt = tissue hydrostatic Pressure
- COPmv = microvasculature Colloid Osmotic Pressure (oncotic)
- COPt = tissue Colloid Osmotic Pressure. (Oncotic)
Hydrostatic pressure (Pt) determined by CV function:
- Preload, HR, rhythm, contractility, lusitropy & afterload/SVR
- Arterial & venous tone 2/2 nervous system & catecholamines/vasoactive substances.
- Systemic & pulmonary circulations function in parallel
- CO = Venous Return
- Frank-Starling = same SV in RV & LV.
- Acute pulmonary edema or acute CHF = system out of balance & unable to meet tissue metabolic needs.
- Fatal if untreated.
Hydrostatic pressure increases 2/2:
- Fluid accumulation, overload & retention – hypervolemia
- Fluid redistribution from systemic circulation to pulmonary circulation 2/2 venoconstriction or vasoconstriction in euvolemia
- Increased hydrostatic pressure elevates LVEDP
- Tocolytic beta 2 agonist: terbutaline increases HR, CO, hydrostatic pressure
Capillary permeability increases 2/2:
- Increased plasma volume of pregnancy in setting of decreased colloid osmotic pressure (dilutional decreased serum albumin in pregnancy 2/2 ^^TBW)
- Endothelial damage from PreE/HELLP
- Mag sulfate may cause direct endothelial damage, but should not be withheld from PreE pts, as seizure risk must be managed.
TWO PULMONARY EDEMA RISK GROUPS IN PREGNANCY
- Non-Hypertensive = similar tx to non-pregnant pt
- Hypertensive: = PreE = unique dx of pregnancy w/ special considerations
NON-Hypertensive
- May be normotensive or hypOtensive.
- 2/2 impaired pulmonary interstitial fluid regulation:
- Hydrostatic pressure, colloid osmotic pressure & capillary permeability
- Reduced pulmonary reserve in pregnancy = reduced tolerance.
Caused by:
- Tocolysis:
- β-2 agonist increases CO & hydrostatic pressure
- Sepsis
- PreE – microvascular endothelial damage ****
- Pre-existing CV dx
- Pregnancy-assc CV dx (PPCM, ischemic heart disease)
- BBs reduce myocardial contractility
- AFE w/LV systolic failure
- Aspiration
- Iatrogenic IV Fluid overload
- Steroid use: Celestone = Betamethasone (for fetal lung maturity)
- Magnesium sulfate (for neuropotection in preterm for non-HTN pt) may cause direct cardiac depression or direct capillary damage
Treatment Non-Hypertensive:
- Lasix, O2, fluid restriction, PEEP/CPAP/BIPAP/intubation, +/- inotropic support if in heart failure. MAY REQUIRE ECMO. VA if HF/cardiogenic shock, VV if no cardiogenic shock.
Hypertensive Pulmonary Edema
* Consideration of delivery if antepartum acute pulmonary edema.
Caused By:
- cHTN, preE, SIPE, gHTN
- Illicit drug use HTN
- Endocrine dx: pheochromocytoma, hyperthyroidism
- PreE:
- Diastolic dysfunction & higher LVEDP (higher hydrostatic pressure)
- Reduced plasma colloid osmotic pressure, colloid osmotic pressure & increased endothelial permeability
- Endothelial damage in preE/HELLP increases capillary membrane permeability
- Mag sulfate for seizure prevention is independent risk factor for pulmonary edema 2/2 theorized direct cardiac depression and direct capillary damage
- HTN crisis (higher LVEDP/hydrostatic pressure)
Goals of TX in HTN Pulmonary Edema:
- Reduce LV PREload & AFTERload (without causing ++HOTN in IV dry PreE pt)
- Reduce/prevent myocardial ischemia.
- Adequate O2 & ventilation w/ clearance of pulmonary edema
Treatment HTN Pulmonary Edema:
- O2 & ventilation
- Nitroglycerin & Lasix
- OFFLOAD VENTRICLES AND MOVE FLUID FORWARD WITHOUT DECREASING CONTRACTILITY
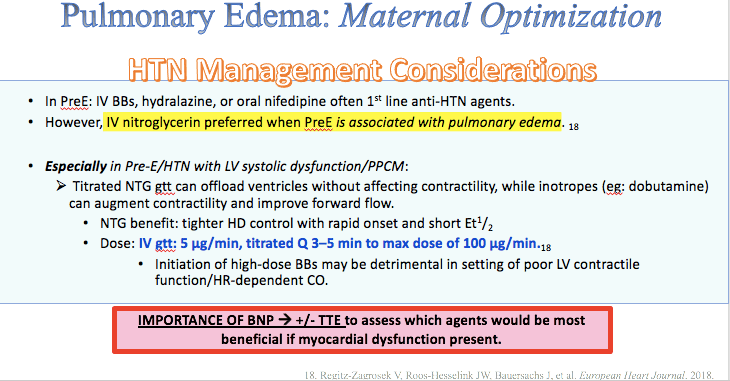
- Although beta blockers* (labetalol) are commonly used as 1st line HTN tx in PreE, this should only be used in Pulmonary Edema with an EF > 40%. which means a TTE is REALLY IMPORTANT to guide tx. At the very least – a BNP >100 can help you distinguish possible heart failure, warranting further cardiac workup – and in the meantime, BBs and CCBs should probably be avoided. HF may actually need inotrope: dobutamine to improve contractility and foward flow. [combo of slow nitroglycerin dosing + dobutamine may be optimal in cases of reduced EF]
- O2 and Ventilation: early and aggressive management of oxygenation and ventilation:
- HFNC, CPAP, BIPAP, Intubation if needed.
- *better options than NC, face mask, or NRB as none of these provide any of the positive pressure or PEEP needed to improve ventilation through fluid-filled alveoli. (even HFNC provides ~5+cm H2O PEEP and increases FRC by augmenting pulm airway pressures)
- FiO2 max for each device:
- NC (4-6L/mn) = ~ 37-44% FiO2 (no PEEP)
- Face mask (10L/min) = ~ 50% FiO2 (no PEEP)
- Venturi (15L.min green adapter) = ~ 60% FiO2 (no PEEP)
- NRB (10-15L.min) = ~ 80% FiO2 (no PEEP)
- HFNC, CPAP, BIPAP= up to 100% FiO2 + PPV & PEEP
- Remember maternal SpO2 > 95% ideally required for both optimal fetal oxygenation and to meet demands of higher maternal MRO2 of pregnancy. Fetal Hgb has left shift, meaning it’ll hang on to O2 better than maternal Hgb. The WHO recommends maternal SpO2 goal of at least 92-95%.
- HFNC, CPAP, BIPAP, Intubation if needed.
- Nitroglycerin: GENTLY AND SLOWLY TITRATED
- IV: 5mcg/min, gradually increasing Q 3–5 min, to max 100 mcg/min−1.
- SL spray: (400mcg, 1–2 puffs every 5–10min
- GOAL IS TO Reduce SBP/DBP SLOWLY: 30mmHg over 3–5min, then slower reduction to ~140/90mmHg.
- A PreE pt is INTRAVSCULARLY DRY at baseline from endothelial damage causing third spacing – rapid vasodilation can cause profound HOTN (and drop in placental perfusion pressure).
- Nitroglycerin has benefit of rapid/immediate onset and titratibility compared to onset times of hydralazine, and labetalol (BB would also decrease contractility) although can still be used in appropriate situations..
- Furosemide:
- IV: 10-40mg over 2 min, repeat 20–60mg after ~ 30min if inadequate diuresis (maximum dose 120mg/hr) *careful in severe PreE – pt is already intravascularly dry from microvascular damage causing third spacing! Can start with smaller doses of lasix to avoid hypotensive collapse with severe hypovolemia..
- 2nd line anti-HTN: CCB nicardipine/nifedipine (esp if diastolic dysfunction is diagnosed)
- 3rd line: Morphine 2-3mg IV (to reduce preload)
PreE and Pulmonary Edema
PreE places women at uniquely high risk from 2 co-existing factors:
- 1) Systemic vascular endothelial inflammation and damage causing BOTH capillary leak at alveolar-capillary membrane (non-cardigenic)
- 2) AND high SVR from HTN causing both LV dysfunction/cardiomyopathy, as well an increased pulmonary venous pressure increasing hydrostatic pressure at alveolar capillary membrane (cardiogenic pulmonary edema).
- Higher-than-normal hydrostatic pressure at an alveolar capillary membrane that has impaired integrity from inflammation has a lower threshold to leak and cause pulmonary edema. Additionally, the profound microvascular endothelial inflammation and damage that affects every organ in her body, also affects cardiac myocytes; and women with PreE have been shown to demonstrate both myocardial swelling and concentric hypertrophy, which can contribute to myocardial dysfunction that can be either subclinical, or exacerbate existing myocardial dysfunction. This is an overlapping, mixed picture requiring thorough CARDIAC AND PULMONARY assessment to best manage.
ACUTE PULMONARY EDEMA IN PREGNANCY ALGORITHM
Activate emergency response team, then AIRWAY..

SCAPE for Non-pregnant pts, but many steps still apply:

POCUS LUNG US FOR PULM EDEMA IN PREGNANCY
(slides from PPT: Heart Failure in Pregnancy)

BLUE (Bedside Lung US in Emergency) protocol for dx lung us – NYSORA:
Acute respiratory failure: The BLUE protocol – NYSORA
[SOAP lecture on pulmonary edema 2/2 diastolic dysfunction in PreE:
(Repeated in Cardiac Disease & Dysfunction in Pregnancy Page)]
DIASTOLIC DYSFUNCTION IN PREGNANCY
TITLE SLIDE: JULY 2022 Webinar

LINK:
MC LMS – 2022 Webinars – SOAP July 2022 Maternal Critical Care Webinar Series
LECTURE NOTES:
PreE puts women at higher risk of developing DIASTOLIC dysfunction —> pulm edema in pregnancy with fluid shifts, & HFpEF later in life
HFpEF = Heart FAILURE w/ Preserved Ejection Fraction.
- high filling pressure, abnormal relaxation 2/2 myocardial stiffness
- *important to distinguish from systolic dysfunction.
- Don’t let the word “PRESERVED” fool you – this is a failing heart with a preserved FRACTION of a crappy volume – not a preserved normal Stroke Volume. (ie 50% of 100cc LVEDV is 50cc SV, 50% of 40 is 20cc SV… same “EF 50%” but SV and CO are poor
- This is a preserved fraction of a low EDV (caused by a stiff LV) which does not equate to a preserved Cardiac Output. HFpEF often is seen with very impaired diastolic filling.
DISTINGUISHING SYSTOLIC vs DIASTOLIC:

Dilated vs normal vs hypertrophied LV chamber
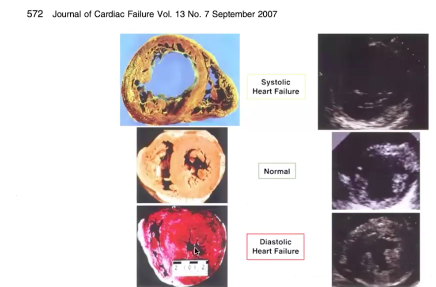
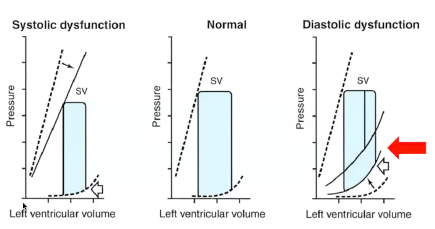
- Diastolic failure = decreased compliance
- More volume = +++ pressure (steep pressure increase with small volume increases)
- Thick heart, impaired relaxation, unable to tolerate extra fluid
- ADD normal physiologic increases in circulatory volume of pregnancy ?? — we’re screwed. Then autotransfusion!? and THEN DOUBLED CARDIAC OUTPUT POSTPARTUM?! Hot mess.
Reminder of NORMAL CV Physiology of Pregnancy:
- NORMALLY: Blood Vol ^^ up to 45% above pre-preg levels, —> assc w HD stress.
- NORMALLY: EF% and LV mass increase 2/2 increased preload —> enlargement of cardiac chambers
Diastolic dysfunction related to:
- Pressure
- Volume
- Impaired relaxation
- Mass/thickness
LAB to evaluate this:
BNP (Brain natriuretic peptide = function of pressure in LV) hormone released when walls of ventricle under high stress. < 100 = non-cardiogenic etiology/pulm edema not due to heart failure. BP >100 BNP LAB VALUE remains normal in pregnancy despite fluid volume increases.
*NT-proBNP level parameters are different, and higher 2/2 the longer half life of NT-proBNP, with less consistent study data on reliable cutoff values to rule in/out cardiogenic etiology.
Evaluation: Imaging Tools:
TTE obvi (no sedation needed vs TEE)
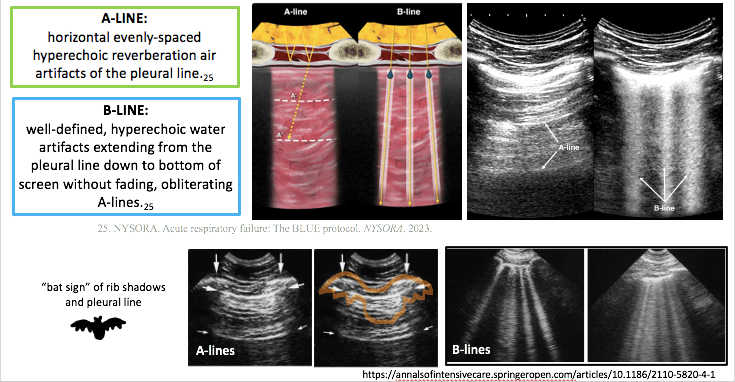
Lung ultrasound to assess for pulm edema:

- A lines = dry lung “A for Air”
- US rays bouncing between air/pleura interface create artifact pattern of repeating horizontal lines
- B lines = high assc w pulm edema:
- (B-lines also seen in covid/pneumonia – so rule out infection/fever)
- B-lines show EVLW (extravascular lung water) = fluid trapped in itralobular septae ~ fluid-filled alveoli – US beams bouncing around and shooting down – creates “sunshine/ sun ray” pattern)
- 3+ B lines in 2 or more segments = abnormal (1 or 2 B-lines in 1 or 2 segments can be normal in pregnancy… but 3+ in multiple segments is NOT normal, and ANY B-lines found in the setting of pulmonary symptoms/SOB/resp distress require further workup.)
- can follow real-time sonographic clearance of B-lines as furosemide administered and lungs “dry out” – once cardiogenic cause ruled out (as cardiac pt may need inotrope to support ventricles and clear edema.
DIASTOLIC FAILURE PT EXAMPLE:
23y/o F arrives to L&D at 30.1wks gestation with NEW acute rise in BP and new onset headache.
PMH: morbid obesity, chronic HTN, Asthma, SVT(remote hx)
Pt admitted to antepartum unit, & over next 24h:
- Acute Rise in BP > 160, & labs confirming preE w SF: proteinuria
- 02 requirements kept increasing over 12h: 2L > 6L > 10L
- FHR tracings deteriorating 2/2 decreased O2 supply.
MFM/OBGYN want to C/S this woman
- BUT WAIT!! FRC decreased, morbid obesity, swollen airway
- what is happening with O2 requirements?
- what is going on?
- Pulm edema?? PE? => ACUTE RESP PATHOLOGY
Do we: Intubate? CT-PE? POCUS, C-Section?
FIGURE OUT CARDIOGENIC VS NON-CARDIOGENIC CAUSE OF PULM EDEMA
- Pt no s/s cough/infection/fever – Covid/pneumonia ruled out
- Lung US: POCUS showed: (on 10L O2):
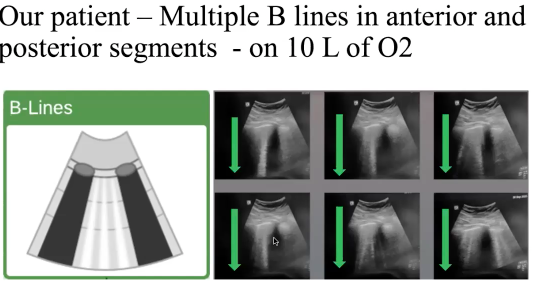
TTE/POCUS EXAM: Grossly normal Biventricular function from TTE, rest of POCUS exam unremarkable
- low suspicion for infectious process
- suspected diastolic dysfunction from preE & intolerance of fluid shifts —> pulm edema
- GAVE DIURESIS: Lasix
- ….1 hr later…REAL TIME resolution of pulm edema —> B lines turned into A lines.
- FHR Cat reading improved – fetus happier with better oxygenation.
- Proceeded to c/s with acute pulmonary process better managed –> reduced risk of cardiopulmonary complication.

Quick Youtube tutorials: INTRO on how to perform quick bedside lung US & Cardiac POCUS:
Video 12 Tutorial on lung ultrasound for pulmonary edema
Assessing Left Ventricular Ejection Fraction With Echocardiography
Introduction to Focused Cardiac Ultrasound: The Parasternal Long Axis View
Why incorporate more routine TTE In pregnancy?
- Immediate CV risk:
- Women who develop early-onset PreE requiring delivery < 34wks great significant r/o devel cardiac DIASTOLIC dysfunction up to 1yr after delivery (vs low-risk preg normotensive women) – TTE guides tx in pulmonary edema (ex: PPCM? diastolic dysfunction vs fluid overload – are inotropes needed?)
- Long term CV risk:
- Hx preE predisposes women to worse LV diastolic dysfunction, increasing the likelihood of later HFpEF development in the 5th decade of life (~20-30 years later!)
Pts with HTN disorders of pregnancy need more specialized attention – shown to have higher incidence of ICU-level care. More PreE w SF pts should probably have routine ECHO during pregnancy/antenatal. Especially considering long-term implications of CV risk later in life 2/2 PreE. BUT ESPECIALLY** IF THEY COME IN WITH PULMONARY EDEMA/ NEW SYMPTOMS OF CARDIOPULMONARY DYSFUNCTION!!