Adam Sachs MD 2018 HH Clinical Practice Reference: CPR.02.440
Introduction
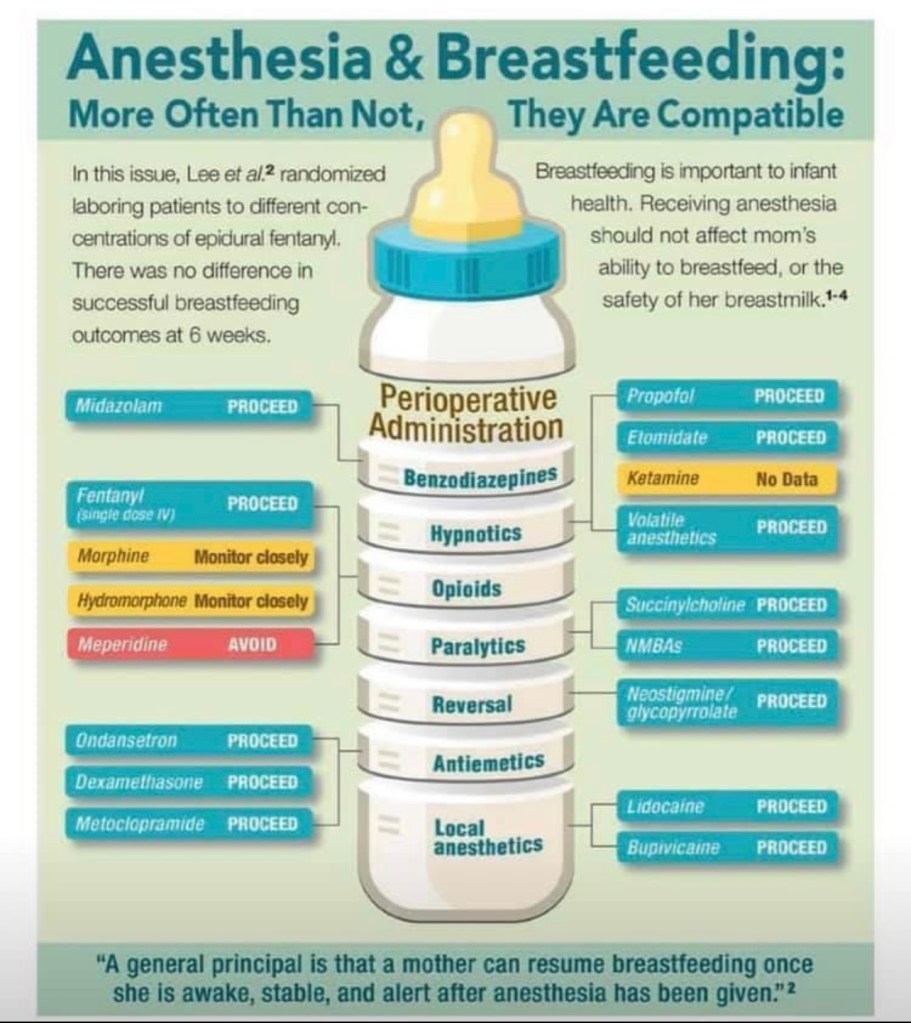
Because of ethical concerns, there is a general lack of information regarding the safety of breast feeding after anesthesia. Based on the available evidence, it appears that most anesthetic drugs administered to mothers are secreted into breast milk but the amount of drug absorbed by the infant is usually small. Ultimately, the amount of drug secreted into breast milk is determined by protein binding, lipid solubility, molecular weight, pKa, and maternal plasma levels. There is little information, and no evidence, that any anesthetic agent administered as a single-dose (typical dosage) is secreted in clinically significant amounts in the breast milk. Most anesthetics are cleared rapidly from the mother, and in almost all cases, it is permissible to allow breastfeeding as soon as practical after an anesthetic for surgery.
Commonly Used Anesthesia Medications
Primary IV Induction Agents
- Propofol
- low oral bioavailability, short duration of action, rapid metabolism and no active
metabolites, which make it an ideal induction agent. Two hours after induction, propofol
concentration in breast milk is negligible.
- low oral bioavailability, short duration of action, rapid metabolism and no active
- Etomidate
- rapid clearance in breast milk with small amounts still present 2 hours after
induction and undetectable amounts 4 hours after induction.
- rapid clearance in breast milk with small amounts still present 2 hours after
- Ketamine
- no available studies
Inhalational Agents
- Sevoflurane & Desflurane
- Rapidly excreted and have poor bioavailability, so it is typically considered safe for lactating women to resume breast feeding as soon as feasible.
Neuromuscular Blocking Agents
- Succinylcholine, Rocuronium & Vecuronium
- Large quaternary ammonium compounds, poor lipid solubility, and poor oral bioavailability make these drugs safe to be administered to breast feeding mothers.
Opioids
- Fentanyl, Hydromorphone & Morphine (IV)
- All secreted into breast milk in small amounts. For typical doses used during a surgical procedure, and in the PACU, it is generally safe for mothers to return to breastfeeding as soon as feasible. With exceptionally large, or repeated doses (high PCA doses), neonatal depression has been observed and a particular waiting period before resuming breast feeding should be considered based on the clinical scenario.
- Remifentanil
- Due to an ultra-short half-life, rapid metabolism by plasma cholinesterase, and high protein binding, it is considered safe for breastfeeding mothers although limited data exists.
Benzodiazepines
- Midazolam (Versed)
- Midazolam and its active metabolite hydroxymidazolam have a low milk/plasma ratio, low oral bioavailability, and short duration of action. A breast milk sample study showed that only 0.004% of Midazolam was secreted into breast milk over a 24-hour period. Furthermore, no adverse drug effects have been observed, although high or repeated clinical doses might be expected to exert a possible clinical effect on the newborn.
- Diazepam (Valium)
- Should be avoided if possible. See below
- Lorazepam (Ativan)
- Has a shorter half-life and no active metabolite when compared to
Diazepam. Preferred if a benzodiazepine, longer-acting than Midazolam, is needed.
- Has a shorter half-life and no active metabolite when compared to
Premature infants have a more permeable blood-brain barrier and impaired drug pharmokinetics. They are more likely to be affected by breast milk after maternally administered opioids and benzodiazepines. If premature infants receive breast milk from mothers who have received these types of medications, the infants must be observed for respiratory depression, apnea, cyanosis & bradycardia.
Reversal Agents
- Neostigmine and Pyridostigmine
- Safe because their concentration in breast milk is low, and GI absorption is minimal.
- Glycopyrrolate
- Not secreted into breast milk in significant concentrations
- Sugammadex (Bridion)
- Secreted into breast milk, but rodent data shows its probably safe
OTC meds
- Ibuprofen (Motrin) & Ketorolac (Toradol)
- Based on the available literature, and the American Academy of Pediatricians, ibuprofen and ketorolac are safe to administer to breastfeeding women.
- Acetaminophen (Tylenol)
- The transfer of acetaminophen into breast milk is low and considered safe for lactating mothers
USE WITH CAUTION in Breastfeeding Women
- Meperidine (Demerol)
- Has prolonged half-life in the newborn due to accumulation of an active metabolite, normeperidine, in maternal plasma and ultimately in breast milk. Infants exposed to meperidine in breast milk have been shown to be less alert and more poorly oriented compared with those who were exposed to morphine.
- Codeine
- Due to its variable conversion to Morphine by CYP2D6, it is best avoided as neonatal depression has been observed in babies with CYP2D6 abnormalities
- Diazepam (Valium)
- Administration has been shown to cause a prolonged presence of active metabolites in the newborn, due to slow infant elimination of the drug.
- Infants exposed to diazepam should be observed for sedation.
- Atropine
- can cause anticholinergic effects in the infant.
- Glycopyrrolate (as an alternative to atropine)
- does not cross into breast milk in any significant amount.