CONTENTS:
- Normal Uterine Vasculature Changes in Pregnancy
- HTN disorders of pregnancy
- Pre-eclampsia
- Eclampsia
- HELLP (Hemolysis, Elevated Liver, Low PLT)
- Gestational HTN
- NEURAXIAL PLACEMENT CONSIDERATIONS IN HTN pts
- HTN and PLT counts
- HELLP and coags
- Neuraxial sympathectomy in HTN OB pts
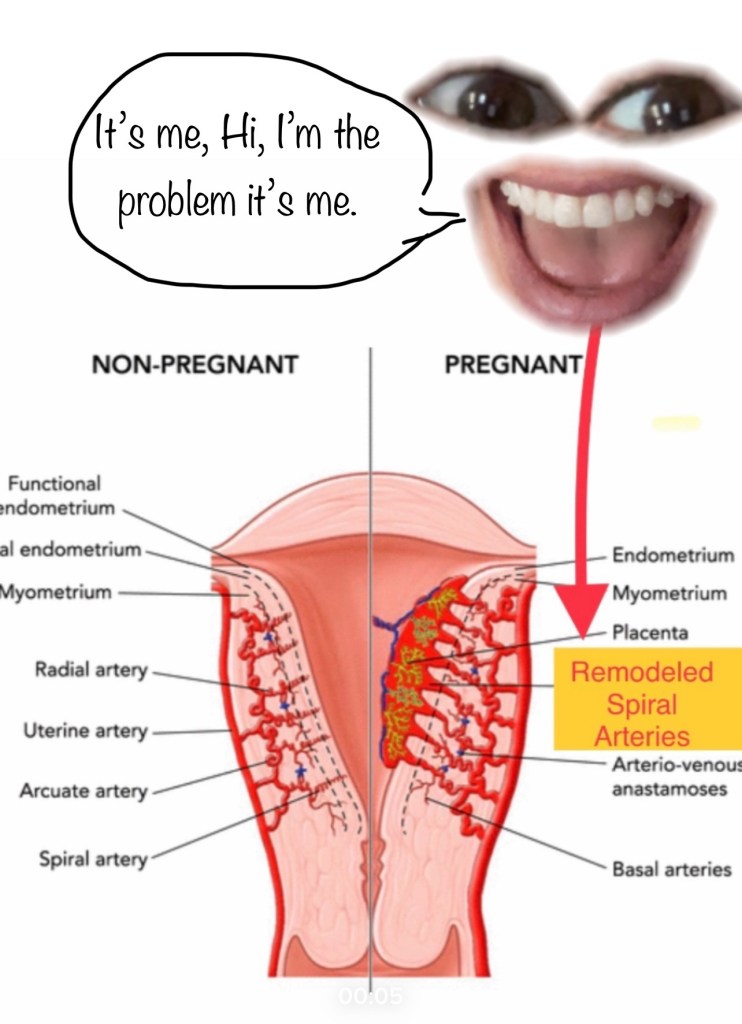
Normal Uterine Vasculature Changes in Pregnancy
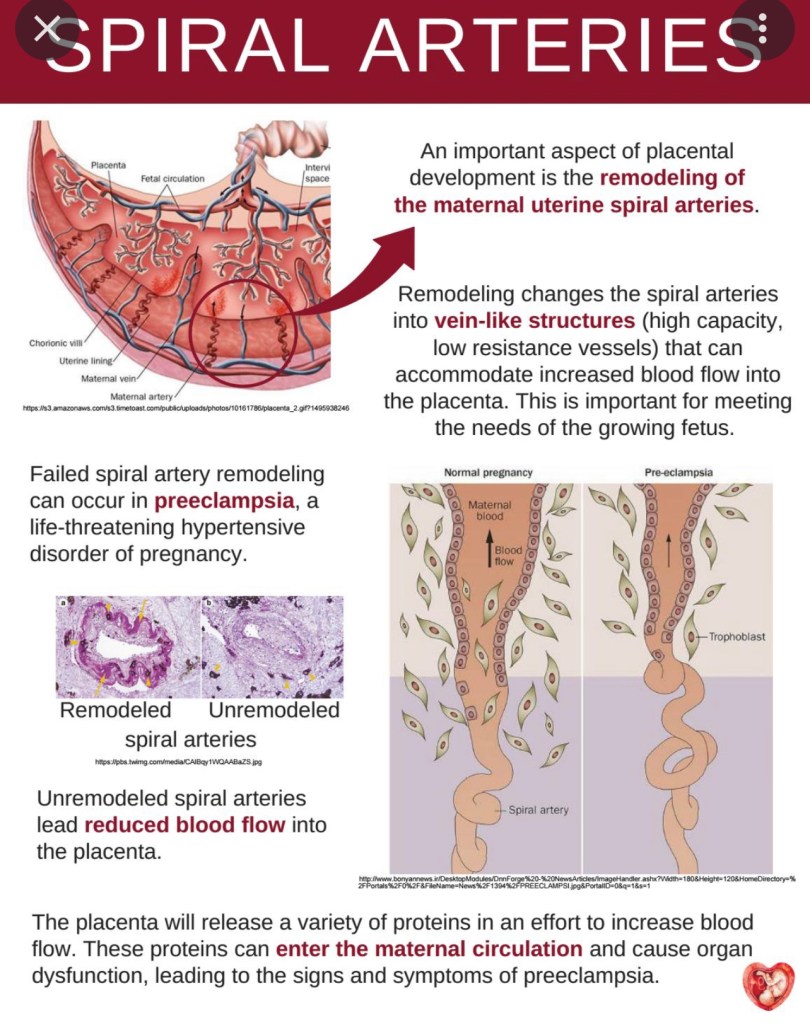
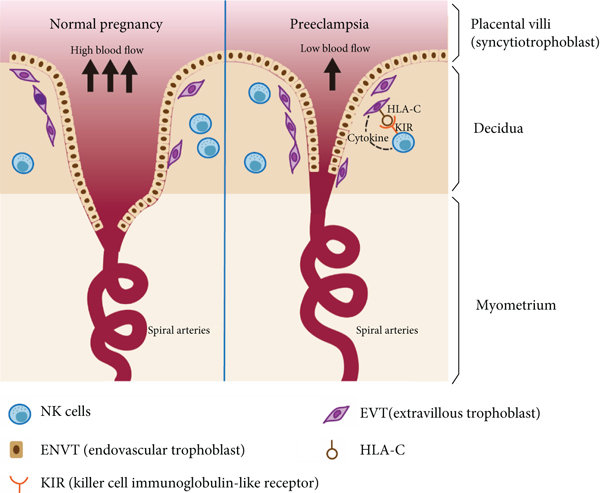
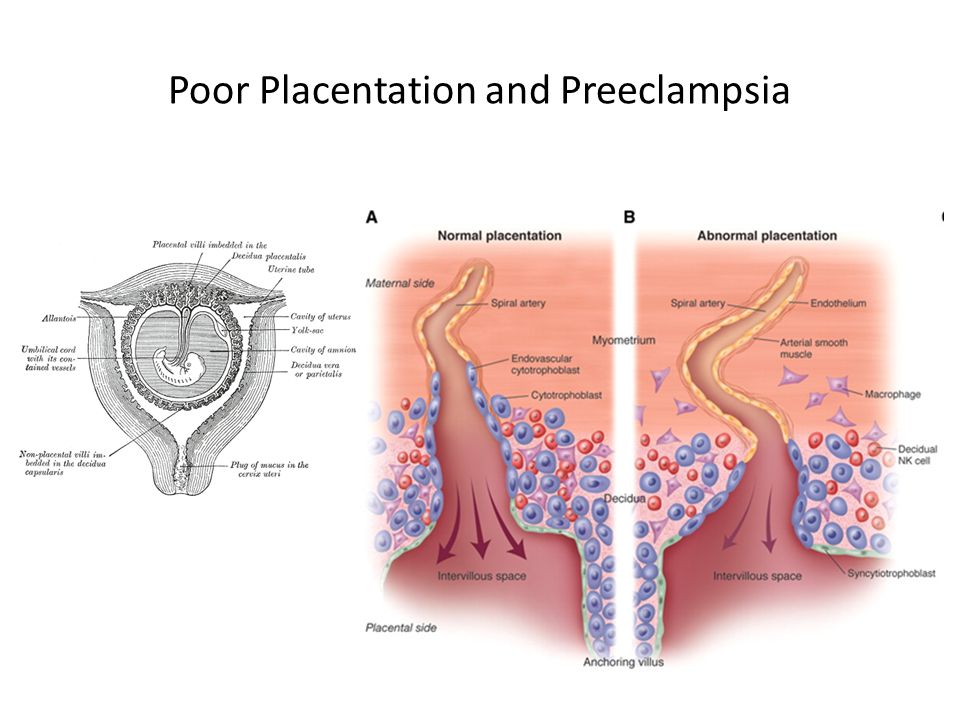
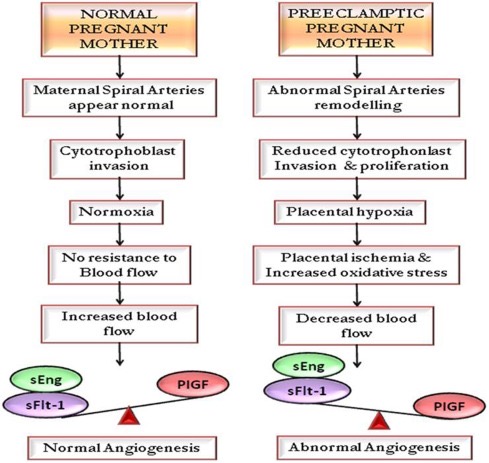
Normal Remodeling of Maternal UTERINE *SPIRAL* ARTERIES IS A CRITICAL COMPONENT OF NORMAL PLACENTATION AND ADEQUATE FETAL BLOOD FLOW AND OXYGENATION
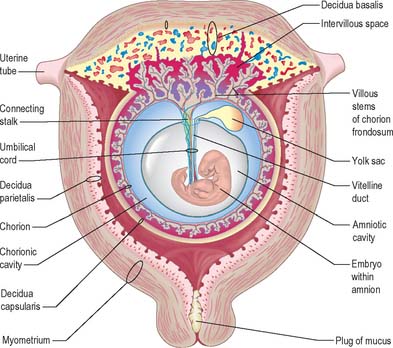
Normal Changes to Uterine Vasculature During Pregnancy
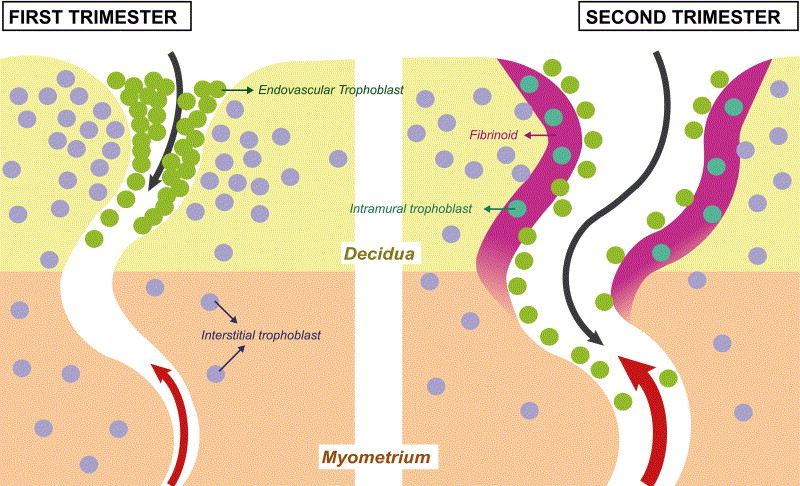
- Uterine spiral arteries, aka “utero-placental” arteries, run through decidua (aka endometrium when non-pregnant) to directly supply the placenta. During normal pregnancy, spiral artery vessel walls undergo radical structural transformation by trophoblasts to become wide open, high flow, low-resistance vessels to supply the placenta (with a ton of blood: 500-700cc/min by term)
- The key findings of physiologic transformation are:
- dilatation of the lumen
- trophoblast invasion of the vessel wall: media & endothelium
- replacement of muscular and elastic tissue of the arterial wall by a thick layer of fibrinoid material.
- The key findings of physiologic transformation are:
- These structural changes, especially the destruction of muscle in the media, would likely lead to loss in vasomotor control. Collectively, these changes maximize maternal blood flow to the intervillous space by making the arterial lumen wider and reducing the responsiveness to vasoconstrictor agents
- Spiral arteries are a distal branch of uterine radial arteries. Pitocin keeps these spiral arteries from bleeding by making the uterine muscle/myometrium contract and physically clamp down on/around the arteries supplying these wide-open spiral arteries:
NORMAL AND ABNORMAL TRANSFORMATION OF THE SPIRAL ARTERIES DURING PREGNANCY
HYPERTENSIVE DISORDERS OF PREGNANCY
Biggest risk of HTN disorders is maternal hypertensive crisis and stroke.
- Chronic = (cHTN) dx < 20 wks, or prior to pregnancy (NOT a pregnancy-related condition)
- Gestational HTN (gHTN), absent proteinuria/preE markers of end-organ damage
- Superimposed PreE on cHTN (SIPE)
- PreE w/wo severe features (SF): HTN >160/110, + Proteinuria, or another sign of end-organ damage
- Eclampsia
- HELLP (can also be normotensive/hypotensive)
HTN disorders of pregnancy all have theoretical causes but still definitively unknown.
HTN Diagnosis Timeline:
- PreE usually not diagnosed until after ~ 20wks, unless severe. Can be diagnosed up to 4 wks postpartum! (R/O postpartum PreE in PDPH workup – check BP.)
- Chronic HTN 0-20wks – usually diagnosed in office in early pregnancy.
- GHTN, preE, SIPE 20-38 wks
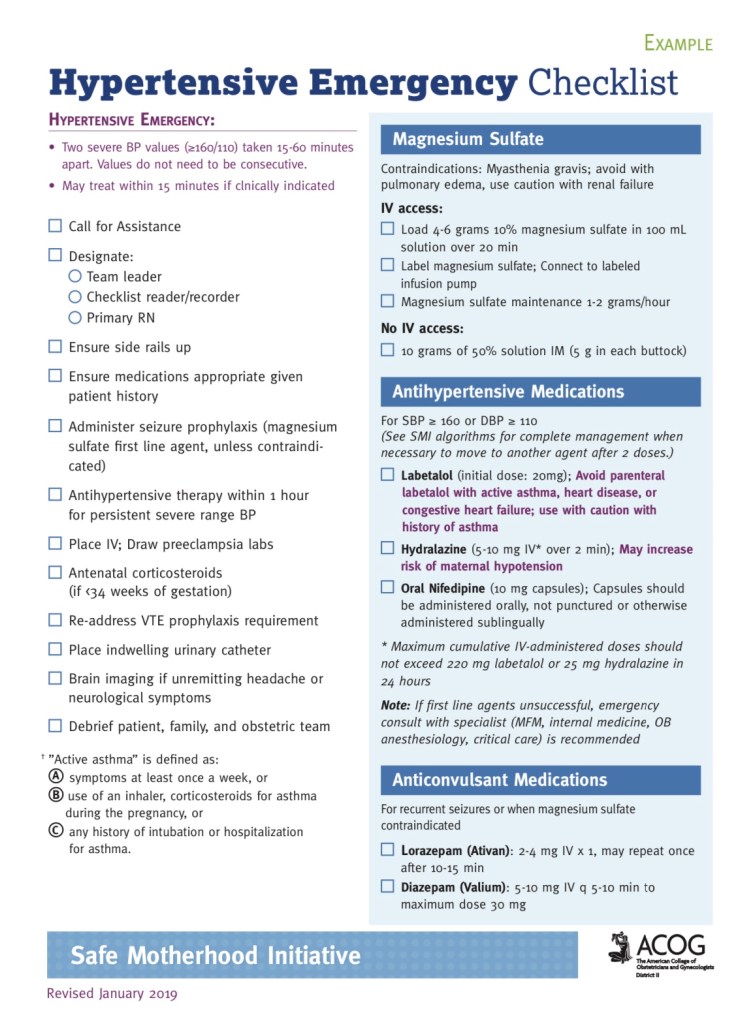
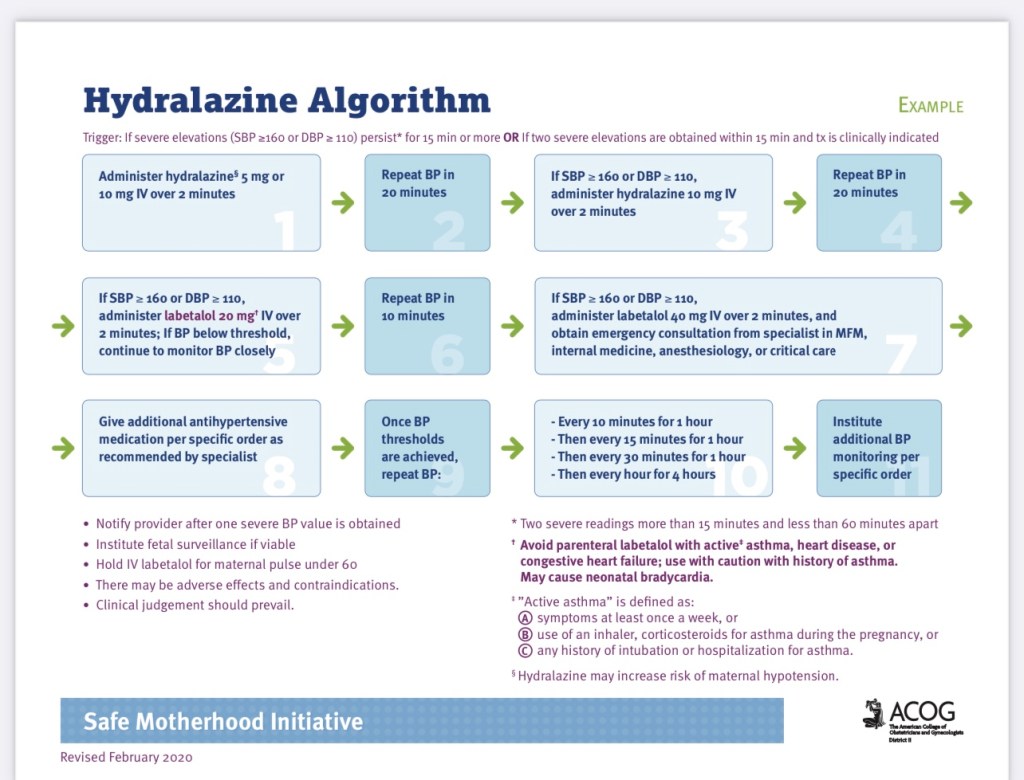
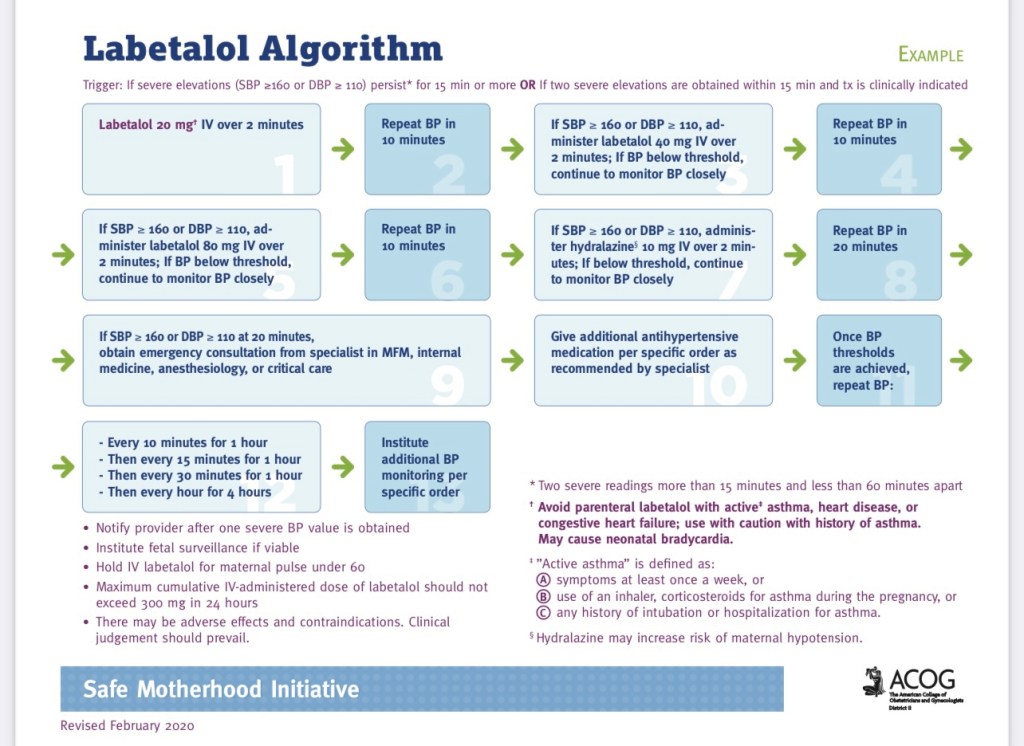
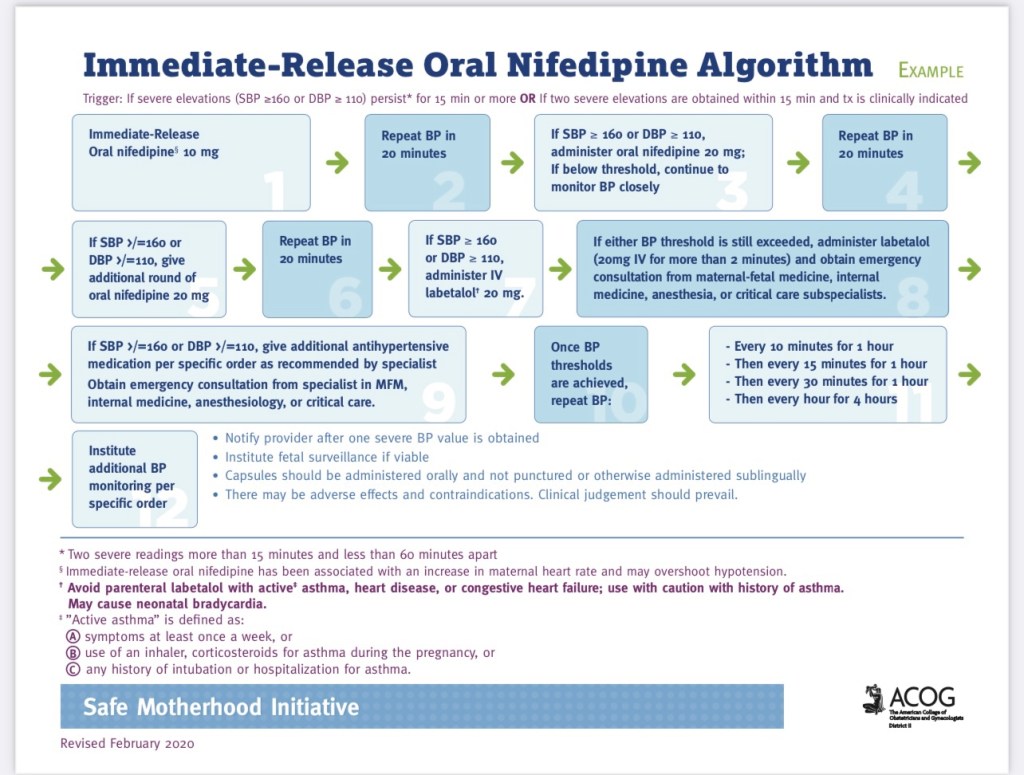
Hypertensive Emergency Algorithms
PREECLAMPSIA
PreE Diagnosis timing:
- EARLY: < 34 wks
- Placental implantation issue – usually more severe features, often urgent pre-term delivery necessary (c/s)
- LATE > 34 wks
- may be a metabolic issue : DM, HTN, obesity – may be less severe 🤞🏼
- SEVERE FEATURES (25%)
- HTN >160/110
- Proteinuria
- Elevated Liver enzymes, blurry vision, headache, HTN, oliguria, (quantity of proteinuria not indicitave of severity)
- ~ 1 in 10 pts with SF found to have HFpEF 2/2 diastolic dysfunction – SOB and pulmonary edema can be presenting signs, which can be precipitated by iatrogenic fluid overload.
SIGNS/SYMPTOMS for DX:
- HTN (SBP >140 mmHg or DBP >90 mmHg) AND 1 other sign of end-organ damage:(usually proteinuria bc it’s so quick and easy to test for with dipstick)
- AND proteinuria (1+ protein on urine dipstick, or >300 mg/24 hr, urine protein/creatinine ratio >0.3)
- OR thrombocytopenia (PLT <100,000)
- OR renal insufficiency (Cr >1.1 mg/dL or a doubled Cr absent other renal disease)
- OR impaired LFTs (AST & ALT elevated >2x normal limit, while Alk Phos is normally elevated in pregnancy)
- OR pulmonary edema
- OR cerebral, h/a or visual symptoms
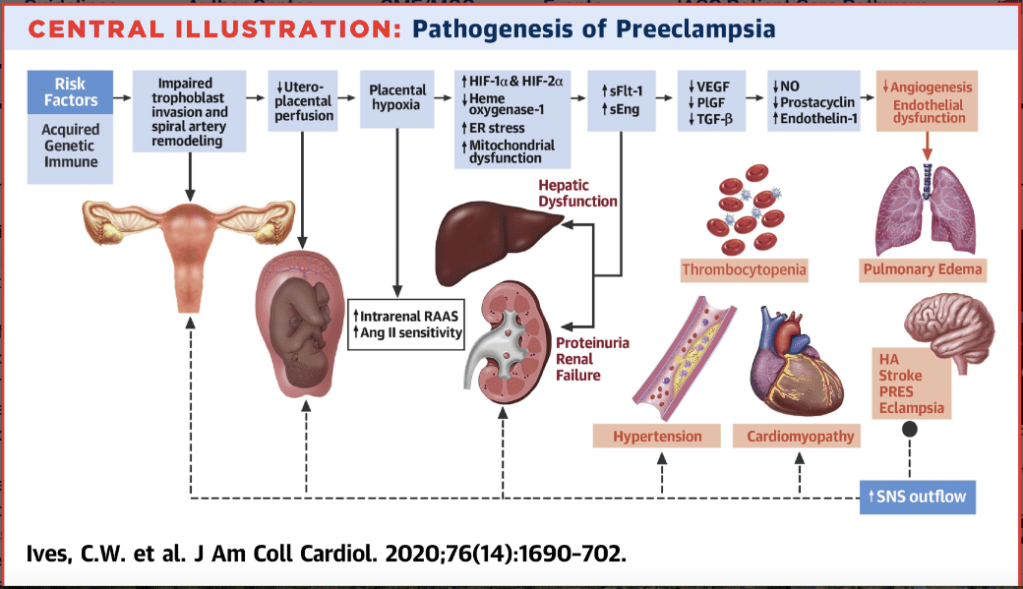
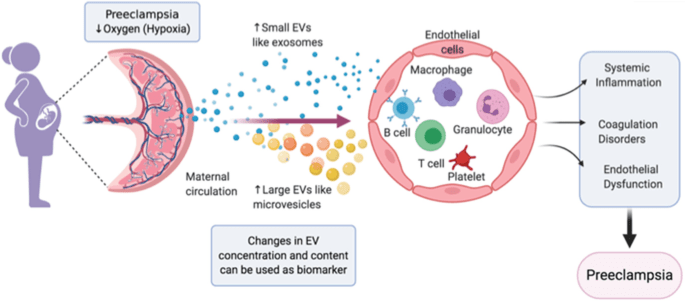
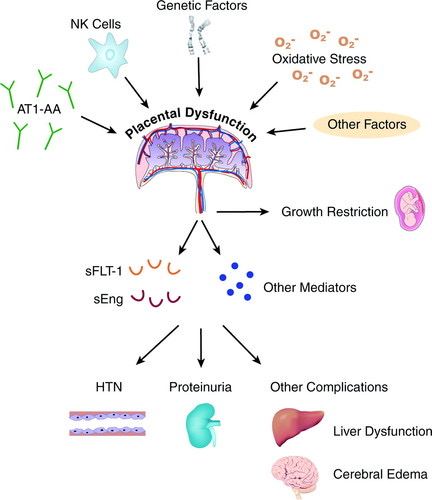
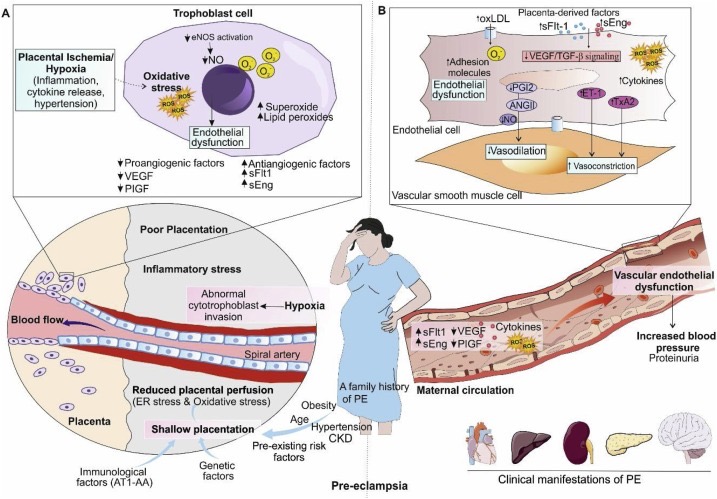
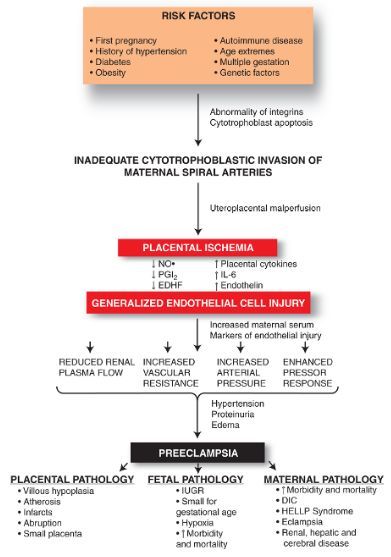
Etiology:
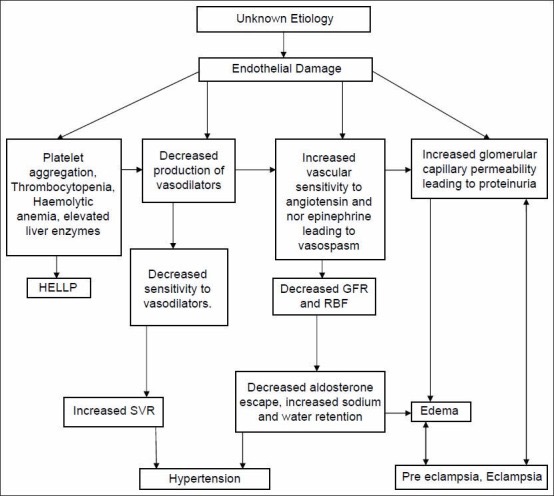
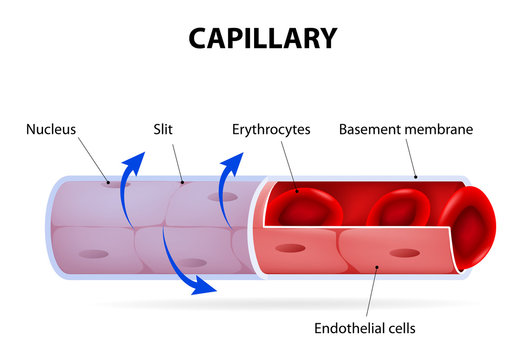
- Theory is inadequate, shallow uterine spiral artery remodeling. Spiral arteries unable to meet placental blood flow demands. Placenta is therefore under-perfused and releases inflammatory mediators into maternal bloodstream causing global endothelial dysfunction. ALL micro vasculature becomes inflamed, causing endothelial dysfunction, which causes end-organ damage and HTN.
- Endothelial damage causes:
- Endothelial inflammation – PLT activation & coagulation cascade activation
- Impaired vessel wall integrity and hydrostatic vs oncotic pressure imbalance
- Leads to increased edema, especially around airway!
- Nitric oxide release (local vasogenic mediator) also impaired —> HTN
- Vessels become hyper-responsive to RAAS Angiotensin2 (vasoconstrictor) —> HTN
- Endothelial damage causes:
- As fetus grows and needs more and more blood volume, the poorly-remodeled spiral arteries cannot deliver, and placenta releases more and more inflammatory mediators into maternal circulation. In this vicious cycle of increased inflammation causing increased HTN, PreE often gets worse and worse until delivery, and often women w/ severe features have to deliver early bc their end-organ damage/physiologic response is too severe to continue to term.
MATERNAL PHYSIOLOGIC CONSEQUENCES OF PRE-E:
- HTN:
- Underlying abnormalities:
- Increased SVR & afterload – diastolic dysfunction –> HFpEF in pts with severe features
- Decreased CO and intravascular volumes
- Activation of RAAS, ET-1, SNS
- AT1R down-regulated, placental hypoxia, and AT1R autoantibodies
- Increased vasoconstrictors (angiotensin2), decreased vasodilators(N.O.)
- Increased sFlt-1 and sEng, oxidative stress
- Clinical consequences:
- Heart failure**
- Pulmonary edema
- Renal dysfunction
- Neurological injury
- Underlying abnormalities:
- Neurologic Disturbances:
- Underlying abnormalities:
- Headache:
- loss of fenestrae on choroid plexus
- periventricular edema
- vasogenic edema in posterior cerebral circulation
- Visual disturbances:
- retinopathy
- retinal detachment
- cortical blindness
- central serous chorioretinopathy
- hypertensive retinopathy
- diabetic retinopathy
- Headache:
- Clinical consequences: Seizures, PRES, Permanent blindness
- Underlying abnormalities:
- Renal Dysfunction (proteinuria)
- Underlying abnormalities:
- Decreased RBF and GFR
- Glomerular endotheliosis
- Increased tissue factor expression
- Thrombotic microangiopathy
- Clinical consequences: HTN, CKD, ESRD
- Underlying abnormalities:
- Cardiac Dysfunction
- Underlying abnormalities:
- Increased SVR & afterload
- Concentric LV hypertrophy
- LA enlargement
- Increased RVSP & LV filling pressures
- LV diastolic dysfunction –> diastolic HFpEF, which can decompensate to HFrEF systolic heart failure
- Clinical consequences: Heart Failure, pulm edema
- Underlying abnormalities:
- Pulmonary Edema
- Underlying abnormalities:
- Increased vascular permeability
- Cardiac dysfunction
- Corticosteroids/tocolytics
- Iatrogenic volume overload
- Clinical consequence: Hypoxemic respiratory failure
- Underlying abnormalities:
- Hepatic Dysfunction
- Underlying abnormalities
- Hepatic microcirculatory deterioration
- Hepatocellular injury
- Clinical consequence: Liver failure, hepatic rupture
- Underlying abnormalities
- Hematologic dysfunction
- Underlying abnormalities:
- Procoagulant state –> consumption of factors/PLT
- Clinical consequences: Thrombocytopenia, DIC
- Underlying abnormalities:
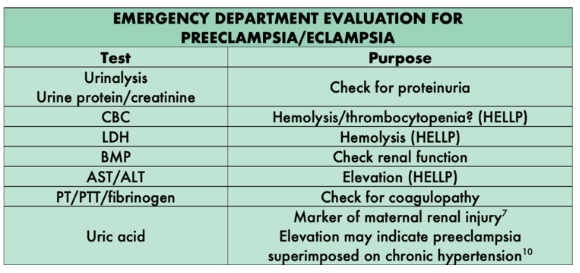
Preeclampsia—Pathophysiology and Clinical Presentations: JACC State-of-the-Art Review


Pts with HTN disorders of pregnancy need more specialized attention – shown to have higher incidence of ICU-level care, and higher incidence of heart failure and suatolic dysfunction. More PreE w SF pts should probably have ECHO during pregnancy/antenatal. PreE assc with disatolic dysfunction and impaired LV cardiac remodeling. Also considering long-term implications of CV disease risk later in life 2/2 PreE (see cardiac dysfunction page: diastolic dysfunction section.)
Maternal Cardiovascular Morbidity Events Following… : Anesthesia & Analgesia
Preeclampsia in the ED — Taming the SRU
ANESTHESIA CONSIDERATIONS FOR PreE:
PDF 2025 Anesthesiology Review of Periop Management of PreE:
- Consider coagulation status: CBC, liver function
- Consider uterine bleeding risk: MgSO4- contributes to uterine relaxation, methergine contraindicated in HTN while pre-term uterus may also be less responsive to oxytocin, thrombocytopenia/HELLP increases bleeding risk
- Swelling everywhere – ESP. AIRWAY.
- Function of normal increased vessel membrane permeability of pregnancy 2/2 increased plasma vol, total body water, and dillutional decrease in serum albumin *compounded even more by PreE- related increased membrane permeability from endothelial damage, and increased hydrostatic pressure from HTN (HTN 2/2 endothelial dysfunction impairing N.O. and increasing sensitivity to angiotensin 2)
- In HELLP – usually no neuraxial, PLT usually too low and compounded by liver dysfunction/coags dysfunction = GA if stat c/s = instrumenting swollen airway that may be more prone to bleeding with thrombocytopenia/disordered coags/liver dysfunction. Also, airway swelling can develop into a CICO situation – airway can swell shut with repeated instrumentation attempts with thrombocytopenia/disordered coags/liver dysfunction. (glidescope should always be used – more gentle intubation with swollen tissues, as well as greater first pass success)
- PreE s/s get progressively worse & worse until delivery.
- Risk of inflammation (injured endothelium)-mediated PLT activation & consumption—> thrombocytopenia.*
- Thrombocytopenia is indicator of end-organ damage 2/2 systemic microvasculature injury
- PLT trended Q6hrs in PreE w/SF (per HH policy). If precipitous PLT drops, can be trended more frequently. ACOG/ASA/SOAP/NYSORA: PLT > 70k for Neuraxial
- If coags do not support neuraxial —> GA, but VERY swollen airway possible.
- If PLT 70-100K, and have been trending down/dropping precipitously, can always add coags/TEG to be extra cautious – esp if elevated LFTs.(*AST&ALT. Alk phos elevation is a normal finding in pregnancy) But best to get labs as close as possible to neuraxial placement.
- PreE pts are intravascularly dry 2/2 third spacing [(2/2 endothelial damage impairing vascular membrane permeability.) HTN maintained as endothelial damage increases response to Angiotensin 2 and decreasing nitric oxide release] = tight, dry vessels.
- This can cause exaggerated HOTN response to vasodilation from neuraxial sympathectomy ––> *esp if BBs used (labetalol is a 1st line anti-HTN for PReE) as now they cannot mount a tachycardic response to decreased preload/SV from sympathectomy-mediated vasodilation to maintain CO. This HOTN can cause FHR late decelerations as MAP-dependent placental perfusion is decreased.
- Slow-dosed epidural is ideal, or pressor (phenylephrine or levo) gtt for surgical-level block
- The answer is NOT to fluid overload them- they have high risk of pulm edema: increased endothelial permeability from damage 2/2 preE, Mag increases risk of pulmonary edema 2/2 cardiac depression and possible endothelial injury, and preE is assc with diastolic dysfunction. Pulm edema risk is especially right after delivery when CO doubles and uterine autotransfusion provided ~750cc bolus.
- Just be cognizant of giving gentle, slower, more dilute epidural dosing, dilute top-offs focusing on volume spread vs concentration, and careful consideration of neuraxial sympathectomy speed and density. Even labor CSE small intrathecal dose might drop their pressure too quickly.
- The answer is NOT to fluid overload them- they have high risk of pulm edema: increased endothelial permeability from damage 2/2 preE, Mag increases risk of pulmonary edema 2/2 cardiac depression and possible endothelial injury, and preE is assc with diastolic dysfunction. Pulm edema risk is especially right after delivery when CO doubles and uterine autotransfusion provided ~750cc bolus.
- Slow-dosed epidural is ideal, or pressor (phenylephrine or levo) gtt for surgical-level block
- This can cause exaggerated HOTN response to vasodilation from neuraxial sympathectomy ––> *esp if BBs used (labetalol is a 1st line anti-HTN for PReE) as now they cannot mount a tachycardic response to decreased preload/SV from sympathectomy-mediated vasodilation to maintain CO. This HOTN can cause FHR late decelerations as MAP-dependent placental perfusion is decreased.
- Maintain uteroplacental perfusion pressure (MAP-dependent).
- Sympathectomy from neuraxial anesthesia managed with neo gtt if C/S under neuraxial anesthesia. For labor epidurals – give 3cc test dose, and a small ~5-6cc loading dose to minimize sympathectomy – can dilate space with saline to dilute loading dose and improve medication spread.
- PreE can cause diastolic dysfunction
- So although they’re often intravascularly dry from the third spacing, do not fluid overload this pt because they are at higher risk of pulm edema. Maintain BP with neo gtt prior to delivery, not fluid boluses. Autotransfusion after delivery & fluid shifts should restore intravascular hypovolemia to some degree. Fluid overload with diastolic dysfunction can cause flash pulmonary edema.
- If questioning fluid overload or fragile cardiac C/S pt – can ask OBGYN to give IU pitocin instead of us giving the usual 10unit/~166cc rapid IV bolus. Then just run 5u/hr normal gtt 83.3mL/hr after delivery.
- Azithromycin can be mixed in 20cc syringe and given slowly 1cc at a time throughout case over ~90 min (instead of 250cc bag)
- Higher risk pulm edema:
- esp in SIPE and CKD(Bun/Cr) – if flash pulm edema in HTN pt: lasix, and nitro to decrease preload. (Management covered in Pulmonary Edema ipage: different tx for HTN vs HOTN pulm edema)
- Higher risk of hemorrhage and DIC:
- – Hemorrhage risk 2/2 atony from uterine relaxant effects of magnesium gtt (MgSO4 given to prevent eclampsia seizures if preE progresses. Mag gtt is still continued through labor and c/s despite uterine relaxant effects)
- – DIC risk from PLT consumption. The inflammation of PreE is constantly consuming PLTs before there’s even an actual hemorrhage, so these patients are basically playing with half a deck if they start bleeding.
- HTN Management: Labetalol, Hydralazine, nifedipine nicardipine, esmolol.
- Reminder about labetalol in asthmatics. (commonly given in OB to control HTN – more commonly given to asthmatics than hemabate, but both cause potential bronchoconstriction/status asthmaticus.
- BBs may also impair baroreceptive response to neuraxial – keep BP tight with neo gtt
- Reminder about labetalol in asthmatics. (commonly given in OB to control HTN – more commonly given to asthmatics than hemabate, but both cause potential bronchoconstriction/status asthmaticus.
LABOR ANALGESIA in PreE
- Better to get epidural in early before PLT drops further, and before airway & interstitial swelling keeps increasing. An epidural is your lifeline to avoid GA for a stat C/S with no epidural.
- and c/s more likely 2/2 fetal intolerance of labor given poor uteroplacental vasculature
- Labor CSE may be questionable in preE
- Higher chance of C/S and ++ airway edema means a PROVEN epidural catheter is needed to avoid GA/airway instrumentation.
- Rapid sympathectomy from intrathecal LA in CSE is inappropriate in intravascularly dry HTN pt. Although labor CSE dose is very small, there is still a faster onset to sympathectomy than a regular epidural dose, giving less time for compensation.
- MAINTAIN MAP (placental perfusion): gentle, slower onset to epidural block.
- Sympathectomy = decreased MAP = decreased fetal perfusion —> decels/fetal acidosis —> stat c/s.
- Can dilate space well w saline still & give smaller loading bolus dose ~ 6cc vs 10cc and saline should help spread the LA (personally I’m *all about* dilating w saline to improve block spread – esp of giving a lower-volume loading dose.)
- *3 cc test dose with these HTN pts, not 5cc (less lido = less sympathectomy)
- Top-offs should be larger volume with more dilute concentration to encourage spread and avoid profound sympathectomy.
ACOG Practice Bulletin on PreE & gHTN:
Gestational Hypertension and Preeclampsia
Online Lecture:
Expectant Management of the Patient with Preeclampsia – OpenAnesthesia
Vasopressor Use in Obstetrics: Past, Present, and Future – OpenAnesthesia
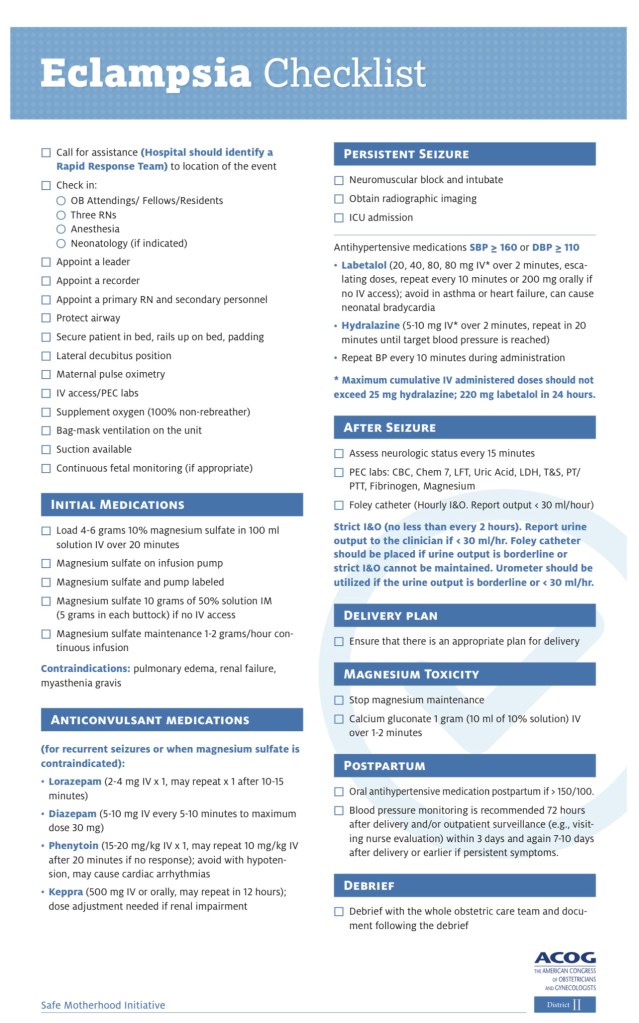
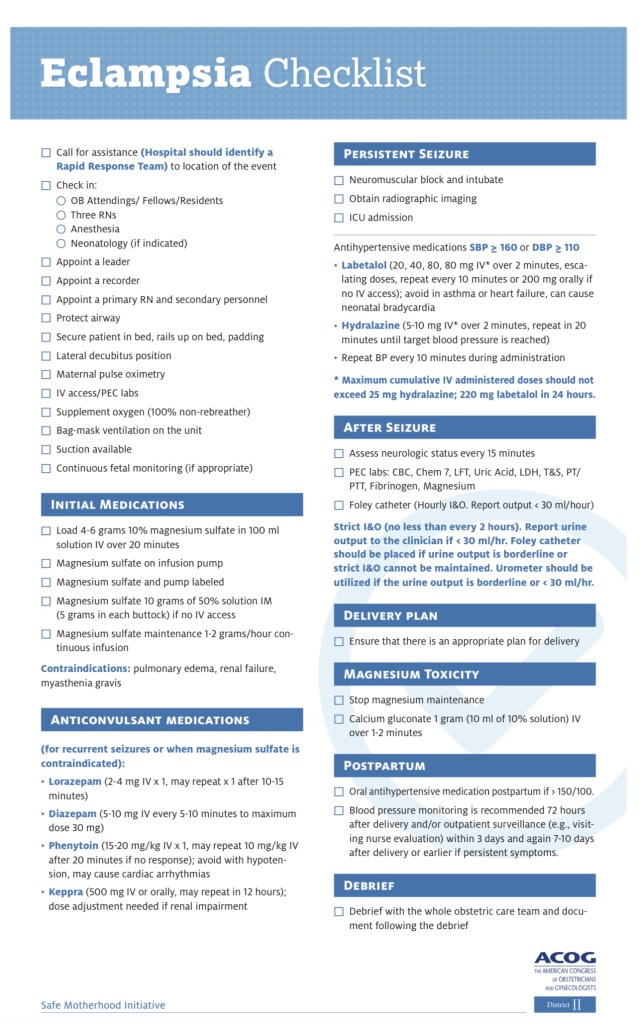
ECLAMPSIA
SEIZURE MANAGEMENT
PREVENT ASPIRATION
4g MANGESUIM SULFATE IV bolus, then 1-2mg/hr gtt
Benzodiazepines to break seizure.
If airway compromise –> EXPECT ++AIRWAY EDEMA. Intubation: RSI with succs & propofol. Propofol push may break seizure as well, but airway/apnea/aspiration risk requires intubation in pregnant airway. (Considered full stomach up to 72h post-partum)
BLOOD PRESSURE CONTROL if > 160 SBP or 110 DBP:
ANESTHESIA MANAGEMENT in ECLAMPSIA
- Differential dx: epilepsy, cerebral infarction, cerebral hemorrhage, SAH, cerebral venous thrombosis, cerebral edema, malignant HTN, benign & malignant cerebral tumors, cerebral abscess, viral, bacterial, parasitic infestations, hyponatremia, hypocalcemia, hypoglycemia, and hyperglycemia.
- BP control with IV Labetalol (20, 40, 80 mg dose, max 220mg total) , IV Nicardipine, IV Hydralazine, Nifedipine is PO.
- Avoid Labetalol is asthmatics.
- Avoid ACE-I, Spironolactone in pregnancy.
- Exaggerated HTN response to intubation can be expected – –> IV anti-HTN meds.
- Magnesium will potentiate NMBDs
- DO NOT FLUID OVERLOAD – Needs fluid restriction.
- DRAW: CHEM, LFTs, CBC, and COAGS: regardless of PLT count: +/- possible TEG. Liver dysfunction highly possible, and coag factor dysfunction possible.
Anesthetic management of a patient presenting with eclampsia
Eclampsia and Role of Magnesium Sulfate
Magnesium Sulfate
- Mag is NOT for BP control. It’s for seizure prevention.
- Adverse effects: muscle weakness leading to respiratory paralysis and failure (careful emerging in GA, Mag causes extra muscle relaxation) then progresses to cardiac arrest as hypoxia worsens and myocardial conduction fails.
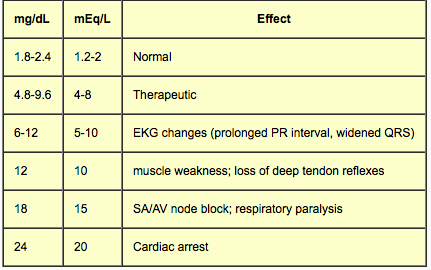
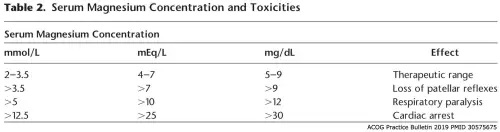
- Toxicity: 6-9mg/dL is therapeutic. If DTRs intact, resp failure is not from Mag — seek another cause.
Mag Toxicity Reversal:
- 10 mL of 10% (1g calcium gluconate IV over 3 min (slowly) to avoid HOTN and/or bradycardia)
- Ca++ competitively inhibits Mag at NMJ, but can wear off if Mag level stays high
- Furosemide may help increase urinary excretion
- Ca++ gluconate = 1/3 potency of CaCl.
HELLP
Pre-E vs HELLP:
- PreE comes in mild-severe cases, whereas HELLP is ALWAYS severe, ALWAYS an emergency.
- Is preE —> HELLP a continuum or separate etiologies? Unclear
- HELLP has long been considered a severe form of preE but HTN isn’t necessarily part of the diagnosis.
- PreE & Eclampsia however do retain HTN in diagnostic s/s.
- HELLP has 20/30% risk of DIC
- HELLP is an EMERGENT condition.
H: Hemolysis
EL: Elevated Liver (enzymes)
LP: Low Platelets
H: Hemolysis
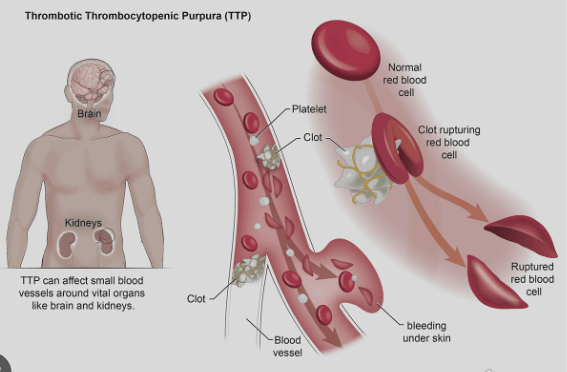
- As systemic inflammation of microvasculature activates PLTs—> activates coag cascade —> forms PLT plugs and then tiny fibrin clots along the microvascular endothelium, the RBCs floating through these micro vessels get damaged/sheared from scraping along these hardened fibrin clots
- LAB FINDINGS:
- “Schistocytes” on peripheral blood smear = little sheared rbc fragments/damaged rbcs
- Schistocytes indicate profound widespread microangiopathic thrombosis and is considered a hematologic emergency.
- (HELLP, hemolytic anemia, TTP, HUS)
- Schistocytes indicate profound widespread microangiopathic thrombosis and is considered a hematologic emergency.
- Elevated Billirubin 2/2 increased hemoglobin catabolism > 1.2mg
- Lactate dehydrogenase (LDH) released from RBCs into plasma from RBC breakdown (normal ~140-280 u/L, hemolysis dx > 600 u/L)
- Elevated ALS/AST (normal ~8-50 u/L, elevated > 70 IU/L)
- Thrombocytopenia < 100K from consumption
- Serum haptoglobin decreases < 40 mg/dL (normal 40-200)
- binds free hemoglobin from lysed RBCs – gets rapidly consumed in hemolytic states
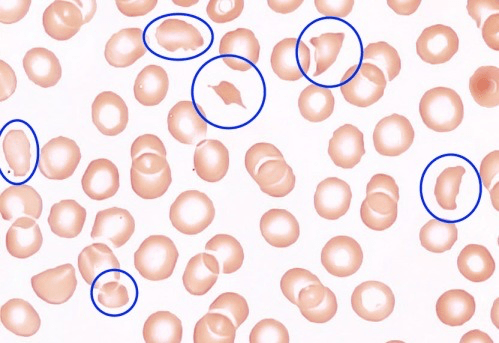
Schistocytes on the Peripheral Blood Smear
EL: Elevated Liver
- only alk phos is normally elevated in pregnancy
- PreE pt w/ ^^^ liver transaminases (AST, ALT) lactate dehydrogenase (LDH), & uric acid might be progressing to HELLP.
- High AST & ALT, bilirubin, and LDH
- Liver transaminases typically > 500 U/L in HELLP. (Much higher in HELLP than preE. PreE may see only a 2-3x increase in severe cases)
Preeclampsia‐induced Liver Dysfunction, HELLP syndrome, and acute fatty liver of pregnancy
Preeclampsia‐induced Liver Dysfunction, HELLP syndrome, and acute fatty liver of pregnancy
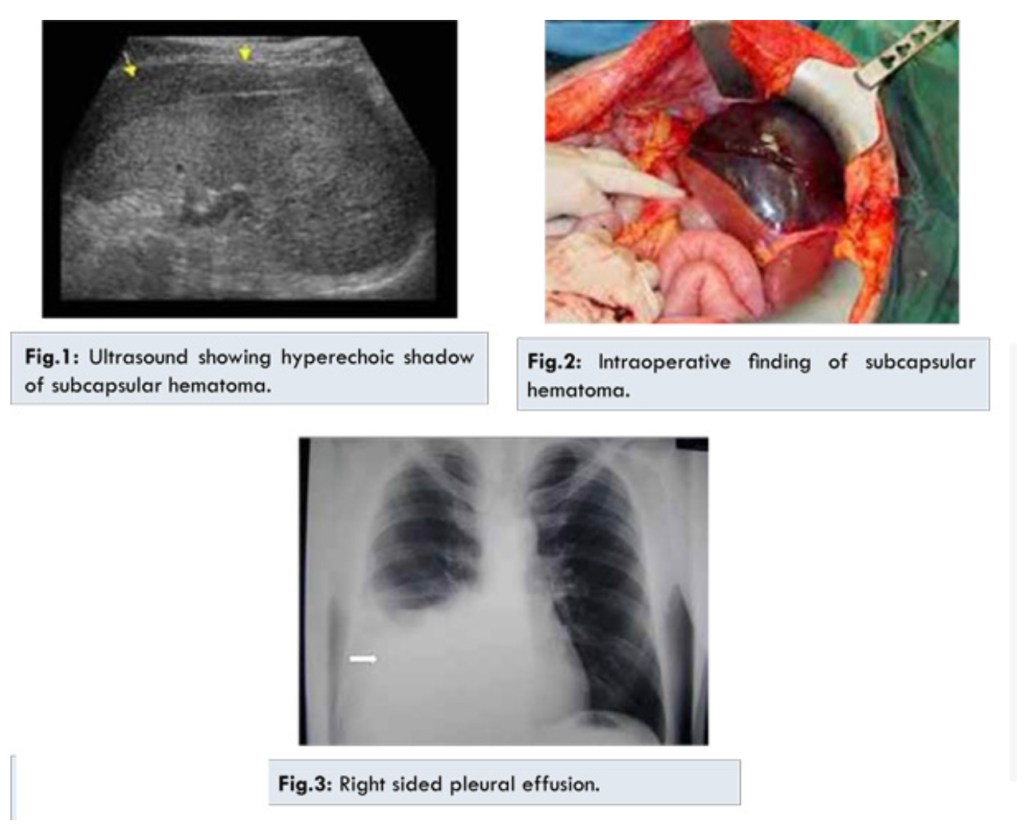
HELLP Fatal Liver complication: Glisson’s Capsule Rupture:
- HELLP & PreE can have liver subcapsular hematoma and rupture (fatal). Pt c/o Upper Right Quadrant pain needs workup.
- Patients with subcapsular hepatic hematoma typically present with epigastric, right upper quadrant or shoulder pain, nausea and vomiting, and/or shortness of breath.
Hepatic Rupture Complicating HELLP Syndrome in Pregnancy
Two Cases of Severe Preeclampsia Were Diagnosed with HELLP Postpartum after Caesarian Section
LP: Low PLT: THROMBOCYTOPENIA
2/2 PLT activation and consumption.
PreE can have low PLT, which we trend Q6h, but in HELLP it’s literally part of the diagnosis – they’re already low when diagnosed.
- This can often mean no labor epidurals and GA is the only method of operative delivery..…..Which sucks bc the airway is often swollen AF and you can easily cause airway bleeding.
HELLP Syndrome – StatPearls – NCBI Bookshelf
Neuraxial HELLP Considerations:
- RAPID, continuous drop in PLT. at least Q6h, or as close to epidural/neuraxial placement as possible. High Risk DIC (20-30%)
- May need TEG too bc PLT themselves can be dysfunctional, even if > 70-100k.
- Check PLT and coags (fibrinogen) before removing epidural catheter. – repeat coags and TEG may be appropriate as well, to better assess coagulation status.
GESTATIONAL HTN
- GHTN may be a function of volume overload on top of chronic subclinical HTN. It doesn’t involve the proteinuria and end-organ damage markers of preE, suggesting there isn’t the same endothelial dysfunction, suggesting it doesn’t have to do with placental ischemia and inflammatory mediators.
- Still has higher baseline BP = higher MAP perfusing fetus, so still needs tight BP control with neuraxial sympathectomy.
- THROMBOCYTOPENIA POSSIBLE: PLT count still monitored/trended. Thrombocytopenia from gHTN may be dilutional?? Unknown cause. Doesn’t usually have precipitous drops like PreE, HELLP, or other thrombocytopenias
- if PLTs stable, then no need to trend Q6h(like we do with preE). QD is enough.
Resources/reviews re: PreE/HTN
GHTN Cause unknown:
Hypertrophic decidual vasculopathy
Episode 162: Hypertensive Disorders of Pregnancy with Juanita Henao
Regulation of Uterine Spiral Artery Remodeling: a Review – Reproductive Sciences
Spiral Artery Remodeling and Trophoblast Invasion in Preeclampsia and Fetal Growth Restriction
NORMAL AND ABNORMAL TRANSFORMATION OF THE SPIRAL ARTERIES DURING PREGNANCY
The trophoblast plug during early pregnancy: a deeper insight
HTN in Pregnancy & Monitoring PLTs for Neuraxial
Thrombocytopenia is a sign of end-organ damage in PreE and HELLP, as damaged endothelium is activating PLTs and the clotting cascade. Thrombocytopenia signals severity of disease process, and can progress as inflammation worsens with longer gestation.
PreE/SIPE:
- Q6 PLT draw is hospital policy.
HELLP:
- Usually not candidates for Neuraxial once diagnosis is made, considering liver dysfunction and Low PLT are part of the diagnosis, and will continue to worsen until delivery.
- Liver dysfunction can cause additional coagulopathy on top of thrombocytopenia.
- High risk of DIC. Q6h PLT, plus coags/TEG if bleeding concerns. These are usually GA for C/S if no neuraxial in place prior to diagnosis.
- HELLP-induced laboratory derangements usually improve by 72 hrs after delivery, though longer resolution, especially with transaminases, can be seen up to several weeks postpartum
- PLT counts often recover within a day or so after delivery if epidural catheter is in pace waiting to be pulled – recheck CBC/PLT count postpartum.
Liver dysfunction:
- Q6 PLT AND coags/TEG prior to neuraxial. Will be GA if c/s required and neuraxial deemed unsafe.
- Acute Fatty Liver of Pregnancy is high risk of DIC (80-100%) – Neuraxial should not be performed!
GHTN:
- Just one daily normal PLT is ok, no need for Q6H monitoring. No signs of end organ damage – This is may be partly due to fluid overload and dilutional thrombocytopenia, rather than damaged-endothelium-mediated PLT activation and consumption of preE/HELLP.
CHTN:
- Just one normal PLT on admission is OK. without dx of PreE or GHTN, there is no need for additional PLT trending.