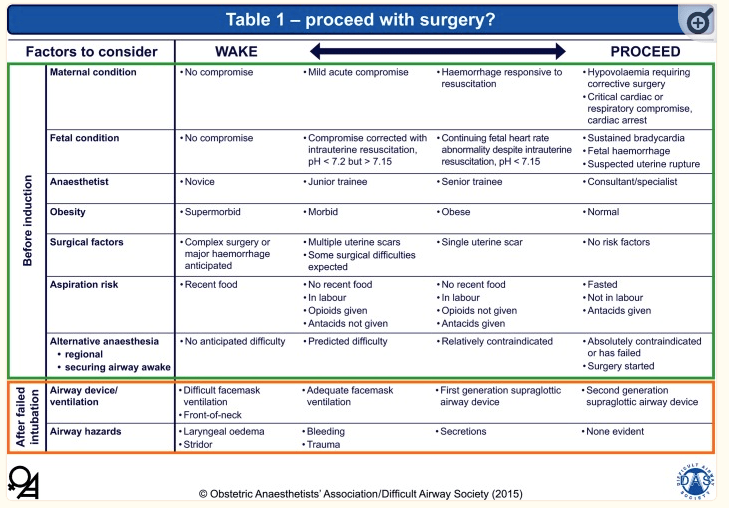
PLAN THROUGH TO THE FINAL DECISION OF: In event of failed airway, are we: WAKING HER UP, OR PROCEEDING NO MATTER WHAT, FOR EACH PATIENT
Serious airway problems have occurred in pregnant women during recovery from GA. If there have been multiple intubation attempts or signs of airway edema at laryngoscopy, there is a potential for SERIOUS airway problems after extubation. The cuff of the tracheal tube should be deflated before extubation and a leak around the tube confirmed before its removal. Extubation in all obstetric patients should be AWAKE.
- ** L&D pacu nurses may not be as accustomed to airway obstruction management as Main OR pacu nurses who often have ICU experience, are used to GA recovery, and usually deal with much sicker/more complicated post-op patients. Make sure patient will be ok for L&D pacu as the pts FRC is still decreased, and 02 demands are increased postpartum, leading to rapid desaturation with airway obstruction.
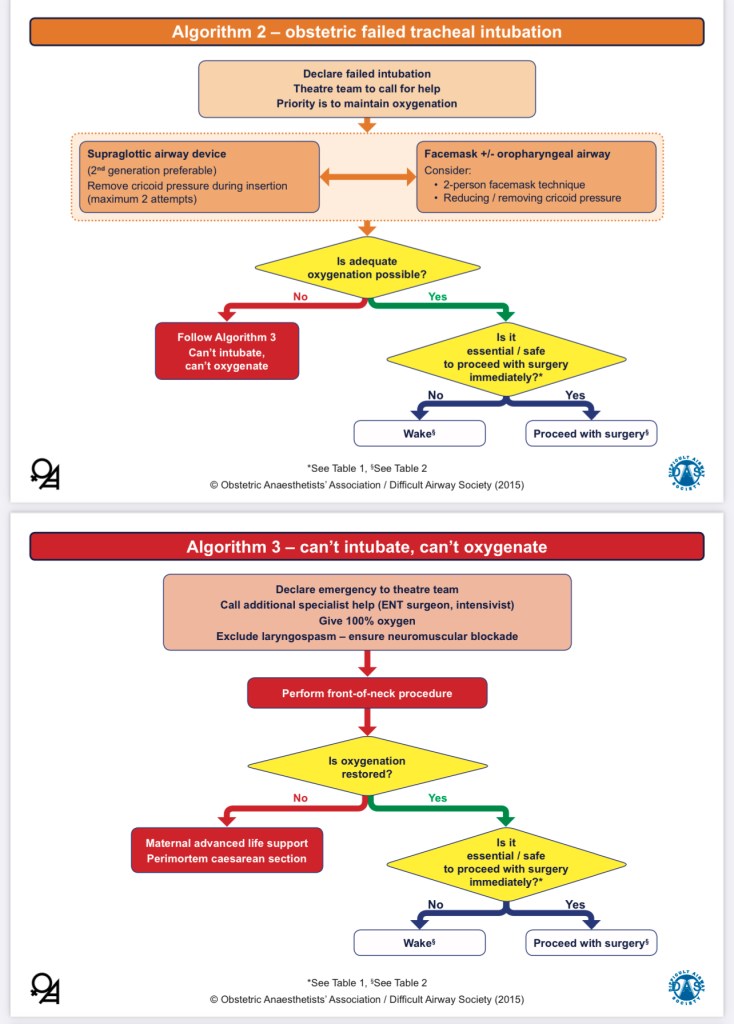
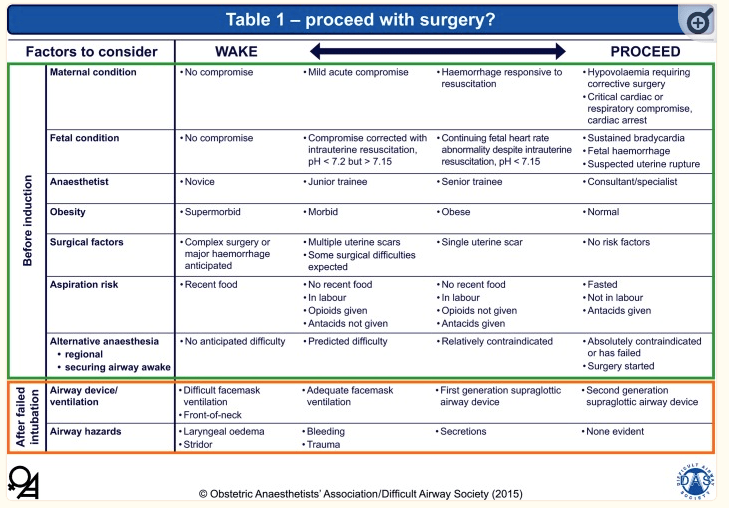
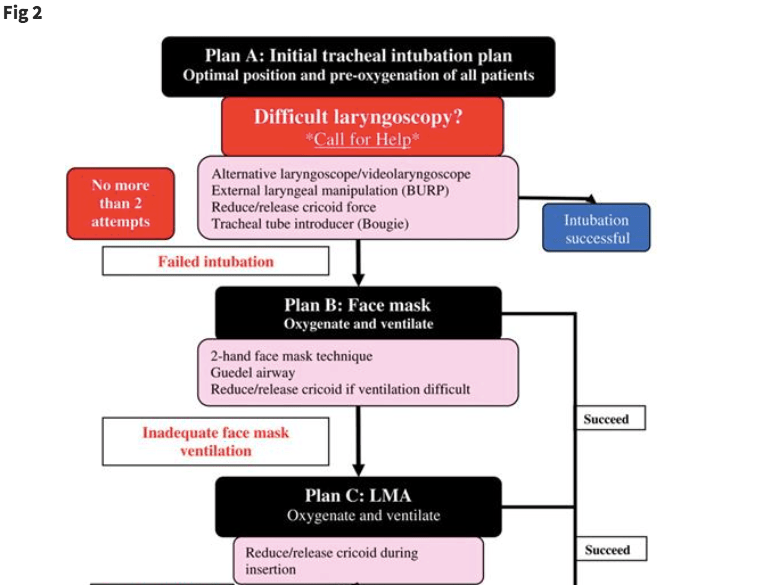
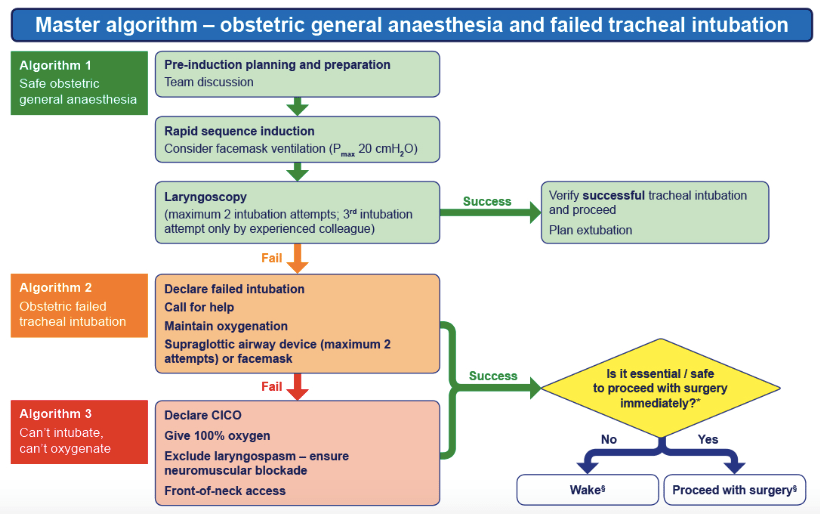
AIRWAY ALGORITHMS
ASA Adult Difficult Airway Algorithm VS Obstetric Anesthetists Society/Difficult Airway Society OB Difficult Airway Algorithm:
ASA:

Obstetric Anesthetists Society/Difficult Airway Society OB Difficult Airway Algorithm:

DIFFICULT AIRWAYS IN OB
- Incidence of failed intubation in OB reported to be around 1:300
- GA generally only used in emergent situations, where urgency and stress can add to difficulty of airway management in high-risk patient:
- Urgency may compromise: pt positioning, airway assessment, and pre-oxygenation.
- (aka sometimes we panic, don’t optimize the airway, and shoot ourselves in the foot, making a high-risk airway now even more difficult)
- Urgency may compromise: pt positioning, airway assessment, and pre-oxygenation.
- Most patients who are impossible to intubate can still be ventilated:
- So prediction of impossible mask ventilation is valuable.
- Independent predictors of impossible mask ventilation in adult general population were:
- neck radiation changes, OSA, male sex, Mallampati 3-4, & beards.
- RE: OBSTETRICS: Mallampati 3+, and OSA independent predictors of impossible mask ventialtion.
- Independent predictors of impossible mask ventilation in adult general population were:
- So prediction of impossible mask ventilation is valuable.
WHY GA?
- NEURAXIAL ALWAYS BEST if no contraindications, but TIME-SENSITIVE nature of fetal distress or neuraxial contraindications May warrant GA.
- GA with RSI is fastest an acutely compromised fetus, may save 8+ min (over awake fiberoptic) and 5+ min (over spinal).
- Obstetric Difficult Airway Algorithms are a compromise of speed versus safe progression through a number of logistic steps.
- Urgency in fetal distress is 2/2 vulnerability of the fetal brain to hypoxia/ischemia. Unclear timeline for human fetal brain injury during acute hypoxemic-ischemic event.
- Studies in non-human primates and sheep show: 12–15 min of umbilical cord occlusion enough to cause significant neuronal injury in term fetus
- Human fetus can perhaps tolerate 15–20 min in near-total occlusion vs total occlusion, assuming a normoxic fetus at baseline.
- Urgency in fetal distress is 2/2 vulnerability of the fetal brain to hypoxia/ischemia. Unclear timeline for human fetal brain injury during acute hypoxemic-ischemic event.
- What is my plan if I fail to intubate?
- What is my plan if I fail to ventilate?
- In the event of a failed intubation, will I allow surgery to proceed if ventilation is adequate?
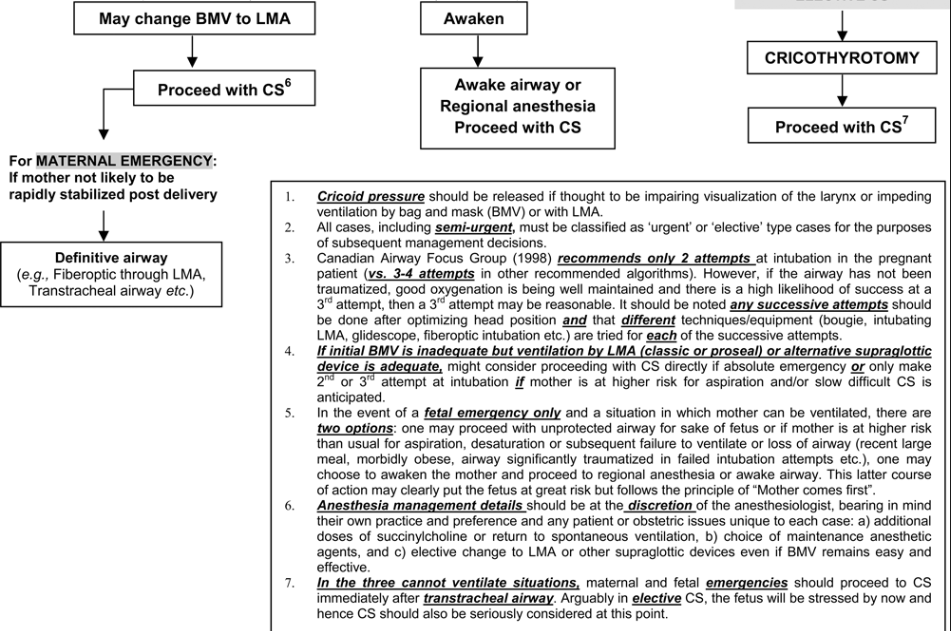
MORE OB DIFFICULT AIRWAY ALGORITHMS


- Adequate preoxygenation must be a priority. Preoxygenate as early and as long as possible to ETO2 > ~ 85%
- >10L/min O2: 3 min tidal breathing, or 8 vital capacity breaths
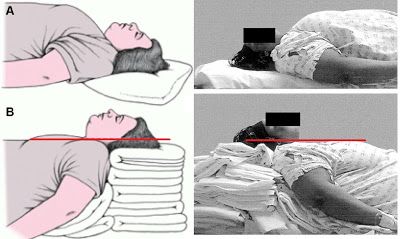
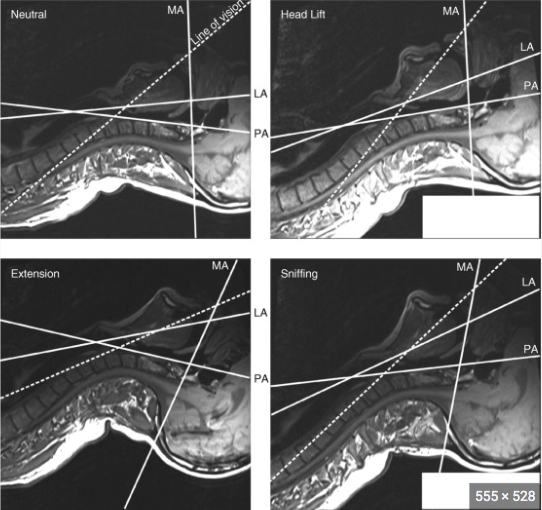
- Patient positioning:
- Ramp/sniffing position improves glottic view, and allows access to cricothyroid membrane
- Also creates more space between her chin and chest for laryngoscope blade to enter mouth as cricoid pressure is being held, because someone’s hand holding pressure on her neck will be in your way.
- Ramp/sniffing position improves glottic view, and allows access to cricothyroid membrane
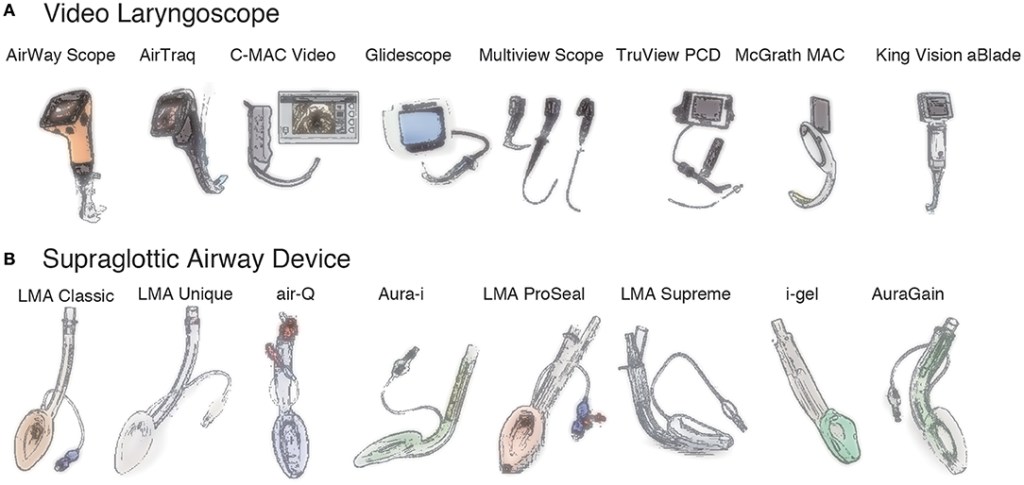
- Videolaryngoscope, ETTs, LMAs, Oral airways, Aintree exchange catheter, boujie, fiberoptic scope. *MLTs should be in difficult airway cart to intubate through LMAs with.
- Succinylcholine vs Rocuronium (large-dose sugammadex allows faster reversal)
- Succs may wear off during difficult airway attempts, making intubation even more difficult. Longer acting Rocuronium may be beneficial in this situation, given its ability to be rapidly reversed.
Pregnancy-Related Features That May Contribute to Difficult Airway
- High risk of aspiration and Mendelson syndrome: (chemical burn from gastric acid aspiration pH <2.5)
- Reduced Lower esophageal sphincter tone & increased intra-gastric pressure
- Gastric emptying delayed by labor and opioids
- Increased gastric acid volume and acidity
- Rapid onset hypoxemia after induction
- FRC reduced by ~20%
- O2 consumption increased by ~25% (up to 60% during labor)
- Difficulty inserting laryngoscope blade
- Enlarged breasts
- Weight gain/obesity
- Someone holding cricoid pressure with their hand in your way
- Poor view at laryngoscopy
- Mispaced cricoid pressure and/or misaligned laryngoscopy 2/2 left lateral tilt
- Airway edema due to increased total body water and reduced colloid-osmotic pressure (decreased albumin)
- Exacerbated by PreE
- Risk of bleeding from airway manipulation
- Capillary engorgement of nasal and oropharyngeal mucosa
- Coagulopathy in PreE/HELLP
- Other factors: Obesity, Mallampati grade 3 or higher, any standard airway assessment abnormalities, OSA.



Sources:
Difficult and failed intubation in obstetrics
The obstetric difficult airway: if we can’t predict it, can we prevent it?
Anesthesiology News: “Airway Management of the Obstetric Patient: What’s New?:”
Airways to watch out for
Pushing, Pressure, Boobs, & Braids
Pushing: Pushing during labor increases airway swelling. Mallampati scores usually increase a grade after pushing. Can lead to easier airway obstruction, worse glottic view, and increased chance of tissue damage and bleeding on intubation.
Pressure: HTN disorders of pregnancy (preE, HELLP) increase airway swelling 2/2 third spacing and endothelial damage disturbing normal starling forces governing fluid movement across vascular and interstitial tissue membranes. The normal airway swelling of pregnancy 2/2 increased volume, TBW, and decreased serum protein, is made worse by PreE. Additionally, PreE and HELLP can cause thrombocytopenia/coagulopathy and make the friable tissue more prone to bleeding.
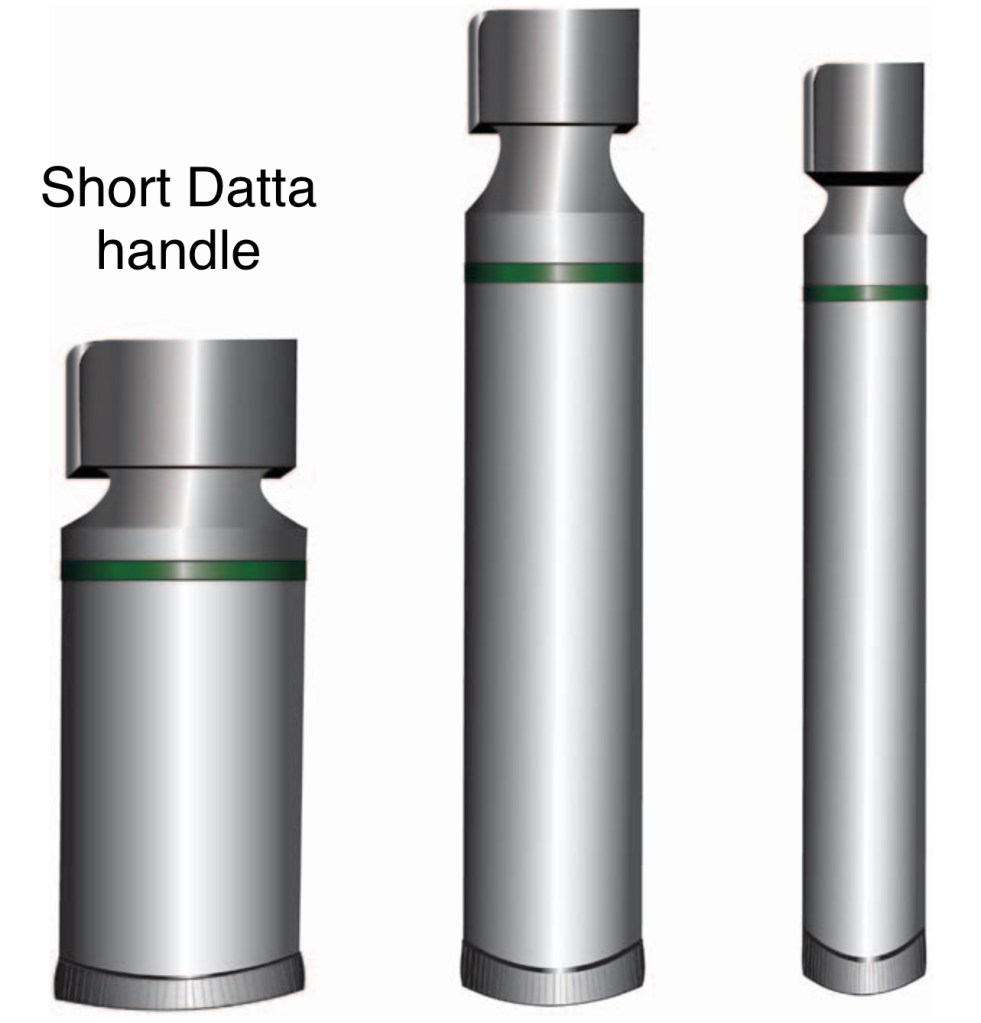
Boobs: Normal breast engorgement at term pregnancy can impair ability to not only perform DL, but impairs neck access for emergency cricothyrotomy in a critical failed airway. Especially women with really large breasts would benefit from a ramp to reposition breast tissue down and away from her neck. Although the Glidescope handle can be turned sideways to insert into mouth, the standard DL mac/miller requires open space around the mandible for blade handle to insert correctly and obtain a view. The Datta handle was developed for this reason.
Braids: Lots of thick hair or braided hair can impair their ability to extend their necks when supine – may impair glottic view. Can take out scrunchie/hair ties, or part hair down middle, if possible, or arrange ramp/towels to allow for full neck extension. Figure this our PRIOR to start or c/s and assess the ability of EVERY c/s pt to extend their neck prior to starting the case. Obstetric airways don’t allow for time to figure it out and reposition as you go.

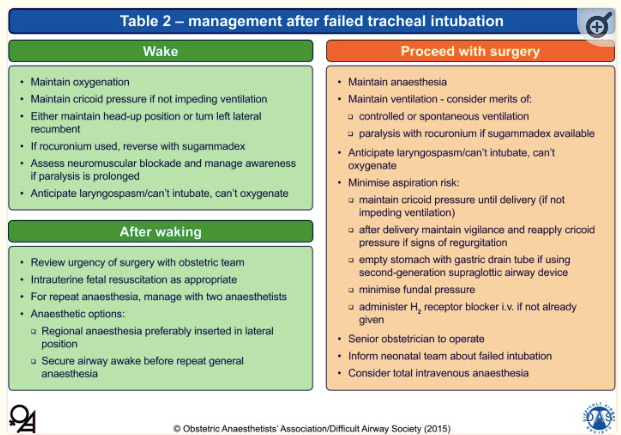
FAILED INTUBATION – CAN YOU VENTILATE?
- Failed intubation clearly announced to whole OR team
- Call for help
- Anesthesia priority: oxygenation & ventilation.
- 1st attempt is via face mask, 2-handed technique with cricoid pressure maintained. USE ORAL AIRWAY to decrease risk of gastric insufflation.
- Communication to whole OR is vital since 2nd pair of hands required to squeeze the bag while another person maintains cricoid pressure.
- Cricoid pressure should be reduced and if necessary released if ventilation remains inadequate.
- An oropharyngeal airway may assist ventilation and reduce gastric insufflation. Nasal instrumentation avoided.
- If ventilation now possible, decide whether to proceed with surgery or wake up.
- If ventilation remains ineffective, an LMA/supraglottic airway device must now be inserted.
CAUTION: Always remember that repeated failed laryngoscopy/ intubation attempts and airway instrumentation of any kind can quickly convert a ‘maskable’ airway into a CICO scenario!
TRACHEAL INTUBATION VIA LMA
KNOW YOUR TECHNIQUE AND EQUIPMENT NEEDED BEFORE ATTEMPTING THIS!!!
2 LINKS: 1) UCSF Intubation through SGA, & 2) Anesthesiology News
LINK 1:
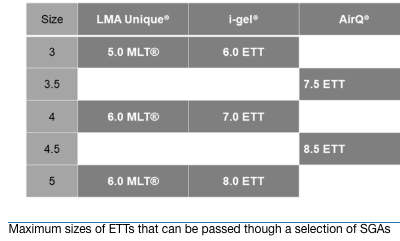
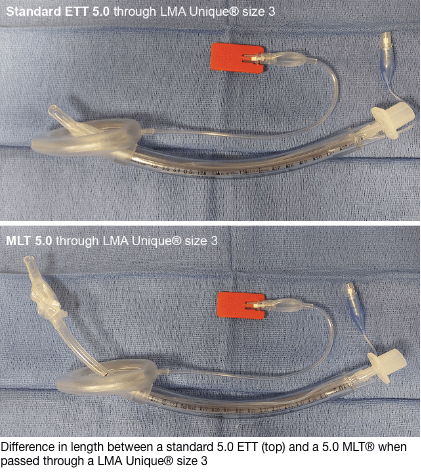
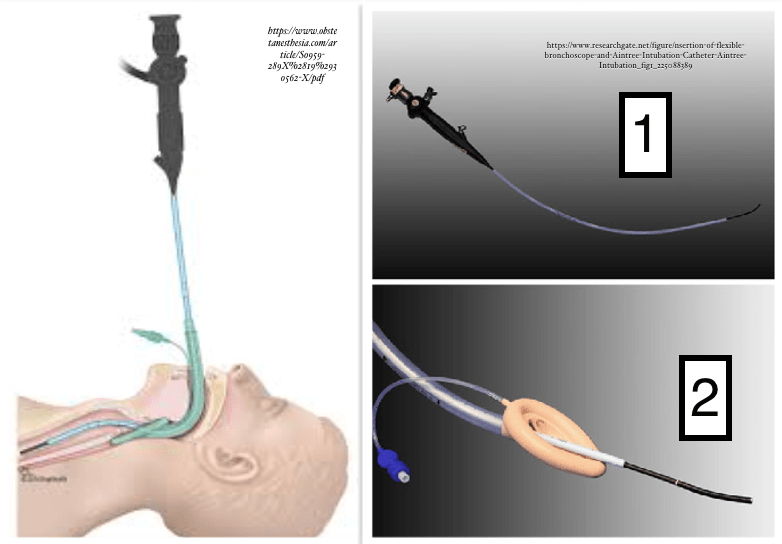
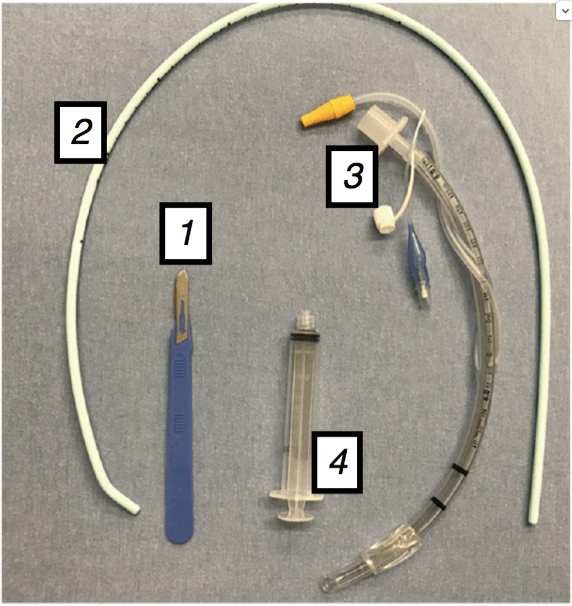
MLTs are always best through any LMA to ensure the ETT cuff will reach past the vocal cords, and should be available in any difficult airway cart*** Otherwise can use AINTREE catheter over FOB, or FOB alongside visualized Boujie through LMA into trachea as a placeholder and railroad ETT over.
- If decision made to continue surgery after an LMA is inserted but a more secure airway is desired, the LMA can be used as a conduit to intubate the trachea.
- Standard ETT may not be long enough to reach through vocal cords from most LMA models – should use Microlaryngoscopy tube (MLT) for increased length.
- LMA Fastrach™ (Intubating LMA) facilitates intubation while maintaining ventilation; however, its insertion and use differ from the classic LMA with which most anesthetists are more familiar.
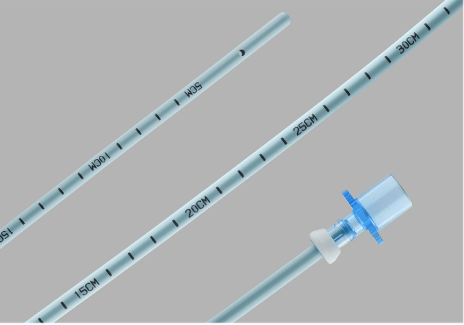
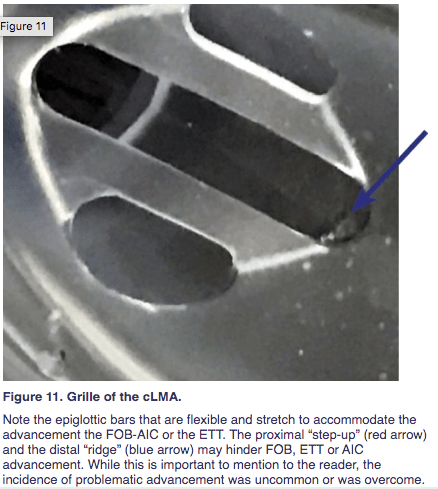
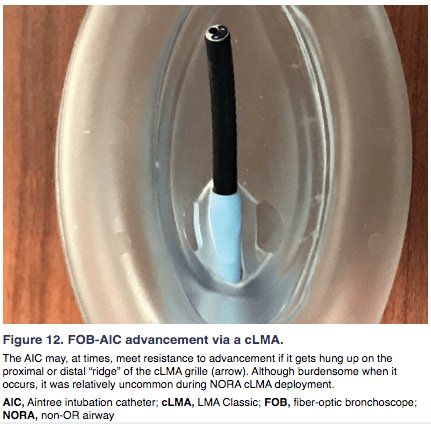
- The Aintree Intubation Catheter (AIC) can be threaded over fiberoptic scope, and passed under fiberoptic guidance into the trachea using the LMA as a conduit. The fiberoptic scope can be removed while the aintree left in place. Then the LMA can be removed over the Aintree. Then a tracheal tube can be railroaded over the Aintree after removal of the LMA.
- The ease of using an AIC may be influenced by the type of LMA acting as the conduit.
- Inserting an LMA Supreme ™ to rescue ventilation may be attractive because of its potential to reduce the risk of gastric regurgitation; however, passage of an AIC may be more difficult through this device than through other LMAs.
Aintree internal diameter 4.8mm, so ONLY fits over slim/pedi FOB.
Aintree External diameter 6.0mm – ONLY 7.0 ETT fits over it.. can’t use 6.0.
Aintree compatible with ANY size LMA: 3, 4, or 5.
LINK 2:
Intubating through an LMA Article: Considerations, Equipment, Explanation, & Pictures:
(This article/guide is the best! And written by our very own Dr. Mort, Difficult Airway Extraordinaire!! 👏 👏)

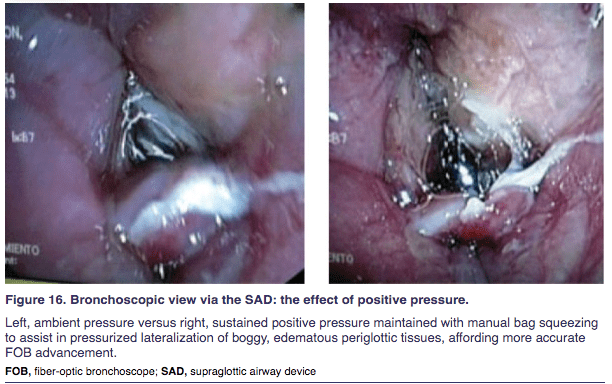
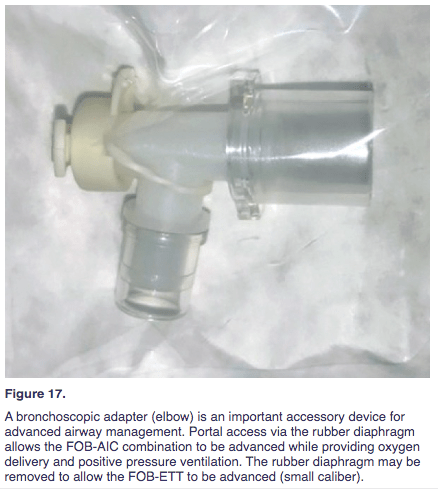
Expert Tip from Dr. Mort: “If one encounters an edematous boggy periglottic area that is difficult to discern exactly where the airway hole is located, the application of PPV may improve visualization of the glottic opening. A colleague then provides ongoing PPV support while FOB intubation takes place. The AIC package (Figure 17, Cook Medical) includes a bronchoscopic adapter. Otherwise, this valuable accessory should be available in the DA cart or FOB tower. “
VIDEOS FOR AINTREE SGA INTUBATION TECHNIQUE
Fibreoptic Guided Intubation through SGA using Aintree Intubation Catheter
And if Aintrees are hard to come by in this scenario bc let’s be serious – you can also place ANY size fiberoptic through LMA and into the trachea, then place a lubed bougie down alongside FOB into trachea and visualize with FOB – then remove LMA and FOB, leaving bougie in trachea, and railroad ETT over the bouigie – VOILA!
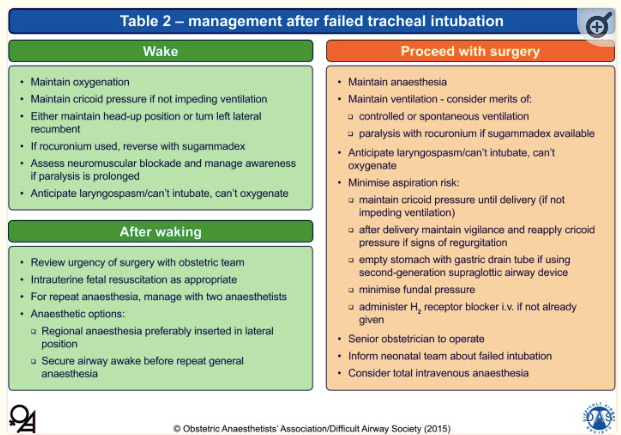
IF FAILED INTUBATION, BUT MUST PROCEED WITH SURGERY & DELIVER:
If intubation has failed, but ventilation is possible, and must continue C/S: (maternal or fetal emergency)
-
- Spontaneous ventilation under deep inhalation anesthesia (SEVO for non-irritant properties) has traditionally been advocated.
- Assisted ventilation with maintained cricoid pressure may be appropriate if ventilation is straightforward.
- High % of volatile agent will decrease uterine tone, but necessary to reduce risk of laryngospasm/bronchospasm in spontaneously ventilating pt. (glyco may also be helpful to dry secretions)
DECISION TO WAKE PT UP
Turning the patient on their side to recover has been advocated; however, if maintaining the airway is already difficult in the supine position, it may be prudent to stay supine with cricoid pressure maintained until the patient is awake.
CAN’T INTUBATE, CAN’T VENTILATE
When both intubation and ventilation have failed, (failed: 2 x intubation, 2 x LMA, and failed mask with OPA) CEASE further attempts at oxygenation by face mask or LMA and proceed RAPIDLY to the NECK to access the upper airway for transtracheal ventilation.
No clear consensus on optimal equipment/technique for providing transtracheal ventilation.
- The Difficult Airway Society recommends following one of two pathways:
- 1) Access the neck with a cannula & ventilate with O2 under high pressure
- 2) Perform a surgical cricothyroidotomy and ventilate with O2 delivered by a low-pressure source (ETT can connect to ventilator).
- Each method requires different equipment & skills and presents different challenges and complications. In such a difficult situation, every anesthetist must know the technique they would use and equipment must be readily available.
- Anesthetists may be better at using a syringe & cannula than a scalpel, making cannulas a more suitable first-line device to access the neck.
- Advantage of cannula cricothyroidotomy:
- reduced risk of trauma during insertion vs scalpel.
- Disadvantage of cannula: risks of jet ventilation.
- Many anesthetists unfamiliar with emergency subglottic jet ventilation. Potential for serious barotrauma and disruption of soft tissues in neck from high-pressure ventilation through a misplaced cannula.
- Advantage of cannula cricothyroidotomy:
- Anesthetists may be better at using a syringe & cannula than a scalpel, making cannulas a more suitable first-line device to access the neck.
Should cannula transtracheal ventilation fail, scalpel incision of cricothyroid membrane and rail-roading an ETT over a bougie inserted into the trachea have been recommended.
Once oxygenation improved, must now decide to continue with surgery or wake up. Unless the mother’s life is seriously threatened, she should be woken up.
SURGICAL AIRWAY
This is the worst case scenario – but it’s important to know how to do this. Does every pt coming for surgery have the ability to extend their neck and allow neck access? Is the pt appropriately ramped/positioned BEFORE start of surgery to allow neck access should an emergency occur and they are unable to be intubated or ventilated?
While videos of cadavers and mannequins are helpful in understanding technique, it’s really important to understand HOW MUCH BLOOD will be present in a live patient. (Watch the videos linked below).. Real life is NOTHING like a cadaver or mannequin…. You will NEED extra hands: helpers can help retract skin, suction blood, apply gauze for blood, and hand you the bougie, ETT, and 10cc syringe to inflate cuff.
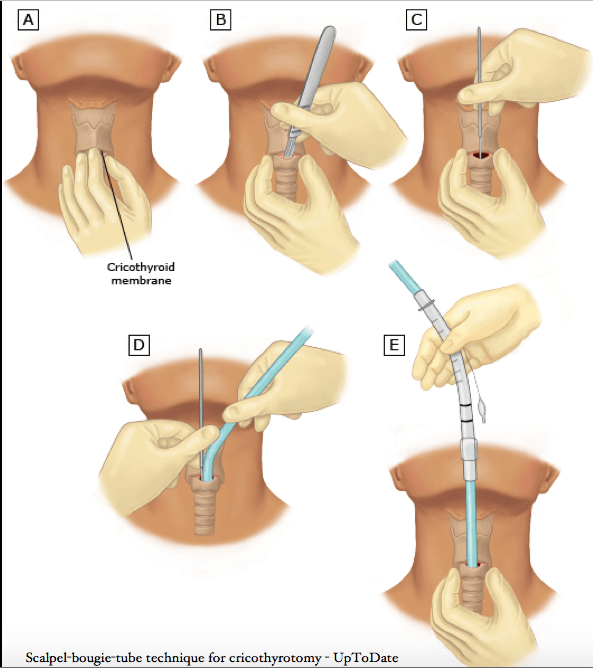

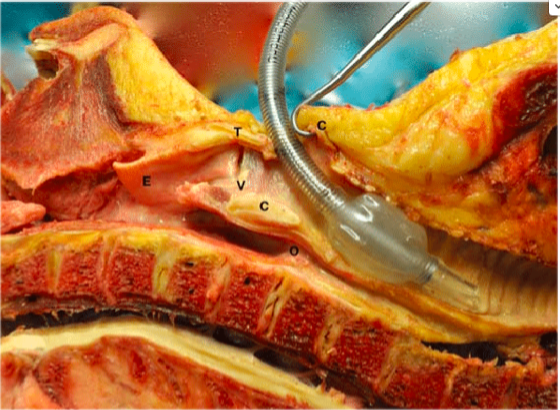
VIDEOS OF SCALPEL-FINGER-BOUGIE TECHNIQUE FOR EMERGENT CRIC
Mannequins for technique:
Scalpel Finger Bougie Cricothyrotomy for SMACC 2014
Bougie Aided Cricothyroidotomy
LIVE patient videos:
LOOK HOW MUCH BLOOD TO EXPECT!!
Surgical Airway (Cricothyrotomy) Performed by Ram Parekh
This second video is in Spanish (skip to 00:30sec). For this video – this cric was poorly executed bc look how difficult it is when they DO NOT USE A BOUGIE or VERTICAL SKIN INCISION. NEVER let go and loose your place once you reach trachea – maintain hole and immediately insert bougie as placeholder for ETT.
Dr. Antonio Navarrete. Vía Aérea Difícil 20: Cricotiroidotomía quirúrgica 2a parte
DECIDING TO WAKE UP OR PROCEED WITH SURGERY & DELIVER
- Sometimes obvious, sometimes not so much:
- Decision weighted by:
- urgency of the procedure
- condition of the mother
- condition of the fetus
- experience of the anesthetist, and their confidence in that pt’s airway management
- In case of a failed intubation in elective C/S:
- Mother should be woken.
- UNLESS faced with a life-threatening maternal event:
- severe ante-partum hemorrhage
- maternal cardiac arrest requiring peri-mortem C/S
- there is no option but to proceed with surgery.
- UNLESS faced with a life-threatening maternal event:
- Mother should be woken.
- More difficult if failed intubation during a non-elective C/S for fetal distress where ventilation by an LMA is adequate but the fetal heart remains compromised.
- The LMA has been used in many Caesareans but most reports are of elective, fasted, non-obese women.
- Case reports of LMA rescuing ventilation in emergency situations do not prove the safety of the technique. They only provide reassurance that proceeding with surgery, while maintaining cricoid pressure may be appropriate in some situations.
- Without clear available guidance on what to do in these grey areas, the best decision made will be based on the case circumstances and the experience of the anesthetist.
- It is important to consider this before inducing GA
Remember you can intubate through an LMA with a fiberoptic scope: Can use Aintreee over fiberoptic scope, OR can slide boujie down LMA alongside fiberoptic scope, and place boujie into trachea under FOB guidance, then remove LMA and railroad ETT over boujie.
RECOVERY
Serious airway problems have occurred in pregnant women during recovery from GA. If there have been multiple intubation attempts or signs of airway edema at laryngoscopy, there is a potential for FATAL airway problems after extubation. The cuff of the tracheal tube should be deflated before extubation and a leak around the tube confirmed before its removal. Extubation in all obstetric patients should be AWAKE. If no cuff leak or known significant swelling/airay trauma = DO NOT EXTUBATE!!! Swelling will only worsen as postpartum fluid shifts increase swelling and edema. Pt must go to ICU until swelling resides and extbation is safe!
ADDITIONAL CONSIDERATIONS
re: PARALYTICS
- There is evidence that significant gastric insufflation unlikely during gentle PPV if cricoid pressure correctly applied and ORAL AIRWAY* utilized
- Gentle bag-mask ventilation has been advocated for after induction to prevent/delay desaturation and allow more time should intubation be difficult.
- Especially if Roc used instead of succs.
- DAS/OAA guidelines perform gentle facemask ventilation before tracheal intubation decreases the risk of desaturation AND the stress level of the anaesthetist**
- High-flow nasal cannula with humidified O2 increases apnea time, but has not yet been adequately tested in OB pts.
- Face mask ventilation may be easier in the presence of adequate muscle relaxation
- (may be benefit to Roc vs succs, if adequate sugammadex available)
- Avoid a 2nd dose of succs after failed intubation:
- Correct course of action is to abandon intubation attempts and provide ventilation and oxygenation by other means.
- In failed intubation, face mask ventilation or LMA insertion may be difficult 2/2 decreasing depth of anesthesia and incomplete muscle relaxation.
- In this situation, the patient may not be sufficiently awake to spontaneously ventilate or deep/paralysed enough for ventilation to be effectively provided.
- Whether muscle relaxation may be beneficial in these circumstances is debatable.
- Gentle bag-mask ventilation has been advocated for after induction to prevent/delay desaturation and allow more time should intubation be difficult.
- Sugammadex may influence established practice in obstetric airway management.
- May increase safety & confidence using longer-acting Roc induction, which may have benefits in difficult airway management.
- If Sugammadex required to reverse Rocuronium, needs to be administered rapidly in correct dose.
- Maintaining a supply on the difficult airway cart along with clear dosing guidelines is sensible.
- Sugammadex rapid & permanent reversal of paralytic does not imply rapid return of spontaneous ventilation – airway can remain obstructed/no return of respiratory drive.
- Maintaining a supply on the difficult airway cart along with clear dosing guidelines is sensible.
- ON EMERGENCE – ENSURE FULL RECOVERY OF MUSCLE FUNCTION – especially since magnesium can impair respiratory muscle strength. (And Mag given in preE (preE puts pts at higher risk of airway swelling 2/2 damaged vascular/capillary endothelium)
- When you’re alone managing extubation, you can feel pressure from team/obgyns (who do NOT manage airways) to always extubate, but it is your responsibility to only extubate patients who are 100% ready.
- But if the pt has no leak – the answer is NO. Once again: incidence of airway-related mortality in OB is just as high, if not HIGHEST in post-extubation period
SALAD TECHNIQUE: INTUBATION DURING ACTIVE ASPIRATION: