CONTENTS:
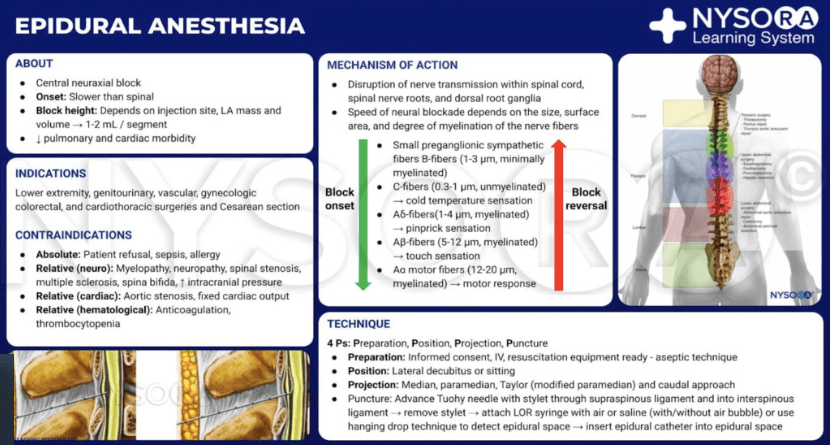
- Epidural sensory levels
- Epidural anatomy review
- Epidural placement tips/troubleshooting
- Contraindications to neuraxial are in NEURAXIAL C/S – Same for epidural
- Timing of labor and labor epidurals: NPO guidelines and Labor stages
- Adding fent to epidurals
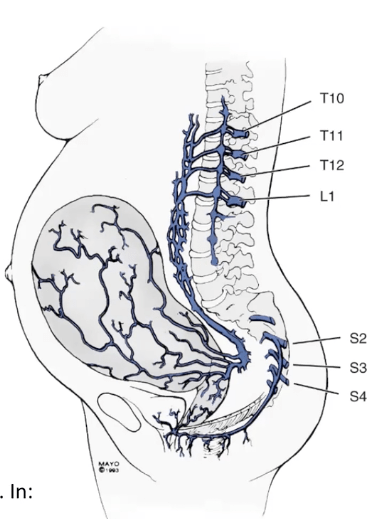
- Spinal nerve, dermatome, sensory coverage assessment review
- Labor CSE: timing & techniques
- Pros/cons of Labor CSE
- Physiologic responses and comorbidity considerations for dosing/topoffs/ sympathectomy/ Horner Syndrome
- Top-offs and troubleshooting
EPIDURAL LABOR ANALGESIA

3 Big Things:
- Get organized & efficient at Pre-procedure interviews and consent.
- Don’t show your face in the room until you have at least skimmed her chart, seen her labs, and can efficiently do a pre-op. If she is in pain, the second she sees you, the clock to relief starts ticking for her. So read the room and don’t ask 500 slow meandering questions as she’s dying with each contraction – that is torture.
- Spend the time to memorize a system for pre-op interviews that is thorough and efficient. Your patients will thank you and love you forever. (One method is listed in the NEURAXIAL for C/S page, Use whatever works and makes sense for you – just get good at it)
2. CONTROL THE ROOM
- You’re doing a procedure many pts are pretty apprehensive about, to say the least. Some are easy, some are SO FRUSTRATINGLY DIFFICULT. It’s ok, if they were easy, everyone would do them…The skill comes in when troubleshooting the difficult ones. And it’s so important to keep calm, no matter what. As soon as she hears you sound doubtful or not confident, or anyone in the room sees you sweat, everything spirals. I have dropped every single thing in my kit on the floor before, I’ve gotten extra equipment, I’ve gotten entirely new kits and started over, IT’S OK. I’ve had to take my gloves off and told the nurse in the room – watch the sterile field for a sec, and had go out to the hallway at 4am and get more equipment. Or I’ve given the nurses my badge and directed them where to get more stuff for me from our carts…Nobody cares if it takes a while or you have to get more stuff – they care that you know what you’re doing. When you’re brand new – by all means ask for someone to give you a hand in the tough ones – we don’t want to torture people, but also know that some of these are just really difficult. Don’t become demoralized or visibly shaken if it’s a tough one or it’s taking a bit of time. Be gentle and reassuring. The room could catch fire and you have to be totally calm and zen and self-assured. A-hem it’s called *acting*… and many of us have delivered oscar-worthy performances..
- “This space is a little tricky but no worries I’m wiggling my way in. Are you doing ok? Anything sharp or just pressure? I want to make sure I’m keeping you comfortable while I navigate this.”
- “Do you need a quick break? I can pause and you let me know when you’re ready for me to proceed – we’ll get there don’t worry. We’ll be best friends again once this epidural is in and working”
- “Sometimes this is just a positioning thing – let’s reposition again and see if we can get this anatomy to line up a little better.”
- (drops Tuohy on floor) “Give me one sec I have to grab one extra piece of equipment for this kit.”
3. POSITIONING POSITIONING POSITIONING
- “Difficult” epidurals are often made worse by poor positioning. You can be the epidural G.O.A.T – a crappy position won’t open the space and you’ll hit os everywhere. We’re behind her sticking giant needles into her back – any sane person will reflexively pull away. Every time you touch her she’s going to reflexively pull away a little, in anticipation of a giant needle – often without even meaning to. But when they PULL AWAY – They are EXTENDING (arching) their backs and closing/narrowing the intervertebral spaces. Be patient & reposition CONSTANTLY. I explain that positioning is the most important part, and tell them to feel my hand on their back and push out against it. I correct their position constantly throughout the procedure.
- This lumbar flexion can also be explained like a pelvic tilt tucking their bottom in under them.
- Also important they don’t lean forward from the hip. This also lends to extension & prevents the lumbar FLEXION we need. It also messes up your anatomy angles and Tuohy trajectory. They have to sit straight up “like the letter L,” relax shoulders and push their lower back out from there.

EPIDURAL SENSORY LEVELS
Epidural Anesthesia and Analgesia
Important to distinguish a key difference between Epidural and Spinal anesthesia.
- Spinal/Intrathecal LA works by spreading evenly through small fluid compartment of CSF and bathing spinal nerves evenly. Block level is BILATERAL AND EVEN from highest level down. So if pt has block at T4, she reliably also has block at T5-12, L1-5, S1-5, etc – EVERYTHING from that level DOWN is reliably blocked.
- Assessing a spinal’s coverage is just assessing where the highest level of sensory loss/pain relief is.
- T4 block to COLD (C-fiber: visceral pain) required to cover discomfort from visceral/peritoneal pain as uterus is manipulated. 2 levels lower at T6 the sharp pain will be blocked (A-deltaType1&2), and T10 block is required for sharp pain from incision, so a T4 block would reliably cover everything.
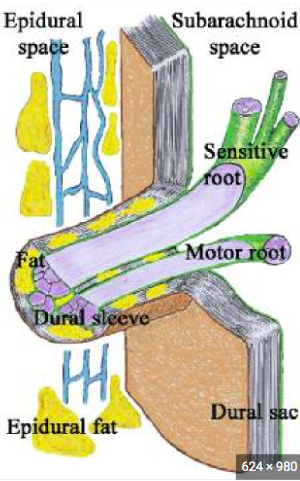
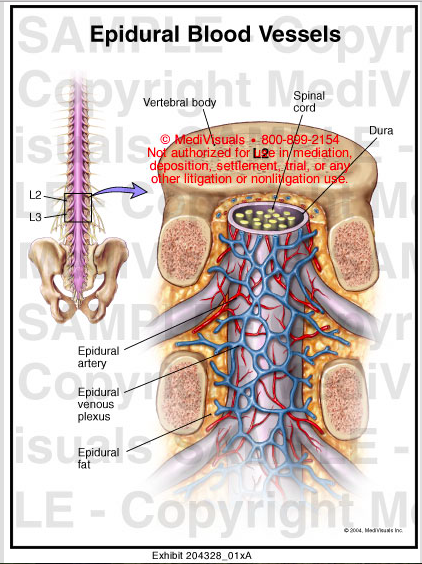
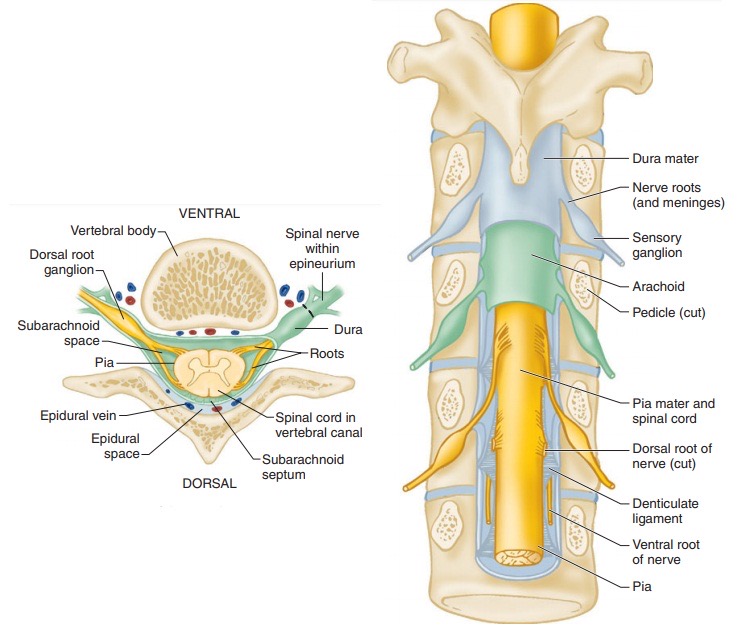
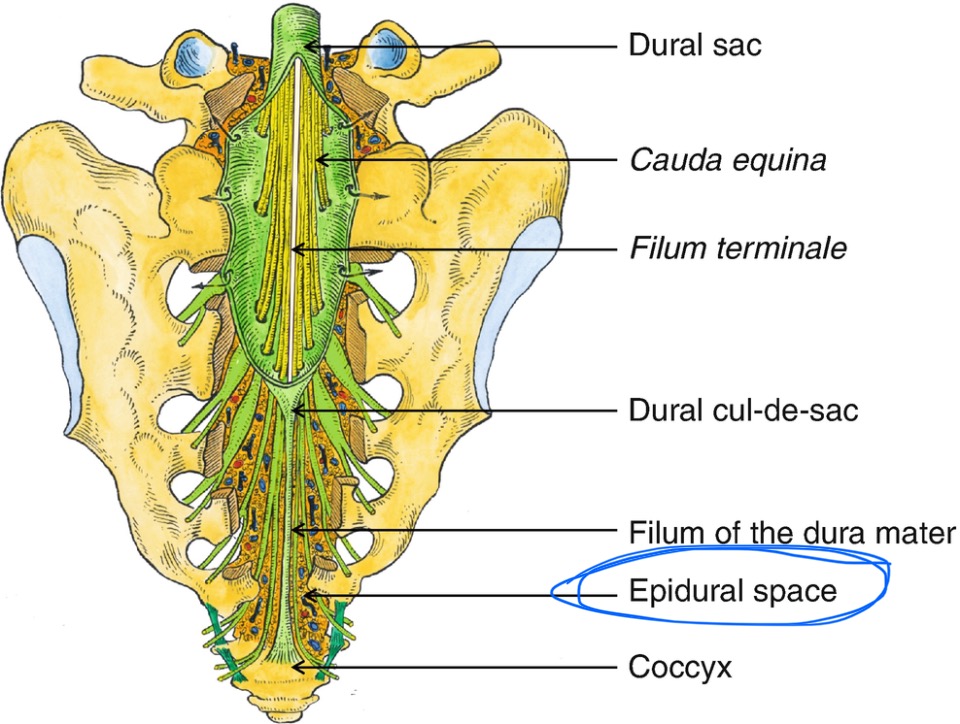
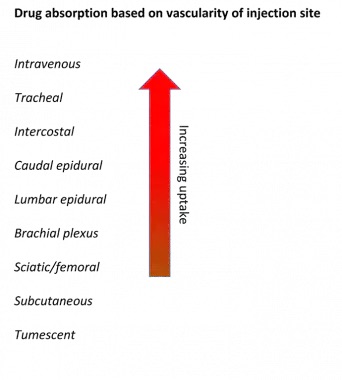
- EPIDURALS, however, work by LA spreading through epidural space to reach bilateral spinal nerve roots and dorsal root ganglion as they exit the spinal cord and traverse epidural space. LA must bathe each individual nerve root to provide relief. The epidural space is not a nice open fluid-filled compartment that encourages even LA spread. It is instead filled with fat tissue, vessels, and connective tissue. This means there can be uneven spread, and nerve roots that get spared, creating “windows” where the patient still feels pain over certain dermatomes.
- Assessing epidural coverage requires assessing each dermatome (if pt complaining of pain) to assure adequate bilateral spread through this epidural space filled with obstacles.
- Don’t worry though, the pt WILL tell you if a dermatome is not covered!
- T10-L1 cover sharp pain (A-delta) from uterine cxns and cervical dilation.
- S2-S4 also needed for later labor and pushing to cover pudendal nerve pain from pelvic stretching and pressure. Can see one-sided pain or spared dermatomes, requiring better epidural spread through high volume, low concentration boluses to force fluid channel communication to allow LA contact with each nerve root traversing epidural space.
- Assessing epidural coverage requires assessing each dermatome (if pt complaining of pain) to assure adequate bilateral spread through this epidural space filled with obstacles.
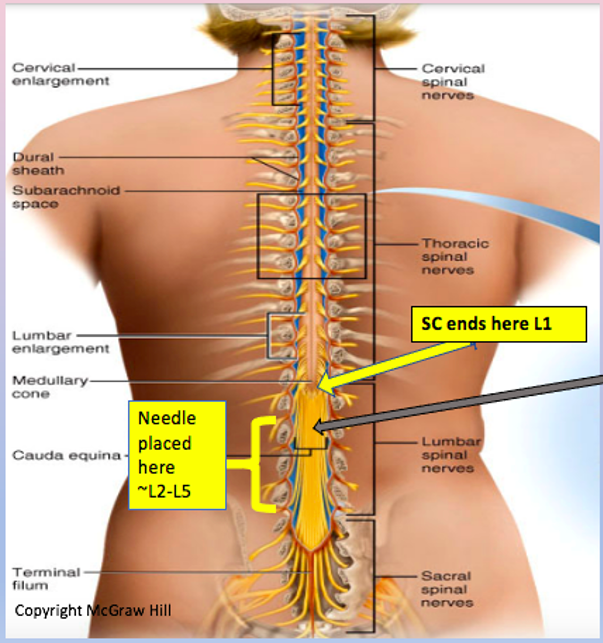
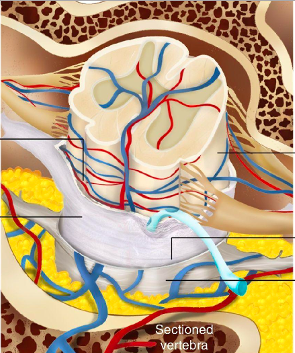
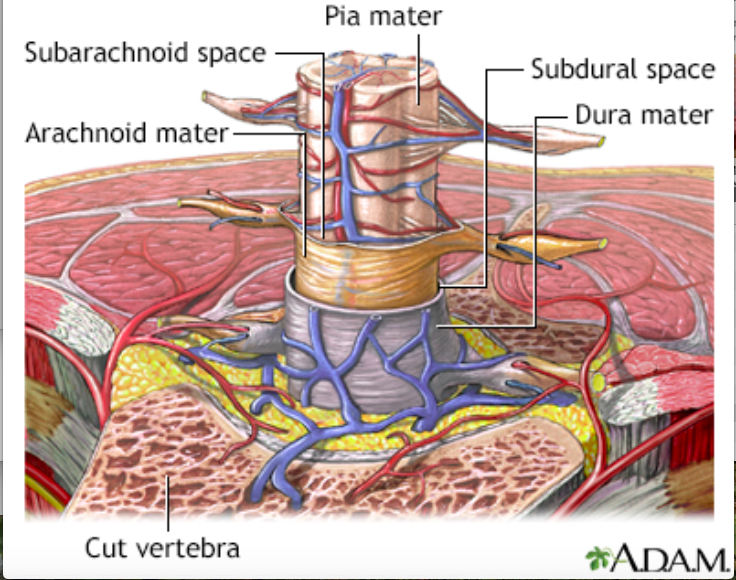
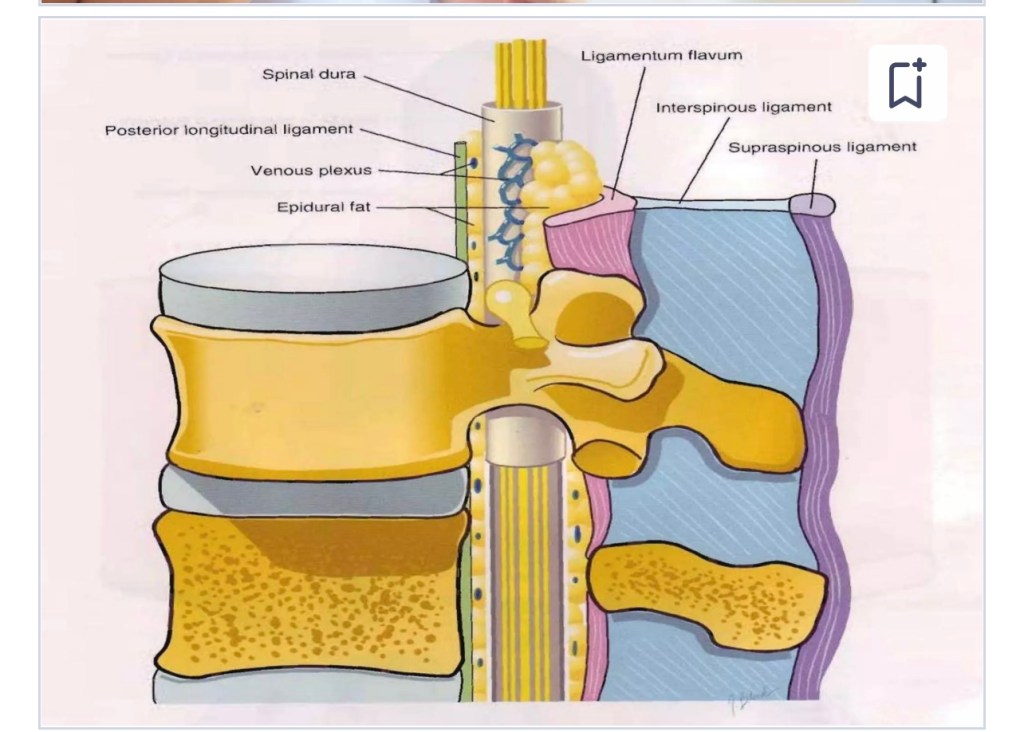
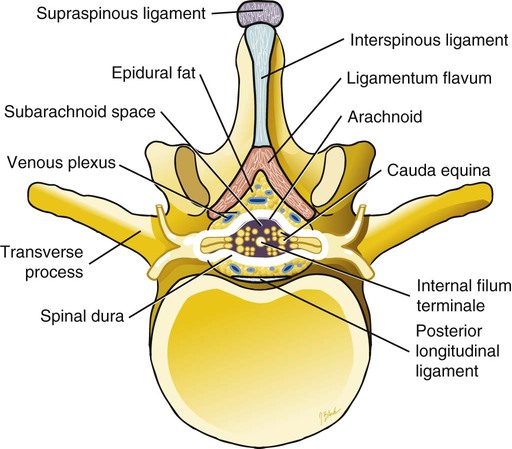
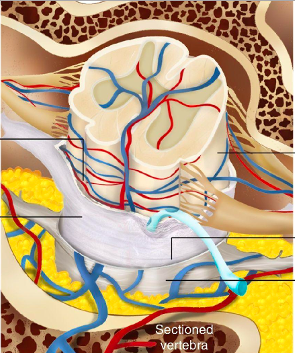
Epidural Anatomy
- SKIN/SUBQ tissue (localize and skin wheel)
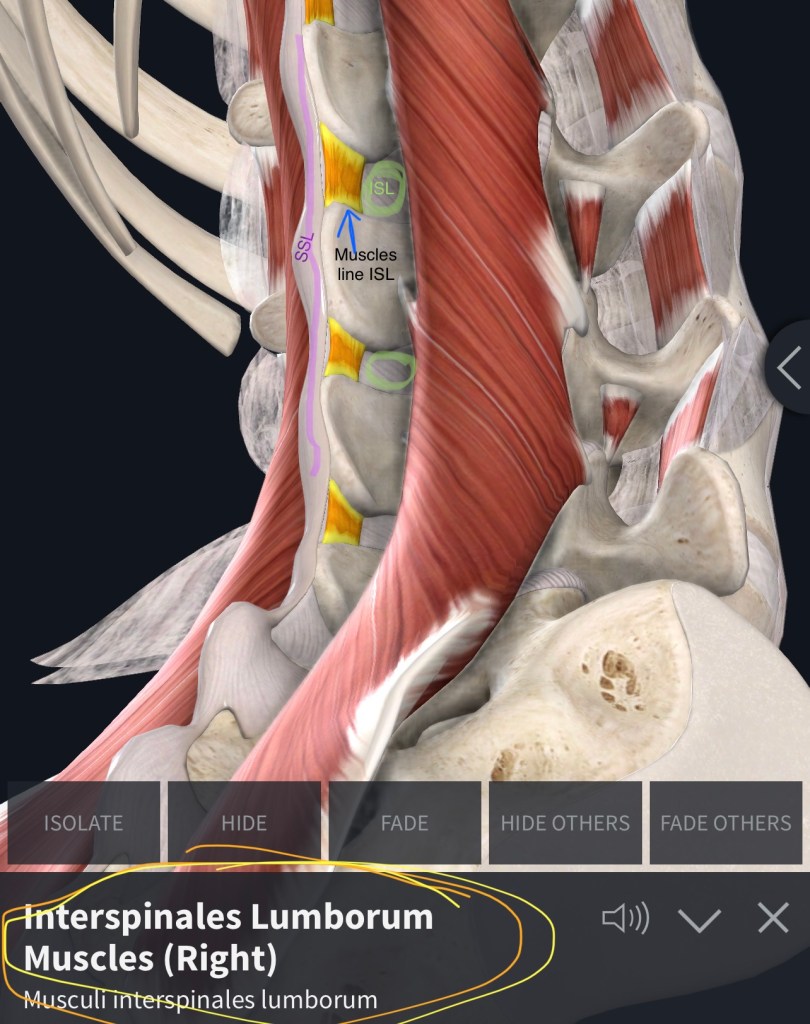
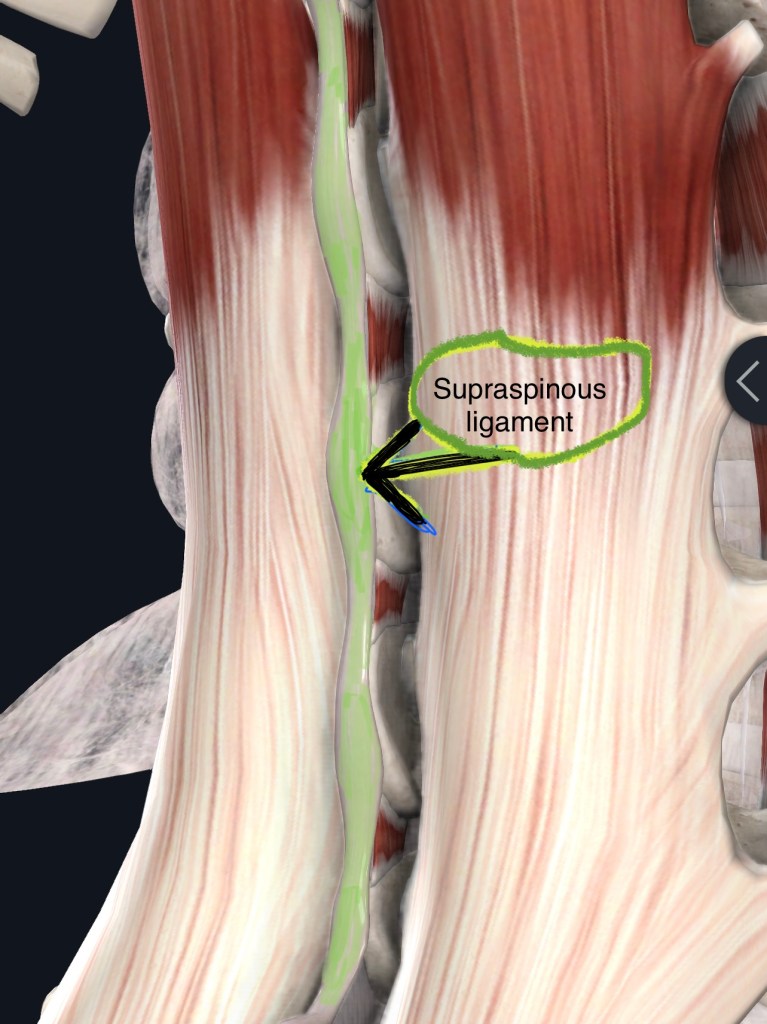
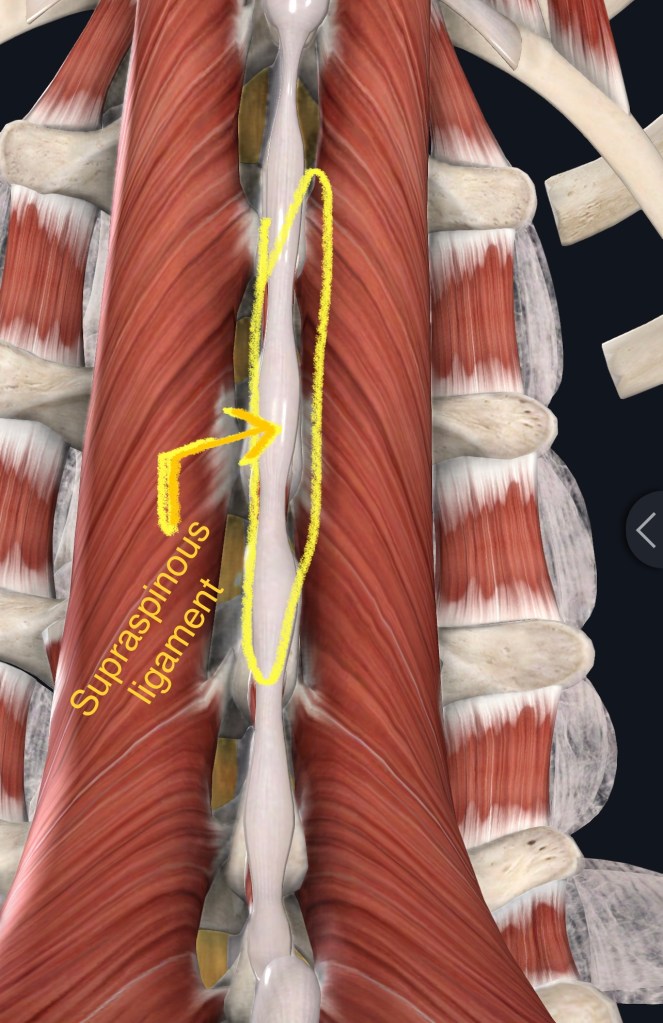
- Supraspinous ligament (first crunch)
- Interspinous ligament
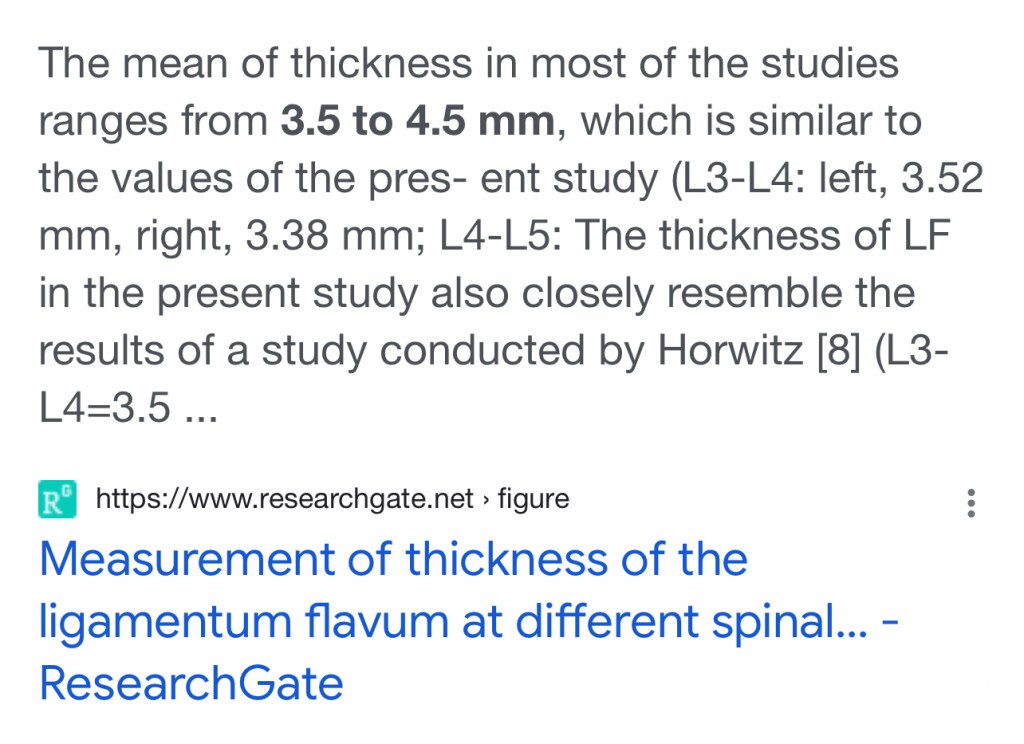
- Ligamentum flavum (ligament is ~3-5mm thick) (crunchy)
- LOR at Lumbar Epidural space (space is ~3-5mm wide)
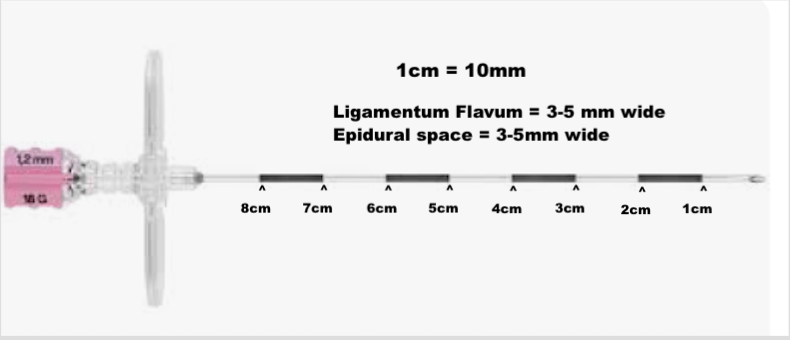
- This means the distance from entering ligamentum flavum and wet-tapping the pt is ONE CM. ONE little silver/black marking on your 10cm Tuohy needle.
- Trying to engage ligamentum flavum right off the bat with the styletted tuohy could put you at higher risk for wet tap, bc you haven’t been able to keep track of your anatomy path via ligament resistance feedback with LOR syringe, and if it’s a softer ligament or you pop right through, you may be unsure of whether the loss of resistance you feel is accurate
- SAFEST technique is to pass through supraspinous ligament and stabilize Tuohy in interspinous ligament, THEN remove stylet, attach LOR syringe, and advance further through interspinous and into ligamentum flavum. You will usually notice increased resistance to LOR syringe when you hit ligamentum flavum.
- Once you engage ligamentum flavum, go slowly & carefully. There is minimal room for error. Post-dural puncture headaches leave women in incapacitating pain. They say their headache hurts worse than their 4th degree tear or their major abdominal surgery c-section incision. Do everything to prevent them.
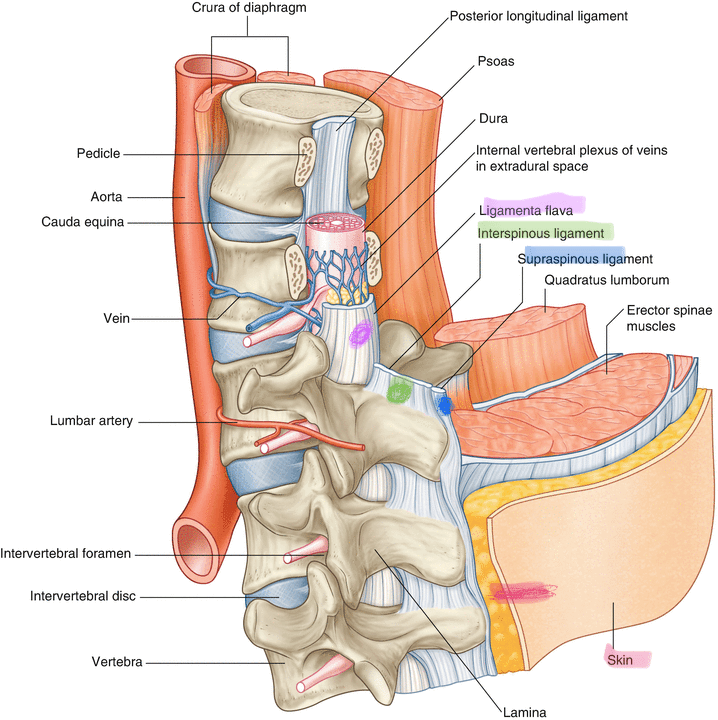
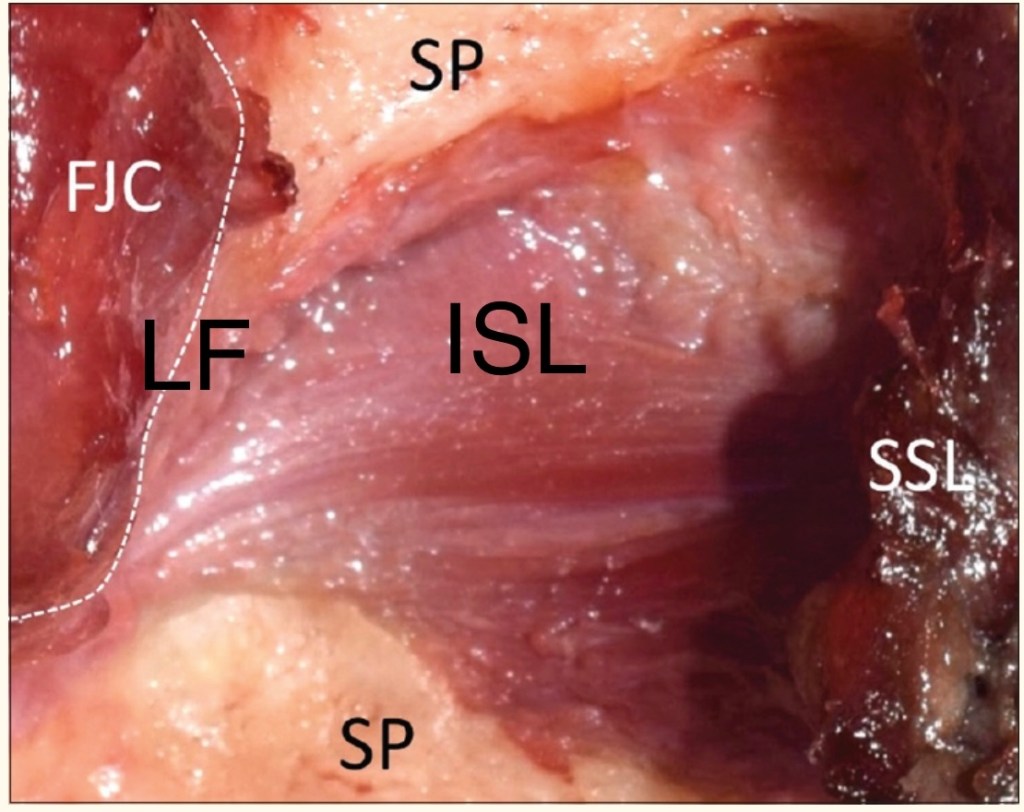

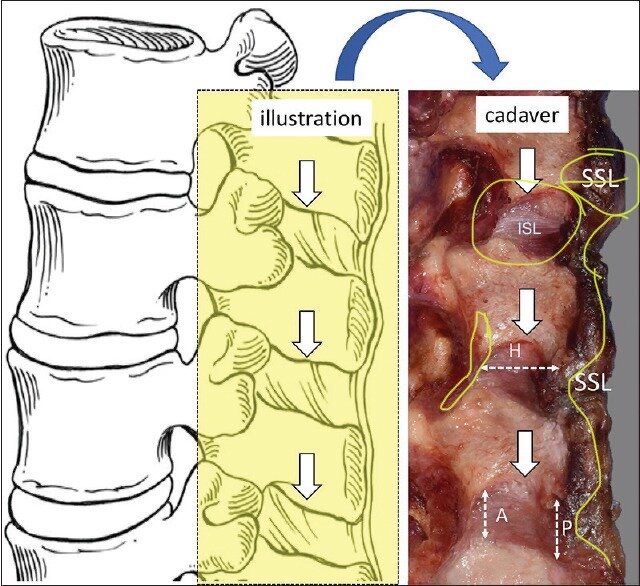

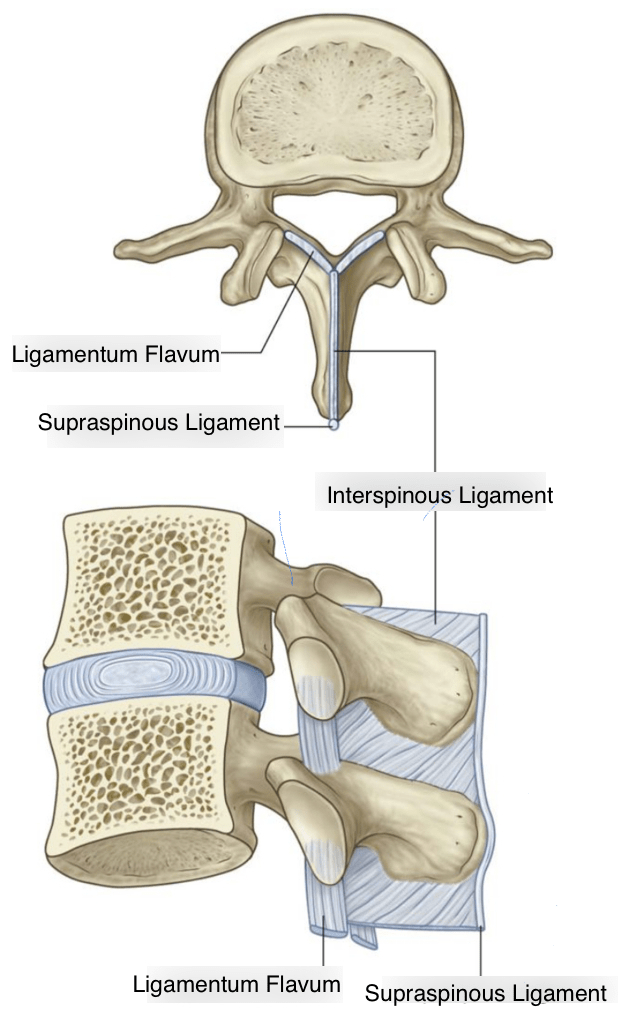


SUPRASPINOUS to INTERSPINOUS to LIGAMENTUM FLAVUM:
Threading a straight line…*at midline*
- Take note in all the photos above and below of how narrow Supraspinous(SSL) and Interspinous ligaments(ISL) really are. The following photos show some of the musculature alongside the Interspinous ligament. Notice the SSL is slightly wider than the ISL, meaning you can feel the crunch of going through SSL and still not be in the center of the ISL – you can still be a little off midline and get into musculature on the side of the ISL. It’s ok, but it will hurt and bleed more – and means you’re off midline and more likely to hit os.
- We localize only the dermis & subcutaneous tissue bc that’s where the sensory nerve endings are. Ligaments don’t have nerve endings for sharp pain – pt should only feel pressure … that is, IF you’re midline… if you’re not midline and hit those muscles framing the Interspinous ligament – your pt will feel sharp pain on one side or another. This will clue you in to being off-midline, and you can redirect your Tuohy accordingly. Tiny *tiny* mm adjustments make large trajectory differences by the time you reach Ligamentum Flavum.
- Also muscle is very vascular, and there are vessels on either side of the ISL – if you’re getting blood back in the tuohy – you’re a little off midline. *Clear the tuohy out well with stylet- blood will easily clot & clog your Tuohy, impairing your tissue feedback. You wouldn’t even know if you had a wet tap bc no csf would come back through a clogged Tuohy.
- Also – don’t panic when you first see this – when you hit a vessel with an 18/17g Tuohy – either in muscle or in the epidural space – you will get a RIVER of blood back in your LOR syringe – it *pours* back. It’s especially pronounced if you use saline for LOR. It looks very dramatic, and the first time people see it they’re like OMG this is a crime scene. But don’t worry – your pt will be fine. Just careful with those glass syringes – once they get blood in them they can get a little sticky from the RBCs and lose their fricton-less glide….so clear out your Tuhoy well with the stylet, and flush your glass LOR syringe out with some fresh saline (the plastic LOR syringes are fine – just the glass ones seem to get a little sticky with blood)
- When I get into musculature before LOR and hit a vessel, I usually just mention to the pt they might feel like there’s a little bruise/soreness on their back even if they don’t see a bruise – (there may be a tiny hematoma in the muscles on the side of the ISL)
- IF you hit a vessel in the epidural space with the Tuohy (after LOR) – they’re hypercoagulable in pregnancy – it’ll be OK. Epidural catheters also thread into vessels all the time – its ok – it’s only a problem if they have a coagulopathy/blood thinner and can’t form a clot (epidurals contraindicated anyway).
- Also – don’t panic when you first see this – when you hit a vessel with an 18/17g Tuohy – either in muscle or in the epidural space – you will get a RIVER of blood back in your LOR syringe – it *pours* back. It’s especially pronounced if you use saline for LOR. It looks very dramatic, and the first time people see it they’re like OMG this is a crime scene. But don’t worry – your pt will be fine. Just careful with those glass syringes – once they get blood in them they can get a little sticky from the RBCs and lose their fricton-less glide….so clear out your Tuhoy well with the stylet, and flush your glass LOR syringe out with some fresh saline (the plastic LOR syringes are fine – just the glass ones seem to get a little sticky with blood)

Human Lumbar Ligamentum Flavum Anatomy for Epidural… : Anesthesia & Analgesia
The incidence of lumbar ligamentum flavum midline gaps – PubMed
Troubleshooting Placement
Placement tips from NEURAXIAL C/S page, repeated:
- Orient to L4 spinous process interspace with iliacrests/tuffiers line. You may still be a level higher than you think, so always feel out the level below especially in shorter and heavier patients. L4-L5 might be your widest interspace.
- Positioning is EVERYTHING*, remind patient throughout procedure to push out their back against your finger/hand (flexion). They’ll subconsciously pull away the whole time and extend/arch their back. Esp after you numb them bc that lido stings like a mofo. Once they’re numb, reposition them again.
TIPS TO MINIMIZE PAIN (and improve positioning/cooperation):
(that have worked for me at least..you can take them or leave them)
- Pain and anxiety are HUGE factors working against you in terms of pts maintaining their position and cooperating throughout the procedure. The little things we can do to mentally prepare them and minimize pain are 1000% worth it.
- These are small things that swear have made all the difference. The devil is in the details:
- MENTAL PREP & SETTING EXPECTATIONS:
- In the pre-procedure interview, I say the same thing to every single pt and I plant this seed: “This isn’t a very painful procedure or a very long procedure. It usually takes 10 mins or so, and worst part is the numbing. I use the smallest needle in the hospital to numb a tiny spot your back, but the numbing medicine burns for a few seconds. So it’s really not the needle that’s painful, it’s just that the solution stings a bit. I’m only going to work in that numb area, so the bigger scarier needles you won’t feel any sharpness from – it’ll just feel like pressure.” I think this re-framing really takes the edge off for a lot of pts who are reasonably afraid of a giant needle in their back and how much it’s going to hurt. For many women this is the most dreaded and feared part of their whole labor/whole life. They cannot wrap their heads around a giant needle in their back and are convinced it’s going to be painful and leave them paralyzed.
- I also add “I’m working well below the level of your spinal cord. So if you’re uncomfortable and have to move a little with cxns, it’s ok I’ll work between cxns and go at your pace. I only do these on women in labor who are usually in pain, so there’s nothing you can do I haven’t seen before. There will come a point where I need you to be still for like 30 secs (going through lig.flavum and LOR to avoid wet-tap) and I’ll tell you when that is. But it’s not because moving will damage your spinal cord, it’s because when you move around, it closes the space I’m working in and makes it really difficult to access the epidural space “ (eliminate their fear of being paralyzed from the needle if they move).
- Then I say, after the skin wheal, “OK THAT WAS THE WORST PART AND THAT PART IS OVER. You did great. That numbing burns like crazy. So take a sec to recover from that, and let’s get back into that procedure position whenever you’re ready..take your time. I have a little more numbing medicine for you, but that first poke is always the worst..” Now they know what to expect, feel a little relief (mental games) and “whenever you’re ready, take your time” gives them back some agency and control to actively participate in the procedure. I swear they are more relaxed through the rest of the procedure and position themselves better bc they are active participants working with me, and aren’t anxiously pulling away as much. I am talking to them through the whole procedure – when passing through ligaments, I’m telling them they’re going to feel more pressure right in the center of their backs and this is all normal, they’re doing really great etc etc…lots of reassurance.
- Lately I’ve been dropping a sterile insulin* syringe onto my field and doing the first skin wheal with it – I draw it up straight from the glass lido vial. (Our L&D rooms always have an insulin needle in one of their drawers for the GDMA pts, so I snag it.) Pts seem to be jumping way less on that first poke. Then I proceed with the kit’s local needles to finish localizing down to SSL. I think it’s made a HUGE difference in pt comfort, and their jumpiness throughout the whole procedure. Everything seems smoother since I started doing this..
- LOCALIZING:
- Small thing I think helps a lot: before poking them with the insulin needle (“big pinch on 3.. 1, 2, 3”) I spray their back with a little of the lido from the syringe just before inserting the needle, so the first sensation they feel (that they’re dreading) isn’t sharp – it’s just cold and wet, and that gets the startle/nerves out of the way, then I poke with the insulin needle and slowly* inject the lido. Rapid tissue spread is painful, regardless of the solution used.
- Skin wheal with insulin needle: doesn’t have to be a huge dime-sized wheal – skin wheals HURT – it’s a lot of stretching. Should be just big enough for the tuohy (your biggest needle) to easily pass through.
- Make one straight numb tunnel with longer local needles down to SSL, and work within that tunnel. Don’t fan the local needle around – you’re only cutting across more nerve endings and causing more pain – and what’s the point? We’re going in with a straight tuohy, so make a straight tunnel. Leaving the tuohy inserted, you can drag your numb subQ tunnel up and down with your tuohy needle to explore up and down – usually the skin and sub Q tissue allow you to drag that tunnel around a bit.
- TB* syringes still have a bigger needle, use an INSULIN needle – it’s so tiny. Also important to not let that insulin needle touch anything before skin puncture – don’t put it through a rubber stopper – it’ll dull the tiny needle and then it’s painful to insert and now what’s the point anymore? (the rubber stoppers on insulin vials are SUPER thin and don’t dull the needle, whereas normal rubber stoppers on lido vials are thick.)
- As a total tangent on my love affair with localizing using insulin needles: If you want to draw up lido for an IV insertion or something using an insulin needle – draw the lido up in a reg syringe with a regular fill needle – then disconnect the needle and put the insulin needle through the luer lock hole in the lido syringe and draw it up from there – it’s like a push and pull from one syringe to the other and it’s messy and lido gets everywhere but whatever it keeps the needle sharp*** Then when you make your little lido skin wheal for an IV, push some lido through the needle first to prime in the needle, and go under ONE LAYER of skin cells so you can basically see the insulin needle tip through the skin, and slowly* inject the lido. This is virtually painless and the awake IV sticks (like a high risk hemorrhage who needs 2 large bore PIVs before we start the case) will love you.
- LOCALIZING:
BACK TO TROUBLESHOOTING PLACEMENT:
- RE-DIRECTING THE NEEDLE: when hitting os or vessels (or pt complaining of sharpness on one side) with the Tuhoy, you’ll need to redirect. The first thing I do is let go of the Tuohy completely and see if it’s leaning in one direction or another. It won’t fall out. I also re-assess the pt position. We can get tunnel vision working in this little sterile window and the pt can meanwhile be leaning forward, arching their backs, leaning sideways, etc etc making the procedure more challenging. So I first see if the Tuohy obviously is slanted, and then I reposition my pt and go around to the side of the bed and check her positioning from there to make sure she’s not leaning forward.
- When you re-direct your Tuohy, it’s kind of like correcting a parking space. It’s already engaged in a lot of connective tissue that doesn’t have a lot of elasticity and wiggle room, so it’s not as easy as just swiveling the needle around. You can wiggle the half outside the patient around but you’re really just bending the needle a bit and I don’t know that the tip really moves too much – instead you need to pull back to SSL and re-engage in a straighter path. It like when you’re parked between two cars and have to correct – you can’t do much inside the space – you have to pull back out and reposition yourself straighter.
- WHEN YOU REDIRECT – do so with the STYLET IN PLACE so you don’t clog the Tuhoy with tissue. The constant pressure of air/saline can protect the Tuohy from clogging as we do the procedure, but we’re not holding constant pressure as we’re repositioning, so the needle can clog. Ensure a cleared out needle before re-attaching LOR syringe
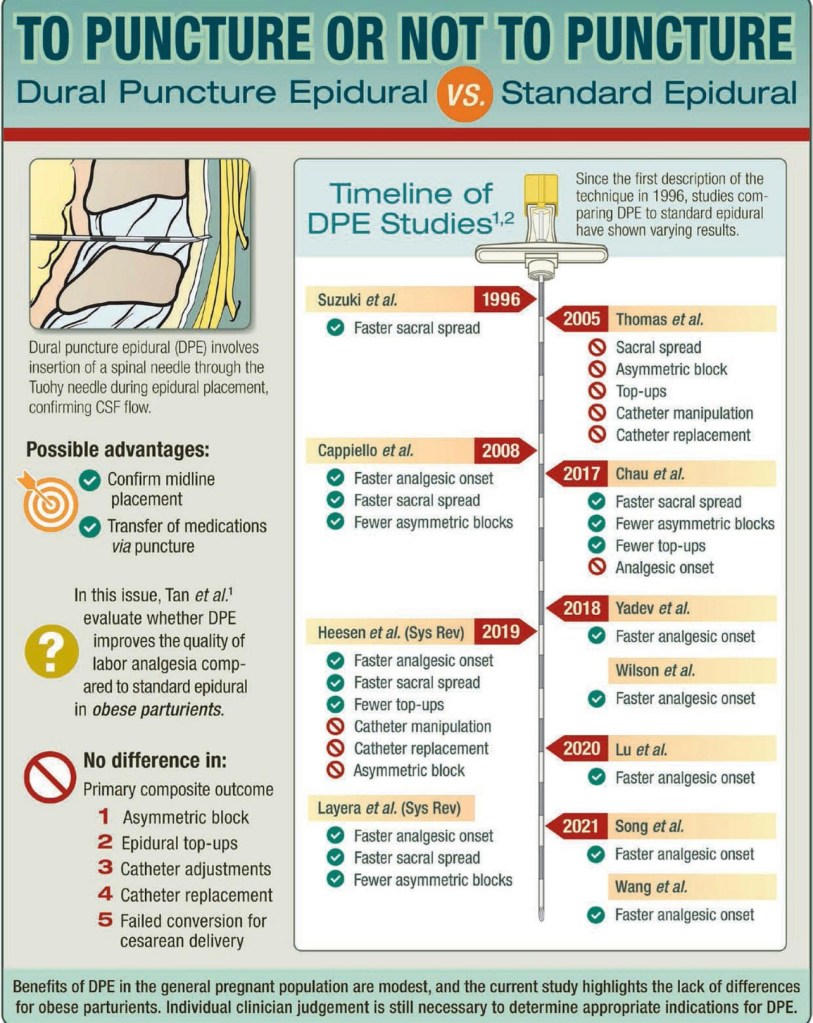
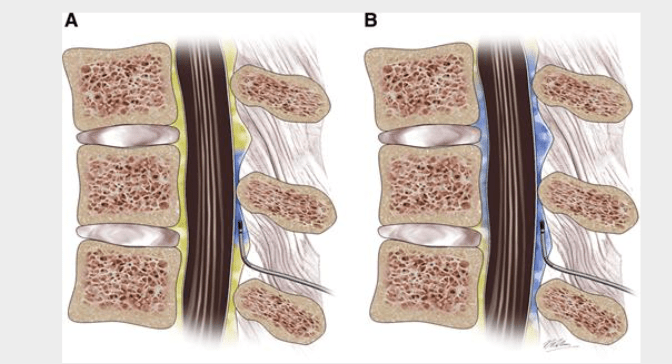
- *If having a lot of difficulty with epidural, or unsure if you really lost resistance, as some epidural spaces are less compliant and don’t have a dramatic, convincing LOR – you can always do a dural puncture epidural (DPE) for confirmation. Just like performing a CSE, when you get LOR, all you have to do is put the Tuohy CSE-compatible long spinal needle through to the intrathecal space to puncture and confirm CSF, which should also confirm your Tuohy placement in the epidural space. No spinal dose administered in DPE, but the puncture creates a tiny conduit for some LA to spread intrathecally and provide more even coverage.
- TIP: when performing a DPE or Labor CSE (tiny spinal dose): when placing a spinal needle to look for CSF – try to leave a drier epidural space prior to dural puncture. Feel free to use saline for LOR but just don’t push the whole syringe of saline into the epidural space right away. If the epidural space is drier before dural puncture, you have more assurance that the clear fluid coming back through the spinal needle is CSF and not saline from the epidural space. Since the CSE spinal needle is so long, it’s usually a much slower drip than the normal shorter spinal needles. For DPE you just puncture, confirm csf, and pull out the spinal needle. For labor CSE you admin ~1cc of 0.25% isobaric bupi (You won’t get the usual swirl we see with dextrose-mixed hyerbaric solution on aspiration.) After spinal needle is removed (DPE or CSE) THEN feel free to dilate the space all you want with saline before threading the epidural catheter. Since this is such a small dose we aren’t as concerned with epidural space expansion compressing the spinal canal and pushing the spinal dose higher, the way a surgical CSE with hyperbaric 0.75% bupi could with ++saline dilation.
- *USUALLY can just hub CSE spinal needle in Tuohy. The spinal needle only comes out 2cm or so past the end of the Tuohy when hubbed – and you want to ensure you’re actually intrathecal.
- The CSE kits have compatible Tuohy and Spinal needles – you have to use both together and NOT mix and match. The CSE kits are not all interchangeable, you must use that specific Tuohy with that specific spinal needle so they fit each other.
- This ensures the spinal needle: 1) fits through that gauge Tuohy, and 2) is long enough to come out the end far enough to reach the intrathecal space.
- The regular spinal kit needles are not long enough to reach the end of a Tuohy needle. You need the CSE-kit-extra-long spinal needle.
MORE EPIDURAL PLACEMENT TIPS
Checking Your Placement:
- Think you lost? Felt a change in resistance? – disconnect LOR syringe and stylet Tuohy to clear it – no CSF? try to thread catheter. If you cannot thread, probably not in epidural space yet, and can feel more comfortable continuing to advance Tuhoy.
- Feel like your Tuohy is deeper than it should be, and you’re afraid to keep going and wet tap? Again, clear your Tuohy with stylet to make sure the resistance you feel is from the ligaments, and not a clogged Tuohy. Once it’s cleared, try to thread catheter to make sure you’re not in the space – cant thread? proceed.
- R/O Wet Tap? If using saline LOR: saline may drip back out of the Tuohy when you disconnect LOR syringe, but should stop after a few drips and would probably also be cold. CSF would probably feel warm, and be a continuously fast drip.
- If it’s a fast drip, plug Tuohy with thumb and don’t allow a lot to drip out —> spinal headache if it’s CSF. But sometimes the saline comes back out as a brisk drip, too. Some epidural spaces are less compliant than others..
- If you’re questioning it – I’d just cover the tuohy with my thumb and wait a few seconds – if it’s saline in epidural space, it should settle with gravity and after a few seconds when you release your thumb, saline shouldn’t keep dripping out. If it’s csf though, it’ll keep pouring out from the pressure gradient of ICP to atmospheric pressure.
- If it’s a fast drip, plug Tuohy with thumb and don’t allow a lot to drip out —> spinal headache if it’s CSF. But sometimes the saline comes back out as a brisk drip, too. Some epidural spaces are less compliant than others..
Avoiding Intravascular Catheters
- IF you hit a vessel in the epidural space with the Tuohy (after LOR) – they’re hypercoagulable in pregnancy – it’ll be OK. Epidural catheters also thread into vessels all the time – its ok – it’s only a problem if they have a coagulopathy/blood thinner and can’t form a clot (epidurals contraindicated anyway).
- Also muscle is very vascular, and there are vessels on either side of the ISL – if you’re getting blood back in the tuohy – you’re a little off midline. *Clear the tuohy out well with stylet- blood will easily clot & clog your Tuohy, impairing your tissue feedback. You wouldn’t even know if you had a wet tap bc no csf would come back through a clogged Tuohy.
- Also – don’t panic when you first see blood in the tuhoy – when you hit a vessel with an 18/17g Tuohy – either in muscle or in the epidural space – you will get a RIVER of blood back in your LOR syringe – it *pours* back. It’s especially pronounced if you use saline for LOR. It looks very dramatic, and the first time people see it they’re like OMG this is a crime scene. But don’t worry – your pt will be fine. Just careful with those glass syringes – once they get blood in them they can get a little sticky from the RBCs and lose their fricton-less glide….so clear out your Tuhoy well with the stylet, and flush your glass LOR syringe out with some fresh saline (the plastic LOR syringes are fine – just the glass ones seem to get a little sticky with blood)
- When I get into musculature before LOR and hit a vessel, I usually just mention to the pt they might feel like there’s a little bruise/soreness on their back even if they don’t see a bruise – (there may be a tiny hematoma in the muscles on the side of the ISL)
TIPS TO AVOID & MANAGE IV CATHETERS
- Helps to dilate space with remainder of saline (7-10cc) through tuohy prior to threading catheter
- [** Especially with the Braun stiff catheters: the most helpful thing I’ve started doing with these specific catheters is to bend the tip of the catheter before threading it through the Tuohy. Bend those first few mm where the blue tip meets the clear catheter into a little candy cane shape (it’s a little tough to do bc its so small, but worth it – I use my thumbnail..) Now when the tip comes out of the tuohy it’s much less stabby and sharp, and should bend away from any obstacle (blood vessel) vs pierce right through it. If I somehow still get an IV catheter despite the bend (and saline dilation), I’ll do all of the listed things below, and re-thread it with the bend facing a different direction to try to thread it in a different direction away from whatever vessel I previoulsy hit.]
- Thread gently, don’t push hard against resistance, try to gently thread past, can try gently twisting the catheter. Be patient.
- Don’t thread during a contraction (~300-500cc autotransfusion back to systemic circ with each cxn = higher venous/bastons plexus pressure, also higher intra-abdominal pressure theoretically compressing epidural space, while engorged veins take up more space in the epidural space)
- IF CATHETER INTRAVASCULAR – DO NOT PULL CATHETER OUT THROUGH TUOHY – IT can SHEAR and NEEDS SURGICAL REMOVAL.
- IF you’re IV – make sure – remove tuohy and pull catheter out to appropriate skin depth (this hopefully pulls it out of the vessel), flush catheter with saline, aspirate, flush with saline, aspirate. If no longer getting frank blood back, maybe just blood-tinged saline – you’re out of the vessel – proceed to test dose.
- IF test dose positive OR you keep aspirating blood – NO WORRIES!! – just look WHERE LOR IS, and remove Tuohy over catheter. Then remove catheter. Flush your catheter free of blood in your tray with the yellow luer-lock apparatus. Now you can just reinsert Tuohy in the same spot (it’s already numb! The pt will love you for not stabbing them again with the burning lido syringe of doom).
- (There’s a lot of dogma about always automatically changing spaces if a catheter goes IV – it makes no sense to me – the catheter can thread in any direction, and the 5+cm of catheter we initially thread into the space can hit a vessel anywhere, you could theoretically even hit the same vessel twice from 2 different spaces. So I think this is silly. With additional saline dilation, and a very gentle thread, the risk of IV catheter should be greatly reduced. The local lido is the most painful part of the procedure for most people – if you can avoid sticking her again, I think it’s worth trying. Plus some epidurals are difficult enough to place in one space, much less two)
- SO INSTEAD, just reinsert Tuohy 1 cm or so before your LOR, and re-engage in ligamentum flavum, lose resistance again, and this time REALLY dilate the space through the Tuohy with more saline (another ~10cc) – the RN can grab you a sterile saline vial or squirt an extra saline flush into your tray. RE-thread your catheter and voila! If the catheter tip has a little natural bend, try inserting it pointing in a different direction this time. Remember to pull the catheter back to the appropriate skin depth before aspirating again. The odds of you hitting the same vessel twice are pretty slim. If you do – then sure, change spaces.
- You’ll likely get some blood-tinged saline on aspiration after dilating the space with so much saline after having a known vessel puncture – but there’s a difference between bloody saline aspirated, and frank blood aspirated – examine it in the syringe and you’ll see the difference. Blood-tinged saline is expected after a vessel puncture. Proceed to test dose.
- Also, after putting 10-15cc into the epidural space, if you change a level after an IV catheter, it’s possible you’ll encounter a little saline already in the epidural space when you lose resistance – this isn’t a wet tap – you’re just hitting the little pool of saline you just placed, and it shouldn’t pour out like a wet tap would.
- Also if you have a known vessel puncture – it’s possible a wee bit of test dose epi can still go IV, and test dose might show a little HR uptick. If everything else looked good, and no other s/s IV or intrathecal lido – I’d leave it and run the pump. If she never gets comfortable, that’s good evidence for an intravascular catheter, as LA goes IV and not into the epidural space. But regarding questioning an IV epidural catheter – if worst case, you bolus up to 10cc pump solution (we have 0.1% bupi aka 1mg/cc), then run the pump at 10cc/hr, that’d be a total of 20mg bupivicaine IV in the first hour. 20 mg IV bupi isn’t going to hurt her or cause LAST – but it WILL NOT touch her labor pain. She will call you back in pain long before she has any LA toxicity risk. So..after a KNOWN vessel puncture – if catheter re-threaded easily and there’s no blood aspirated and it looks good – but the test dose is just a little suspicious for a little bit of IV epi….I’d take it with a grain of salt, let it ride for a little, and see how she feels in ~20-30 min before replacing the catheter. If it’s not in a vessel, she should have relief.
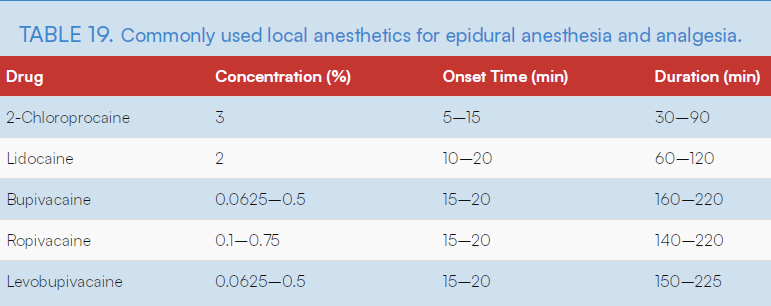
Epidural Anesthesia and Analgesia
Epidural Anesthesia During Labor and Delivery
ULTRASOUND FOR NEURAXIAL
ONLINE RESOURCE:
- ultrasounds useful to find midline in obese or technically challenging pts:
http://pie.med.utoronto.ca/OBAnesthesia/index.htm
Obstetric Anesthesia: Perioperative Interactive Education, PIE, Mount Sinai Hospital, Toronto
HH PHARMACY FORMULARY FOR EPIDURAL PUMPS
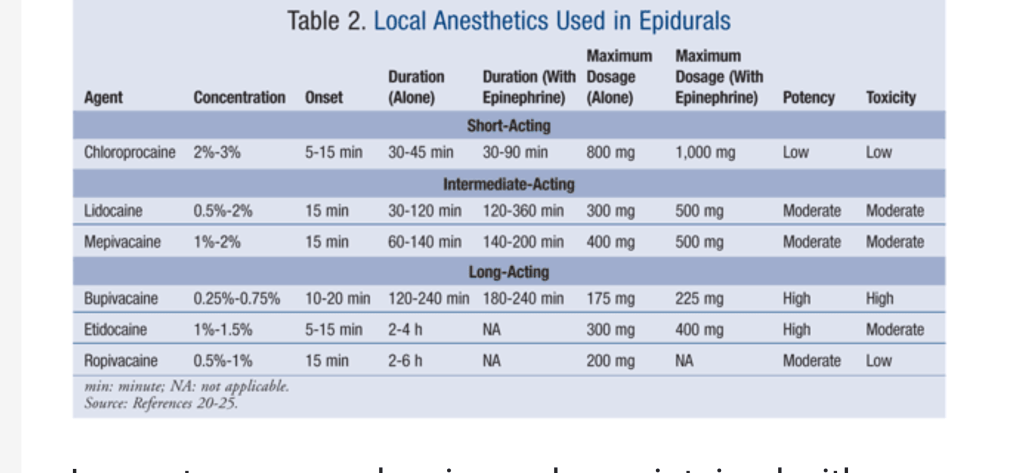
The pump solution our pharmacy supplies is 0.1% bupivicaine with 2mcg/mL fentanyl.
- Fentanyl provides a more dense sensory block, without increased motor block:
- lipophilic – diffuses easily and rapidly across dura to act on Dorsal root ganglions & spinal nerve roots traversing epidural space, as well as across dural cuff into CSF to work act on opioid receptors on the spinal cord.
- works on different receptors than LAs. LAs = Na+ channels to inhibit action potentials – can cause both sensory AND motor block, Fent = Opioid receptors – no motor bock..
- Fent added to LA gives LA-sparing while providing adequate pain control and preserving motor function. (mom has to be able to push)
Timing of Labor & Labor Epidurals
NPO Guidelines:
- Clear liquids are required once she is IN LABOR, and also after epidural placement. Technically, no prior NPO status is required for labor epidural placement, however after placement she can only have a Clear Liquid Diet.
- So situations can arise where she can have eaten right before epidural placement, and we would place it (ex: say a pt lives near to the hospital and was eating dinner when her water breaks and she immediately starts having painful contractions – she comes right to the hospital but ate 20 min ago.. we can still place her epidural right away, and do not have to delay pain control bc she just ate dinner). This policy allows for this kind of situation to occur.. labor is often unplanned, and especially in multips it can progress very quickly, so it’s hard to make women NPO or CLD for any amount of time prior to onset of labor/arriving unexpectedly to the hospital and requiring an epidural. HOWEVER this policy DOES NOT MEAN anesthesia is allowing patients to knowingly eat solid foods in labor while in the hospital!! Once they are in labor in the hospital – CLEAR LIQUIDS ONLY, so the majority of our epidural patients are already on clears, bc they are already in the hospital in labor.
- Once established to be in labor, women can only have clear liquids from that point on until delivery – this is both an ACOG and ASA guideline.
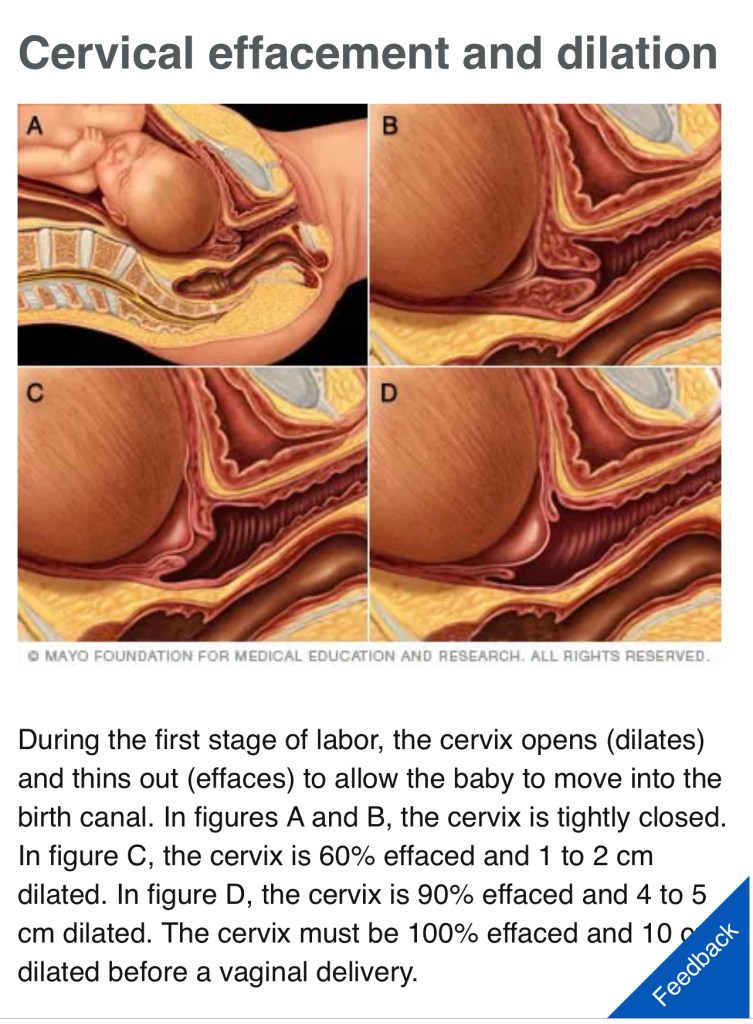
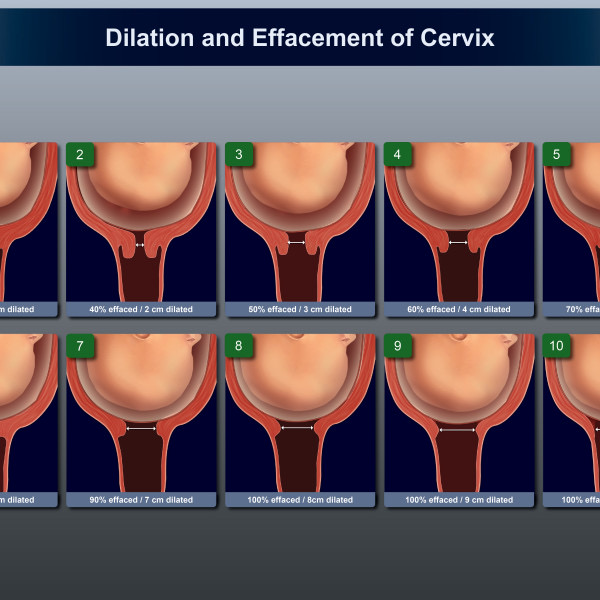
- SO when women come into the hospital IN LABOR – defined by ACOG as “uterine contractions resulting in cervical dilation or effacement” **NOT defined by ROM… they are on a clear liquid diet.
ACOG Guidelines on oral intake in labor:
Approaches to Limit Intervention During Labor and Birth
ASA Guidelines on oral intake in labor:
Statement on Oral Intake During Labor
Department Guidelines on Neuraxial: spinal/epidural & PLTs/labs
STAGES OF LABOR
3 Stages of Labor:
- Stage 1: Dilation —> 10cm
- ( T10- L1 sensory level needed to cover uterine cxns and cervical dilation)
- Stage 2: Pushing (F+P)
- T10 level PLUS S2-S4
- Stage 3: Placenta delivery
Stage 1:
- Early: 0-6cm……ouch
- Active: 6-8 cm ……OUCHH
- Transition: 8-10 cm……M%@#$F#@!*$
Stage 2:
- FULLY DILATED & PUSHING BABY OUT
Stage 3:
- Placenta comes out


Labor Timing:
- Primips (G1P0) often have longer, slower labors. Everything is slowly stretching for the first time.
- Multips (G1+P1+) often progress faster. Every labor after the 1st one can move VERY quickly. Esp after ROM. Not always the case, but always possible.
- Rupture Of Membranes:
- SROM = spontaneous
- AROM = assisted
- PROM = premature
- PPROM = preterm premature
- Once membranes ruptured:
- Labor usually gets more intense for everyone. Cxns become more painful and close together.
- *Esp for multips: delivery can be VERY fast afterward.
- Fewer cervical checks performed after ROM to reduce infection risk. (So what you see on the epic grease board may not be at all up to date) Trust what the nurses and pts tell you about where they are in labor.
- Sometimes ROM happens just before baby is expelled, esp in multips (a gush of water and BOOM baby comes flying out), so ROM isn’t always a meaningful indicator of labor progression in multips.
EPIDURAL TRIAGE
Ex) 2 requests: primip at 4cm w intact membranes who requested first, and a multip with ROM requested a few minutes after – I’m doing the multip first. Not much should change in 30 mins with the primip. But the ROM multip’s condition might change in 30 mins to the point where she cannot sit still for the procedure, or worse, has to start pushing unmedicated.
Normal Epidural Timing
- It’s never “too early” to get an epidural. It can be placed whenever mom wants it.
- The cervical checks listed on Epic grease board are NOT necessarily up to date. After ROM, they check less to decrease infection risk. (Eg: If a multip is complaining of pain and her check is listed at 2/50%/-3 … go see her! She could have progressed rapidly since her membranes ruptured – Don’t believe that chart!)
Early labor: 0-6cm (T10-L1)
- usually easily tolerated, pt can sit still and position themselves
- Plenty of time to assess epidural effectiveness & replace if ineffective so we have a good working catheter in case of an emergent c/s
Active Labor 6-8cm (T10-L1–>S2-S4)
- Mom getting VERY uncomfortable. Be efficient and patient with her moving during contractions. Communicate well with mom and work efficiently between contractions. Regroup & reposition between EVERY cxn.
Transitioning Labor 8-10cm. (T10-L1—>**S2-S4**)
- Mom needs an epidural +/- an exorcism.
- Somatic pain is dull pain from bones/joints/tendons/muscles – similar to visceral pain, this is the pain felt from s2-S4 carried on the pudendal nerve.
- Labor CSE is best for this stage as it will offer more reliable S2-S4 coverage and provide faster, more reliably even relief than a standard epidural, to get them comfortable in time to start pushing.(will discuss labor CSE next)
- Perineal stretching, sacral and pudendal nerves: S2-S4 origin **
- Do not judge her for what comes out of her mouth. She is in blinding, bone crushing pain. Do EVERYTHING possible to give her relief, no matter how frequently she squirms – can even try a side-lying epidural/cse if that’s all they can manage. Be patient and don’t get flustered by position changes – stick with it and work between contractions.
- I’ve done these laterally before if mom is so close to pushing she can’t even sit up or change positions. Usually she can still round out her lower back while lying laterally, and the nurses can help support her in the fetal-ish position to open up her spaces a little. It’s worth trying, and a clutch skill to develop.
- Pressure sensations later in labor with otherwise working epidural are normal, especially when pushing, but epidural should take away sharp pain. Block should not be so dense that mom loses significant motor function (not the goal at least). She should be able to push.
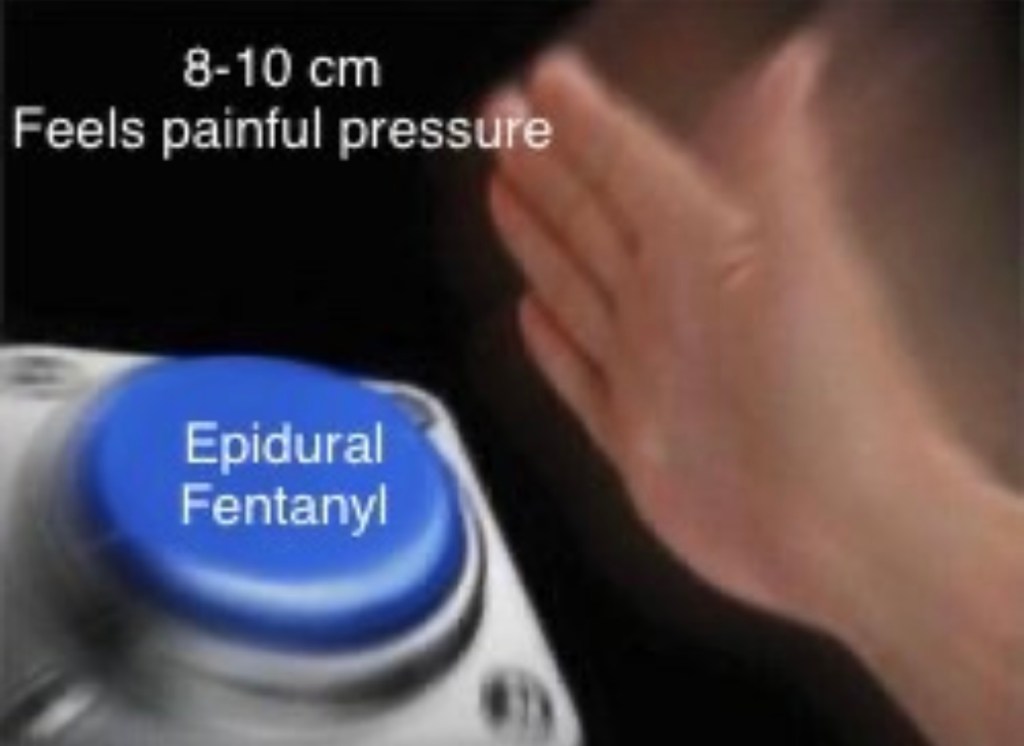
- If >7cm and progressing, and pressure is best relieved by epidural fent: 50-100mcg.
- Tip – before giving epidural fent alone (1-2cc) in late labor (eg: no sharp pain, just vaginal/rectal pressure), dilute it with ~10cc saline so it spreads well.
Adding 50-100mcg Epidural Fentanyl
- Save it for LATE transitioning labor when the pressure on S2-S4 is brutal, and high LA doses will give too strong of a motor block to allow her to push* especially for primips, the first time pushing is the hardest – the ligaments of the pelvic outlet are stretching out for the first time – it is WORK. Mom needs all the strong motor function she can get.
- There is a theoretical risk for higher fetal fentanyl transfer: it’s closer to delivery & epidural space is vascular, some systemic uptake does occur… HOWEVER, I cannot find, nor can my colleagues find, any good evidence that epidural fent decreases APGAR scores, or that the fentanyl/lipophillic opioid transfer (while totally possible) has any actual clinical significance in the form of poor neonatal outcomes when used as a single dose; [prolonged, repeated, high dosing, of course, has longer context-sensitive Et1/2]. Additionally, we give 100mcg epidural fent routinely for epidural conversions for C/S for fetal distress, to create a more dense block quickly, and we have no worse outcomes. We do, however, hold the hydrophillic epidural duramorph until after delivery to prevent fetal transfer, as morphine has been shown to have associations with poor feeding and worse neonatal outcomes/prolonged resp depression 2/2 its long duration of action and active metabolites.
Why give Epidural Fentanyl?
- Pressure sensation (thick A-beta fibers, dorsal lemniscus pathway) is nearly impossible to block – women feel it under spinal anesthesia when baby comes out – they feel intense, uncomfortable pressure despite the spinal block being so heavy she can’t even move her legs. So for pressure sensations (A-Beta fibers), blocking sodium channels with LAs can only do so much…and in a LABOR setting, we ideally don’t want high enough LA doses to impair pushing/motor function.
- Epidural analgesic doses are not as dense as a surgical block- nor should they be – mom should be able to move her legs and have muscle control to push.
- Uterine contractions T10-L1 are well blocked. That sharp pain (A delta type 1&2), and a lot of the cramping (visceral – c-fiber) pain is blocked well with an epidural. By the time women are transitioning and the fetal head is descending through the pelvic outlet into the perineal vault – it’s literally stretching her bones apart, stretching her perineum and vagina apart, stretching pelvic ligaments and tendons to their maximum capacity. The sharp pain is blocked by LAs bc it’s carried on type 1&2 A-delta fibers but the *incredible* pressure carried on thicker (A-beta) are harder to block.
- Fent will offer 2nd mechanism of relief by diffusing across the dura surrounding spinal nerve roots as they exit the spinal canal, and hitting spinal nerve root opioid receptors instead of only relying on the Na+ channel blockade from LAs. Now two types of receptors are working to stop the pain sensation, since LA can only do so much..
(Minimal fetal uptake with epidural fent – don’t even worry about it. Site of action is diffusing quickly across dural cuff due to lipid solubility to hit opioid receptors on spinal cord and spinal nerve roots. Not the same systemic uptake as an IV dose, and significantly more effective for labor pain with less fetal transfer than IV – everybody wins.)
Epidural Fentanyl Produces Labor Analgesia by a Spinal Mechanism

Assessing coverage
Thoracolumbar (T10-L1) coverage & Sacral (S2-S4) Dermatomes needed for labor analgesia:
- Gently poke different dermatomes to assess coverage/sensory loss. Shouldn’t feel sharp sensation, everything should be dull.
- T10-L1: belly button to bikini line 👙
- S2: medial calves. (Leave it at that – lol please don’t test S3, S4 – it’s on the butt)
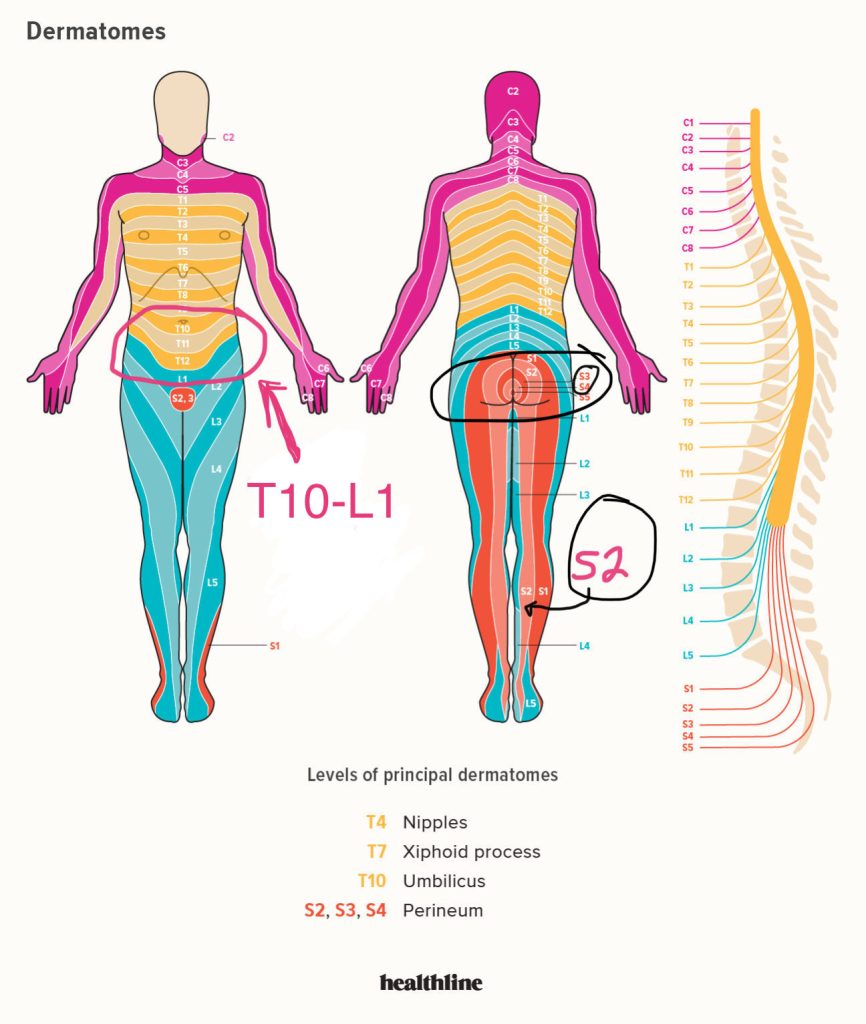
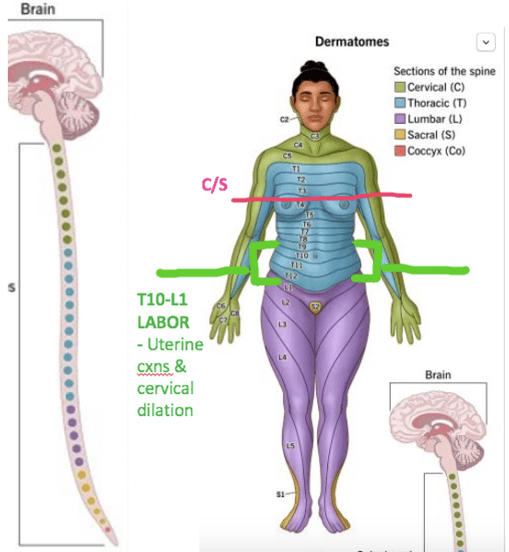
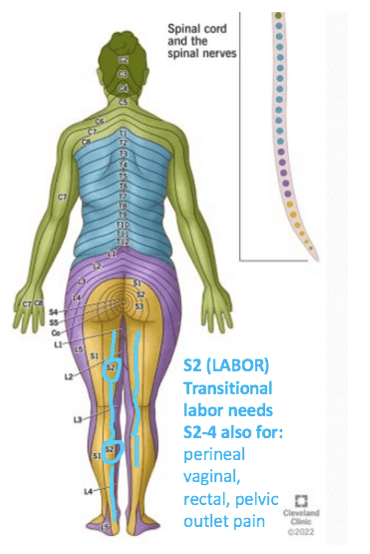
- Uterine contraction pain, and cervical pain = T10-L1
- Perineal/pushing/later labor fetal descent pain = S2-S4
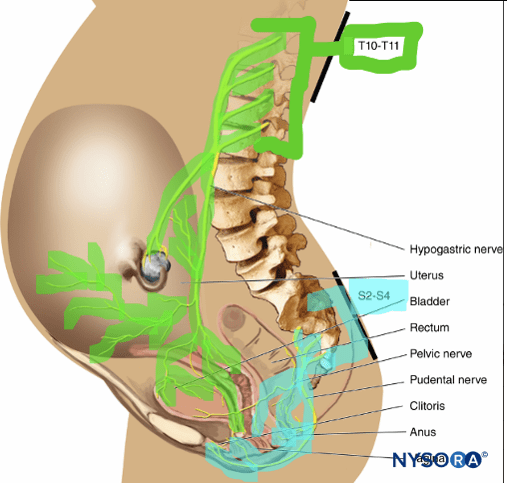
- CIRCUMFERENTIAL EPIDURAL SPACE SPREAD is needed to BLOCK EACH SPINAL NERVE ROOT AS IT EXITS THE SPINAL CANAL THROUGH THE EPIDURAL SPACE.
- This is why DILUTED, high VOLUME epidural doses are needed for adequate spread and complete coverage – with enough LA to cover SENSORY [C, A-delta, A-beta fibers], but not a high enough concentration to knock out MOTOR [A-Alpha] fibers.
- Once you have established fluid communication channels throughout the epidural space, concentration can be titrated up to pt response/relief, with more assurance it will be evenly distributed.
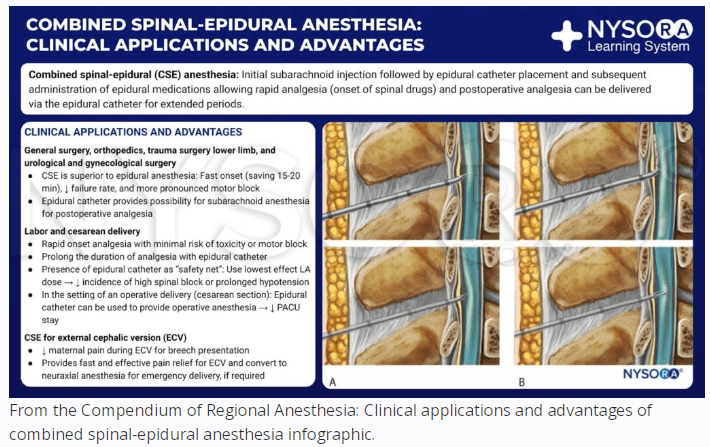
LABOR CSE
Labor Combined Spinal-Epidural is when we do a CSE, but instead of giving a hyperbaric PF 0.75% (7.5mg/mL) bupi dose for a surgical spinal block, we give just a tiny fraction of that dose – 1-1.2ish cc isobaric 0.25% PF bupivicaine (2.5mg/mL) into the CSF. (2.5-3ish mg)
- IF you’re using 0.5% bupi, then the cc dose for 2.5-3mg would be 0.5cc-0.6cc, respectively, but I’ll refer to it in 0.25% bupi doses bc thats what I use/have available, and you can adjust to whatever you have on your own unit..
- [I’ve tried just 2.5mg (1cc) but a few pts didn’t get comfortable, and when I upped it to 3mg (1.2cc), I haven’t had a problem since. So just observationally the 3mg (1.2cc) seems to work better. The ED95 dosing is reported as only 1.66mg BUT* with the addition of 15mcg fent. I just use plain bupi bc finding ppl to waste fent with me at 3am is another extra annoying step…SO if you want to add fent, go for it, and you can come down bit on your bupi dose. And in a pt who you don’t want to give a rapid sympathectomy to (eg: PreE w SF..) intrathecal fent ~20ish mcg alone with no LA is a great option for faster pain relief than a standard epidural, but without the vasodilation and BP drop.]
- Then we DO NOT give the usual 6-10cc bolus loading dose. We just start the pump.
- So 2.5mg-3mg bupivicaine into the CSF to give the pt an almost-immediate, RELIABLE, EVENLY SPREAD sensory block, without the massive sympathectomy or motor block of a surgical spinal dose.
- (if you have a pt who is transitioning quickly she might not have time for: 1) a normally dosed epidural to kick in and provide relief, 2.) ensuring/troubleshooting the epidural so it sets up evenly enough to cover the S2-S4 innervation which is harder to block well and will transmit pain from pushing)
- The CSE offers rapid, reliable, evenly spread relief.
- if you’re concerned about BP in fragile pt you can also just give ~20 mcg fent spinal dose for pain control without any spinal sympathectomy at all, or motor block (bc it’s only fent.) May cause pruritus but once delivery is over, we have meds for that (Nubain).
- The spinal dose should provide sensory pain relief without profound motor block for at least 1-2hrs, while the continous pump gtt in the background slowly sets up.
- The small 2.5-3ish mg isobaric bupi dose isn’t going to cause a high spinal – you don’t have to worry about positioning. You can keep her sitting up for the epidural test dose (this isn’t hyperbaric – it’s isobaric and not moving much) It’s such a small dose. But it is a LIFESAVER in transitional labor (8-10cm) when you may not have time for a traditional epidural to set up well enough to provide the sacral S2-S4 relief she desperately needs for this phase of labor.
- Also this isobaric 1.2 cc 0.25% bupivicaine won’t give you the increased resistance through the long CSE spinal needle that the 0.75% syrupy hyperbaric bupi we use for spinals will.
- After* placing the spinal dose, I still dilate the space with saline through the Tuohy before threading the catheter and test-dosing.
- again – very small 2.5-3 mg dose – I’m not worried about “pushing the dose up too high” with dilating the epidural space, and
- But, because there can still be HOTN 2/2:
- 1) sympathectomy 2/2 vasodilation – nothing compared to a surgical spinal dose
- 2) compounded by decrease in catecholamines 2/2 pain relief..
- NO EPIDURAL LOADING DOSE – just start the pump at 10cc/hr without any loading dose at all, and the saline you used to dilate the space may help the gtt slowly spread and set up more evenly, so by the time the spinal dose wears off, she has a nice even epidural block set up.
- Just for the logistics of this: Our epidural kits don’t include a CSE dose or equipment. We have to bring in and drop a sterile CSE kit (Tuohy & spinal needle combo) onto the field (or drop a compatible spinal needle to our kit’s 18g Tuohy.) I also have to drop an extra 3cc sterile syringe onto the field to draw up the 0.25%bupi into. So to do this alone, I draw up the bupi from a new sterile vial outside the room before coming in, and gently sterile squirt it into one of the wells in my epidural kit in my sterile field. Then once I’m sterile, I draw up that spinal dose first in the extra 3cc syringe I’ve dropped on the field, using the filter thing. I then put that spinal dose syringe in a designated location (I put it in the little removeable betadine tray we never use) so I don’t confuse it with a lido syringe or anything else. You can also drop a 5cc syringe instead and pick one for spinal one for local so you don’t have 2 x 3cc syringes that are easy to confuse. Do whatever makes it idiot-proof for yourself, bc when we’re doing these half dead at 3am we need things to be obvious.
Pros/cons Labor CSE
Pros:
- Fast, reliable S2-S4 coverage with minimal motor block and much less sympathectomy than surgical spinal. (Covers T10-L1 too, but covers S2-S4 more reliably and much faster than normal epidural)
Cons:
- More rapid sympathectomy onset from intrathecal dose may not be tolerated in HTN pts (PreE, HELLP, gHTN)
- Theoretically, spinal dose can mask a poorly-working epidural. Spinal dose makes assessment of epidural spread and coverage impossible to assess until after spinal dose wears off. Theoretically, this could lead to situation where stat c/s is needed and we have only the small spinal CSE dose in place, then we dose the catheter but can’t assess effectiveness and evenness of coverage – then the spinal dose wears off bc it’s so small and we’re left with an epidural that secretly doesn’t work during a c/s.
With that being said, many institutions do labor CSEs for EVERY epidural, regardless of labor stage or maternal obstetric hx or comorbidities. There is no documented problem of Labor CSEs failing in a C/S at any more than regular epidurals. In fact, CSEs report lower epidural failure rate, probably from the midline assurance that a dural puncture provides. There is a valid argument that when you do a CSE, the CSF flow from a dural puncture assures more midline placement of the Tuohy needle, and should provide a more midline catheter thread and therefore a more even, effective epidural block. Additionally some anesthesia providers do a dural puncture for every epidural (with CSE spinal dose or not) just to confirm midline placement.
Who isnt theoretically ideal for a CSE, some might say..
- Women who have never delivered vaginally before (no proven pelvis.)
- If they are unable to deliver vaginally and need a c/s, the CSE could theoretically mask a faulty epidural catheter.
- PreE: rapid sympathectomy may not be tolerated, as spinal onset is faster than epidural onset. Can do dural puncture to prove midline placement without spinal dose. Also she needs a good proven epidural catheter – PreE has higher rates of C/S and this is an airway we do not want to instrument.
- ANY difficult airway, MH history, anyone who should NOt be intubated or placed under general anesthesia.
- …. Bc if the epidural fails that’s what we have to do
- GDMA, fetal macrosomia, or other reason she might not be able to deliver vaginally and may need a C/S – I’d rather not do a CSE and just do a straight epidural so I can assess how well the epidural works, should we need to convert it to a surgical level for a c-section.
- The best case labor CSE is a multip with prior vaginal delivery who is progressing quickly – thought to be 7-8cm – Especially if membranes ruptured on multip and > 7cm – they may move very fast through labor stages.
Top-offs and Troubleshooting
Disclaimer: Everyone has their own little voodoo recipe for top-offs they swear by, whether it make sense or not, but as long as the general principles are followed, and we’re not giving a surgical-density block, theres no real 100% right or wrong top-off concentration (within reason).
- ASPIRATE catheter before pushing any meds through. (no heme does NOT eliminate possibility of IV catheter, but + heme is IV)
- EPIDURALS ARE VOLUME BLOCKS.
- EVERY LA DOSE CAUSES SOME DEGREE OF SYMPATHECTOMY, dose-dependent, and can cause a decel by dropping MAP-dependent placental perfusion.
- DILUTED* volume LA solutions provide more EVEN spread, without dense motor block and profound sympathectomy.
- You cannot achieve pain relief with an uneven block. You can not relieve pain without EVEN SPREAD.
- Manual top-offs should provide higher pressure injection than epidural pump bolus, hopefully achieving better spread. Even if you top-off the same concentration LA as pump solution, you hopefully can spread it better by manual bolus.
- DO NOT BE AFRAID TO REPLACE A NON-WORKING CATHETER AFTER FAILED TOP-OFFS!! We need a working epidural catheter to avoid GA/intubation in high risk OB airway in case of emergency c/s.
Diluted, higher-volume top-off augmented with saline decreases concentration and decreases likliehood of profound sympathectomy. Adequate analgesia can be achieved with less than 0.1% bupi (HH pump solution). In fact, many institutions use 0.0625% bupi for L&D. Giving a higher volume of less concentrated solution will often achieve better analgesic coverage with less hypotension, and less motor block.
Some Viable Options for Top Offs Based on Assessment:
LOOK AT CATHETER. It might be falling out.
SHARP PAIN – BILATERAL:
- Inadequate block spread & density: may need slightly HIGHER concentration
- Ask if catheter EVER made her comfortable:
- If not, lower threshold to replace catheter, can pull catheter back to (hopefully better position) and attempt a second loading dose via manual push (4cc 0.25% bupi, 6cc saline = 0.1% LA (same as pump solution). If this top-off fails again, REPLACE catheter.
- If she was* comfortable bilaterally, but now feeling increased pain, there’s more confidence that catheter works, but she may just need:
- 1) a little extra block density
- or 2) a little volume & gravity spread downward through the full T10-L1 (uterus and cervix) spinal nerve roots, and S2-4 roots (pudendal nerve- perineal pain)
- Can still pull catheter back, if possible, in attempt to pull into more midline position
- Try: 6cc saline, 4cc O.25% Bupi (= 10cc volume with ~same % as pump solution 0.1%) + (2cc lido with 2cc saline (4cc 1% lido) for faster onset to block, and a little stronger block density than pump solution)
- = ~14cc total – should give good spread to reach areas not covered.
SHARP PAIN – ONE-SIDED
- = poor/uneven spread : Needs DILUTE, high VOLUME dose for spread.
- Pull catheter back if possible
- Give large volume ~15-20cc very** dilute solution to spread block better. Use 3cc syringe for higher pressure and better spread.
- This volume should mix with that more concentrated, unilaterally pooled LA, and spread it out more evenly through the entire epidural space.
- Once the unblocked side starts feeling better from having the dilute LA more evenly spread, you can dose a higher concentration and know it’ll spread more evenly through better established bilateral communicating fluid channels.
- If this is a pt who does not tolerate additional sympathectomy, you can just use 20cc saline to spread the existing LA in epidural space around more. You’ve now increased volume spread without giving any additional concentration.
PRESSURE
- if* sharp pain is evenly controlled, then pressure is normal and not indicative of a problem with the catheter. This is typically described as rectal/vaginal pressure, and usually occurs later in labor, as fetal head descends into pelvis/perineal vault/vagina and starts stretching tendons/ligaments/pelvic outlet.
- 50-100mcg epidural fentanyl
- 1) it helps immensely with pressure sensation (A-beta fibers) by working on Mu receptors vs only Na+ channels
- 2) large, concentrated doses LA will impair motor function and can impair ability to push (which will be happening soon). Give fentanyl in 10cc saline to spread dose evenly through epidural space. 1-2cc alone straight from vial may not spread as well and reach the S2-S4 nerve roots causing all of this pressure.
- 3) can add 2-3cc lido to this just for a little extra block density.
- I pretty much always given the full 100mcg bc it works really well, and then I don’t have to waste it :-)…
Pain post-delivery with repairing a tear
- I usually given a solution of 10cc 1% lido with 1cc bicarb, or 10cc chloroprocaine for a fast, dense block…bc actively getting sutures in your vagina that isn’t adequately numb – OMG just kill me (and yes they can inject local as they work but OMFG that would hurt so much – no thanks.. if it were me – just bolus my epidural)
When to Replace the Catheter?
NO RELIEF, or LIMITED RELIEF despite 2+ top offs?
- This means the catheter not only isn’t helping the pts pain, but likely won’t work if we have to convert to a surgical level for a stat c/s and bolus the catheter. Working catheters allow us to bypass GA.
- My final Hail Mary is 5-7cc lido (1% or 2%) w 1/2cc bicarb. This is what we dose an epidural with for c/s – if the epidural is still not working with lido, it won’t work in an emergency with lido, and needs to be replaced. The bicarb will give you a quicker idea of its function, as the block should set in faster.
- Reassure mom the replacement usually is less painful than the initial placement bc some of the dermatomes in the lumbar region back are often more numb.
Physiologic Responses & Comorbidity Considerations for Dosing/Top-offs, and Sympathectomies
- Prior to top-off , consider tolerance of initial sympathectomy during first epidural loading dose, or in any previous top-offs. Check history and go easy on HTN (preE, HELLp, gHTN) pts – placental perfusion is MAP-dependent and a large drop in BP can impair fetal perfusion and send the fetus into a terminal decel. (via heavy initial epidural loading dose or heavy top-off)
For cardiac patients, uncontrolled HTN patients, pulm HTN:
- Gentle onset to sympathectomy w/ slower, more controlled dosing. Lessens initial BP drop by allowing more time for cardiac compensation. Don’t give 10cc loading dose – give 5 or so and she can always have a bolus from the pump if it’s well tolerated and requiring more LA. I like to dilate the space with all of the saline I have ~10cc so the smaller dose spreads better and also is more dilute –> less sympathectomy.
- Esp for heavily beta-blocked pts w/ preE/gHTN, the baroreceptor reflex of ↑ HR may be blocked leading to more profound HOTN after sympathectomy (*↓ placental perfusion)
- *esp preE/HELLP as these pts are intravascularly dry and have exaggerated HOTN responses to sympathectomy
- ALSO for pts with HTN needing a surgical-level epidural bolus for a C/S for decels**– May be better to dose most of it in OR w/ monitors on. Want to keep moms BP at baseline to maintain placental perfusion, which in an already distressed fetus can cause further acidemia/hypoxemia. If you start dosing in labor room/hallway you have no FHR or maternal BP/HR monitor in place to see effects of dose. These PreE/HTN pts are also intravascularly dry and a sympathectomy can cause an exaggerated HOTN from a relative hypovolemia.
- 5cc or so in the room should be fine, but don’t give the full 20cc dose off of monitors.
- Additionally, these pts with working epidurals don’t aways need the full 20cc dose for adequate coverage, so it would needlessly add to a higher-than-necessary-level block and greater sympathectomy.
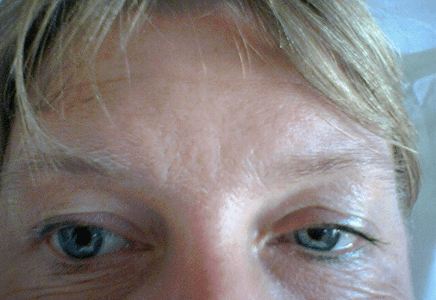
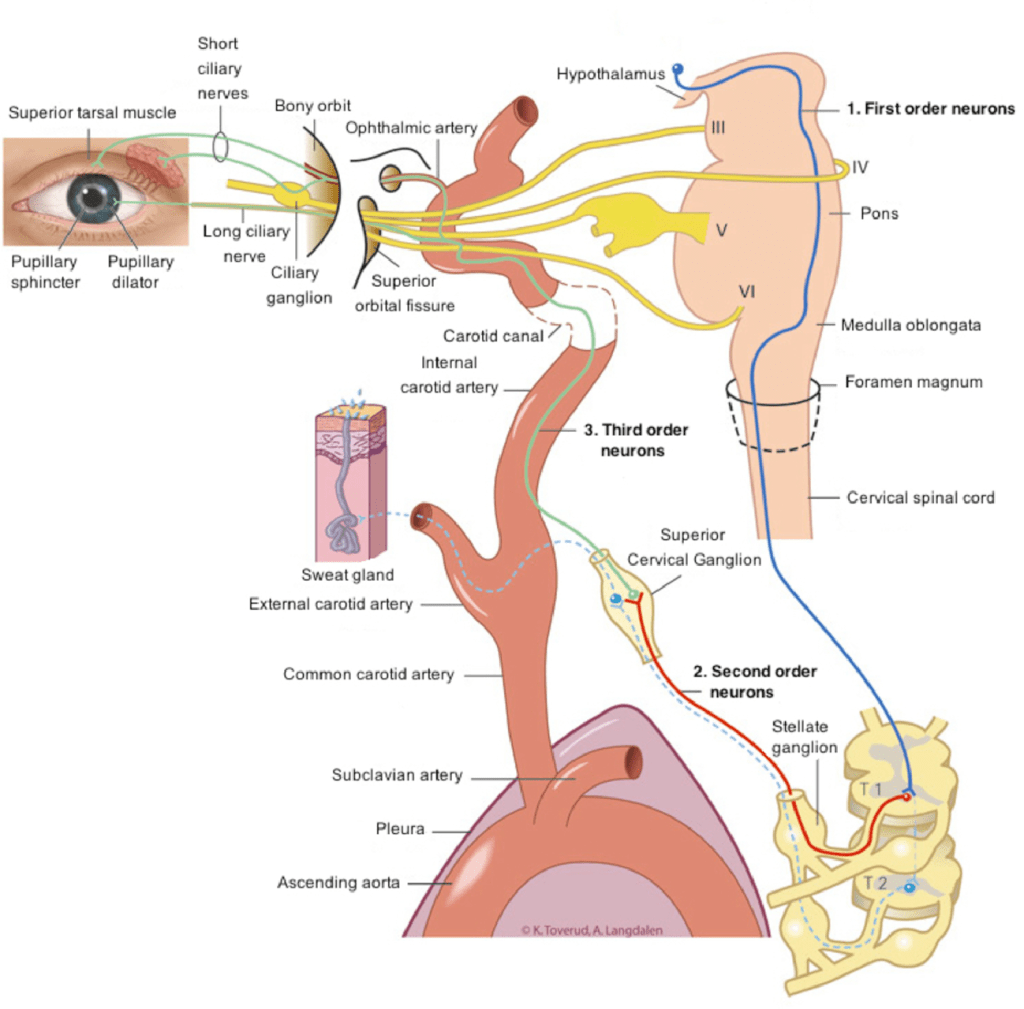
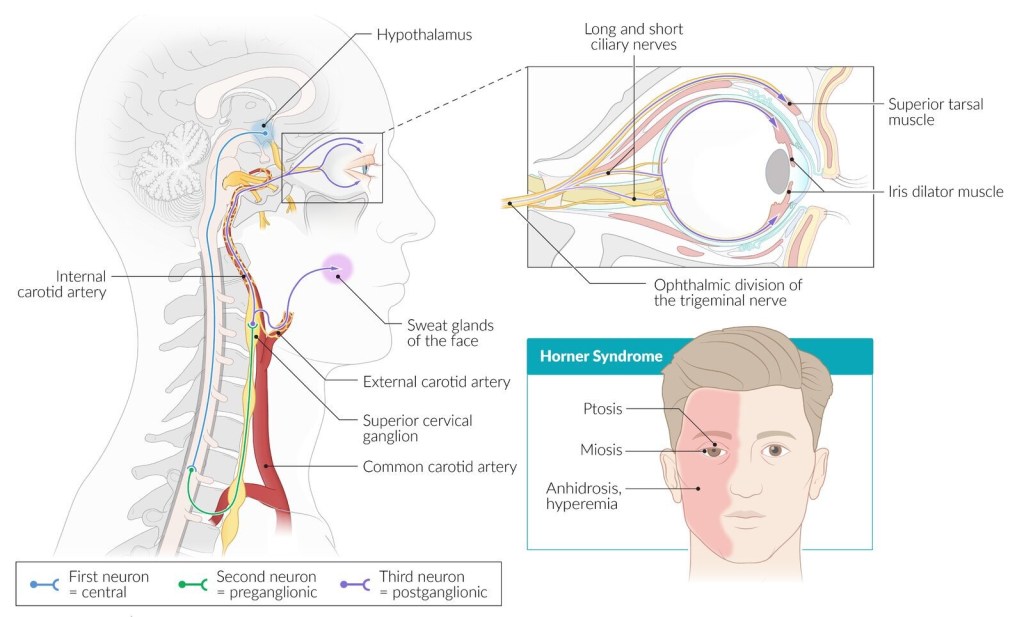
HORNER SYNDROME
aka ” oculosympathetic palsy”
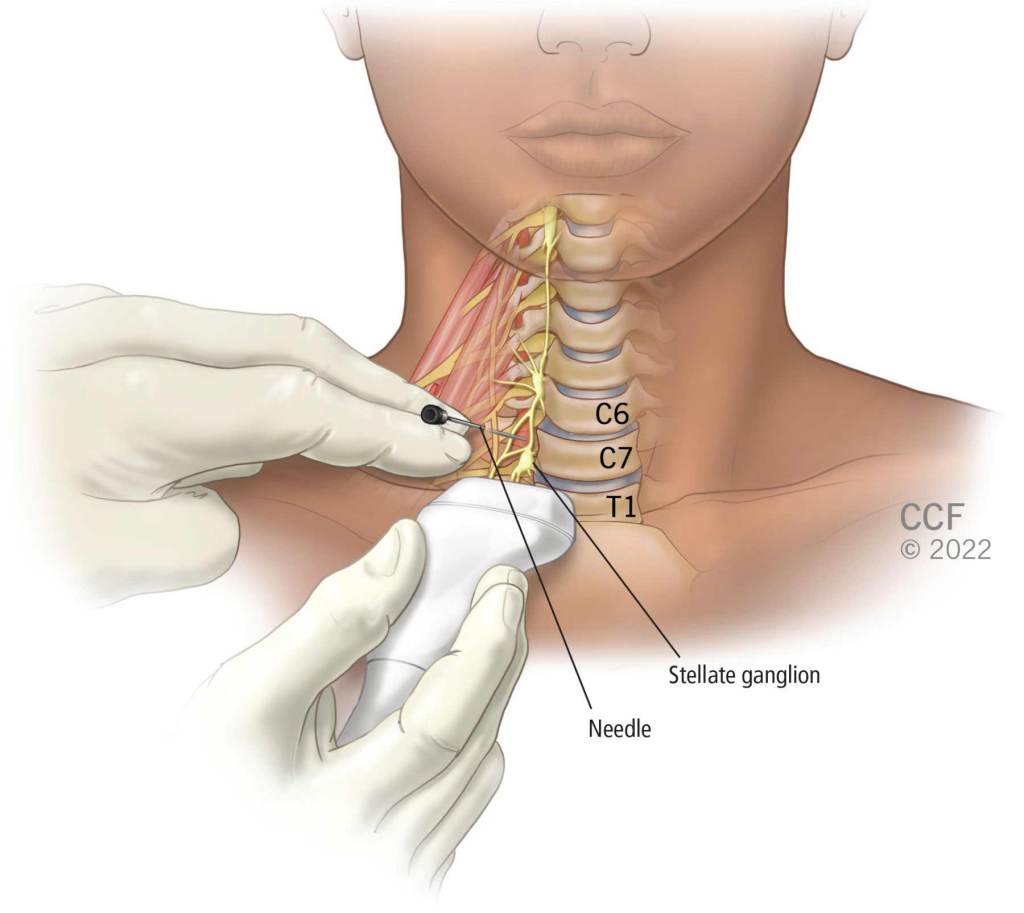
- Possible for pts to develop Horner syndrome from an atypically high cephalad spread of LA up through epidural fat tissue, usually after bolus dose(s) (higher pressure). Epidural space runs from foramen magnum to sacral hiatus, and LA can reach cervical ganglion (C8-T1 nerve roots for Horner’s) (Second-order neuron etiology)
- Horners syndrome is a sympathetic block of the stellate ganglion:
- Normal S/S triad:
- 1) Ipsilateral ptosis of upper lid – caused by denervation of superior tarsal (Muller’s) muscle (SNS innervation: Alpha1D, Alpha2C, & beta2 )
- Slight elevation of the lower lid, sometimes called upside-down ptosis
- Sunken appearance of the affected eye (enophthalmos)
- May see some redness in affected eye from vasodilation (conjunctival hyperemia/conjunctival injection)
- 2) Ipsilateral Miosis (pupillary constriction)
- still reactive to light, may be slightly delayed) (anisocoria is a difference in pupil size) (parasympathetic)
- caused by uninhibited PNS = constriction (miosis – circular muscle = muscarinic receptor- ACh, whereas dilation = radial muscle = alpha1 adrenergic (norepi) SNS receptor).
- Pupillary light reflex & accommodation remains normal – (CN2&3 – reflex not dependent on SNS/adrenergic receptors)
- still reactive to light, may be slightly delayed) (anisocoria is a difference in pupil size) (parasympathetic)
- 3) Ipsilateral Anhydrosis
- face may look red and flushed (SNS controls sweat glands)
- 1) Ipsilateral ptosis of upper lid – caused by denervation of superior tarsal (Muller’s) muscle (SNS innervation: Alpha1D, Alpha2C, & beta2 )
- ASSESS:
- Neuro exam: pupil reactivity (rules out CN 2&3 intracranial pathology), no facial droop should be present aside from ONLY ptosis. No facial nerve (CN7) involvement – assess smile – should be intact.
- Visual deficits are abnormal – pts can see just fine with ptosis (usually don’t realize it’s there) and pupillary constriction doesn’t affect eyesight.
- Check BP – high LA spread = potentially high sympathectomy
- Sensory level block bilaterally – high block? limb involvement? Is she comfortable though? Is epidural still working bilaterally? Not a subdural/not a patchy block? If it’s working, (depends on the pt and difficulty of placement – but might be better to just leave it in place if it still works)
- MANAGEMENT:
- Chill on the boluses.
- Sit her more upright – gravity
- I’d pull the catheter back a little, if possible. Catheter might be in a position near some weird path/channel of least resistance for fluid to move cephalad through the epidural fat tissue, new catheter position via pulling back may cause different spread/put less pressure on that atypical fluid pathway.
- Not necessarily a reason to replace the catheter if it’s otherwise working well – this will resolve when epidural infusion D/Ced.
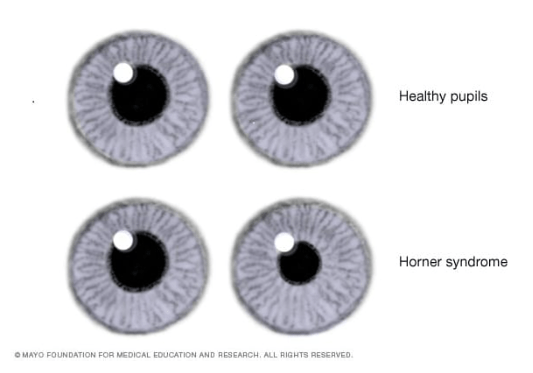


This article explains the pathophysiology & different causes of Horner syndrome – differentiating intracranial pathology vs second/third order neuron causes: From an OB epidural – this is not an intracranial (1st order neuron) pathology. This is a 2nd order neuron pathway (spinal nerve root C7/8-T1) affected by LA, inhibiting pre-ganglionic pathways through sympathetic chain ganglion, and further through superior cervical ganglion, which inhibits post-ganglionic neurons at their effector sites: (short ciliary nerves: SNS ACh-mediated sweat glands of face, & innervating Muller’s (superior tarsal) muscle of eyelid), and long ciliary nerves innervating pupillary dilator (radial SNS-innervated muscle.)
Horner Syndrome – StatPearls – NCBI Bookshelf
What IS NOT Horner’s Syndrome? r/o TIA/stroke
- Impaired vision (pt usually doesn’t notice the ptosis – and pupil constriction does not impair vision)
- Dizziness (eh…a higher sympathectomy from a high block may cause some wooziness – check BP)
- Slurred speech
- Severe, sudden headache or neck pain
- Difficulty walking / Muscle weakness or lack of muscle control (cannot assess with epidural)
- but some ipsilateral upper limb weakness would not be unusual in the setting of Horner syndrome since the LA has traveled high enough to reach high thoracic & cervical ganglion if it has reach stellate ganglion.
BACK LABOR / BACK PAIN
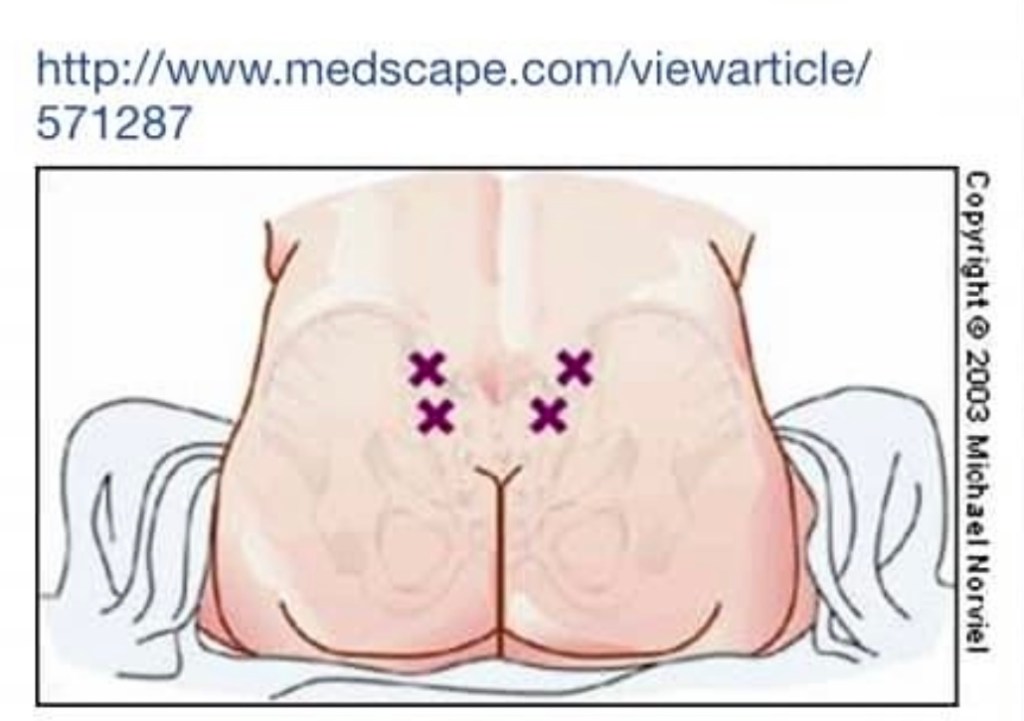
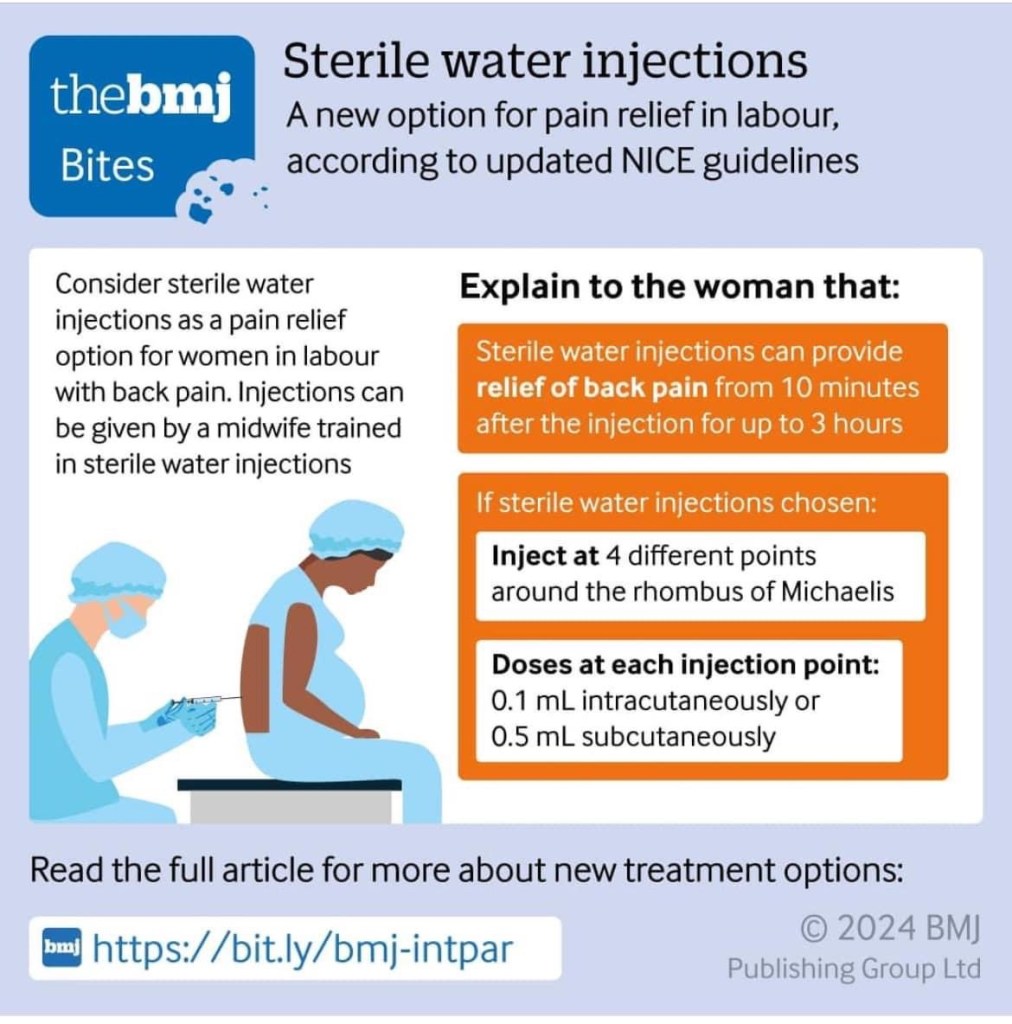
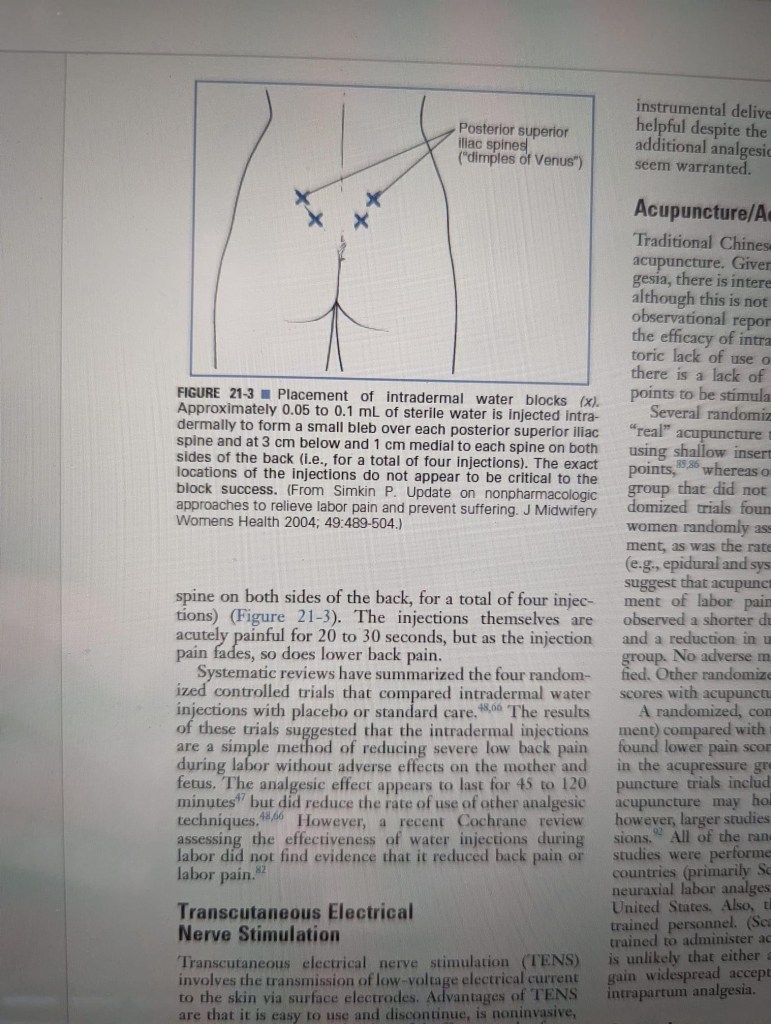
Can inject INTRADERMAL STERILE WATER at specific points with insulin or TB syringe:
DOSE AT EACH INJECTION POINT: 0.1 mL interdermal, 0.5 mL subQ
(I’ve never tried this – I just learned about this technique, but it can’t hurt, especially as an option for women who don’t want an epidural or don’t qualify for one..)