CONTENTS:
- Podcasts & Resources for high-risk OB conditions.
- Lots of links to experts explaining really important topics and simplifying complex concepts. Links are all included, I’ve added some bullets, but the lectures/podcasts are GOLD. Worth every second of listening/watching.
Notes:
- High Risk OB Podcasts: easy to listen to, and very informative.
- The common high-risk placental disorders:
- Vasa Previa
- Placenta Previa
- Placenta Accreta
- Placental abruption
- These all have different levels of terror and apprehension when it comes to neuraxial, coagulopathies, and hemorrhage risk.
AWESOME OB PODCASTS and RESOURCES ON ALL OF THE THINGS:
Great for high-risk topics, cardiac OB concepts as well as coags, general OB anesthesia concepts, physiology, etc etc. Way easier than reading…
Creogs over Coffee:
- 2 lovely OB chief residents discussing all things OB/high-risk, over coffee.
Critical Care Obstetrics Podcast:
- This MFM is great – engaging & easy to listen to – makes complex topics simple. 10/10.
The Critical Care Obstetrics Podcast
Cardionerds:
- It’s a cardiology podcast but they have a cardio-obstetric series with 10 or so OB episodes – filled with content, and awesome expert speakers on every episode.
Cardionerds: A Cardiology Podcast
ACCRAC: (Anesthesia Critical Care Review And Commentary) has some good OB episodes too
- Episode# 62, 63, 46, 162, 159, 160, and a few more..
Episode 62: Problems during pregnancy with Jacqueline Galvan part 1
HIGH – RISK PLACENTAL DISORDERS
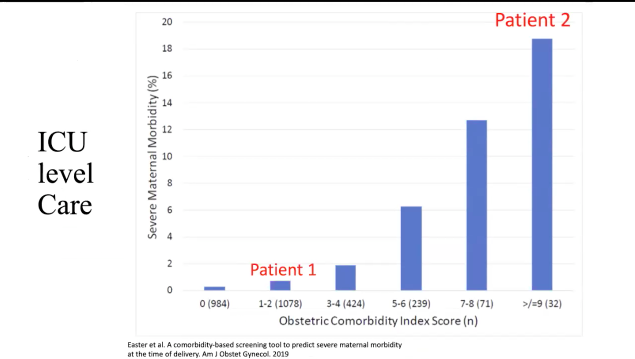
Big players in maternal morbidity:
- Index score for comorbidities
- Bar graph showing totals and morbidity%
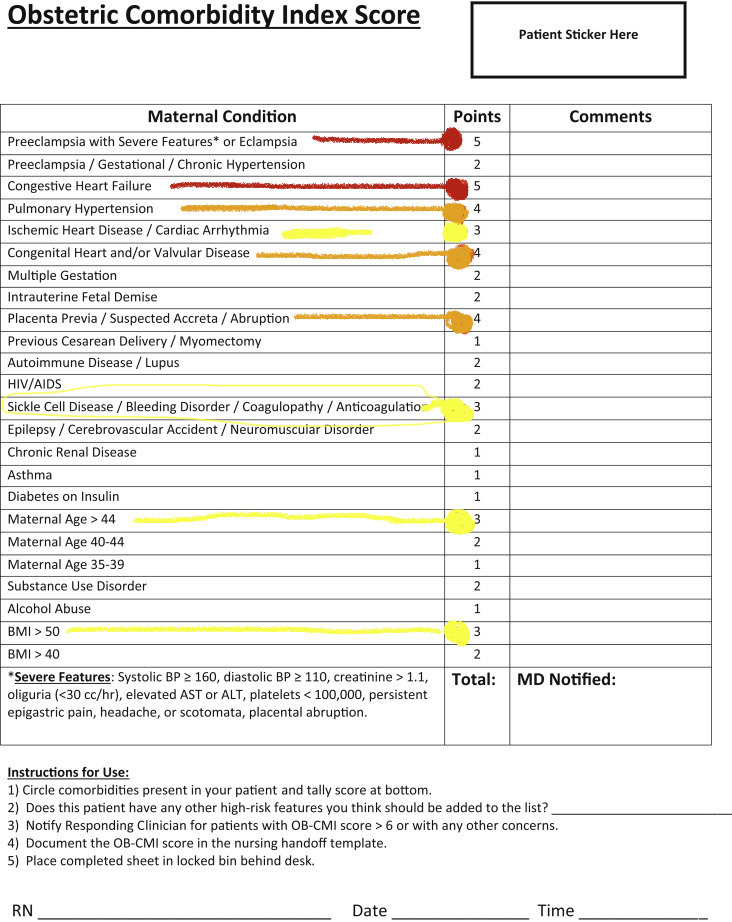
How these comorbidities contribute to requiring ICU-level care:

High Risk Obstetrics Guides & Resources
Anesthesia in High-Risk Obstetrics
Anesthesia for the high-risk parturient – PubMed
HIGH RISK PLACENTAL ABNORMALITIES
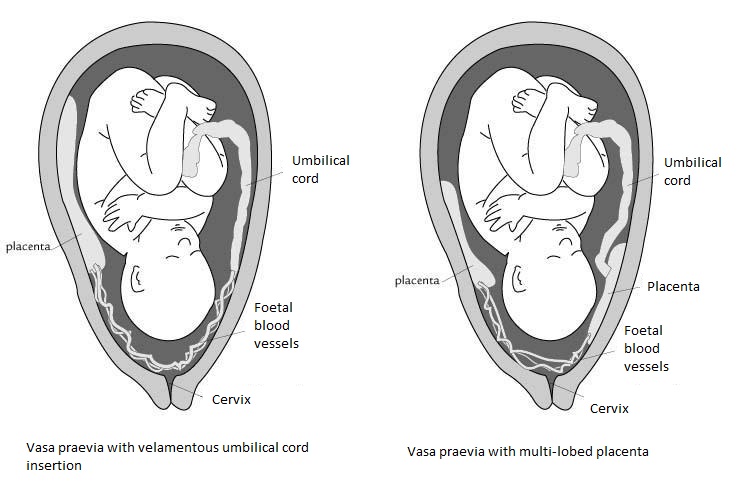
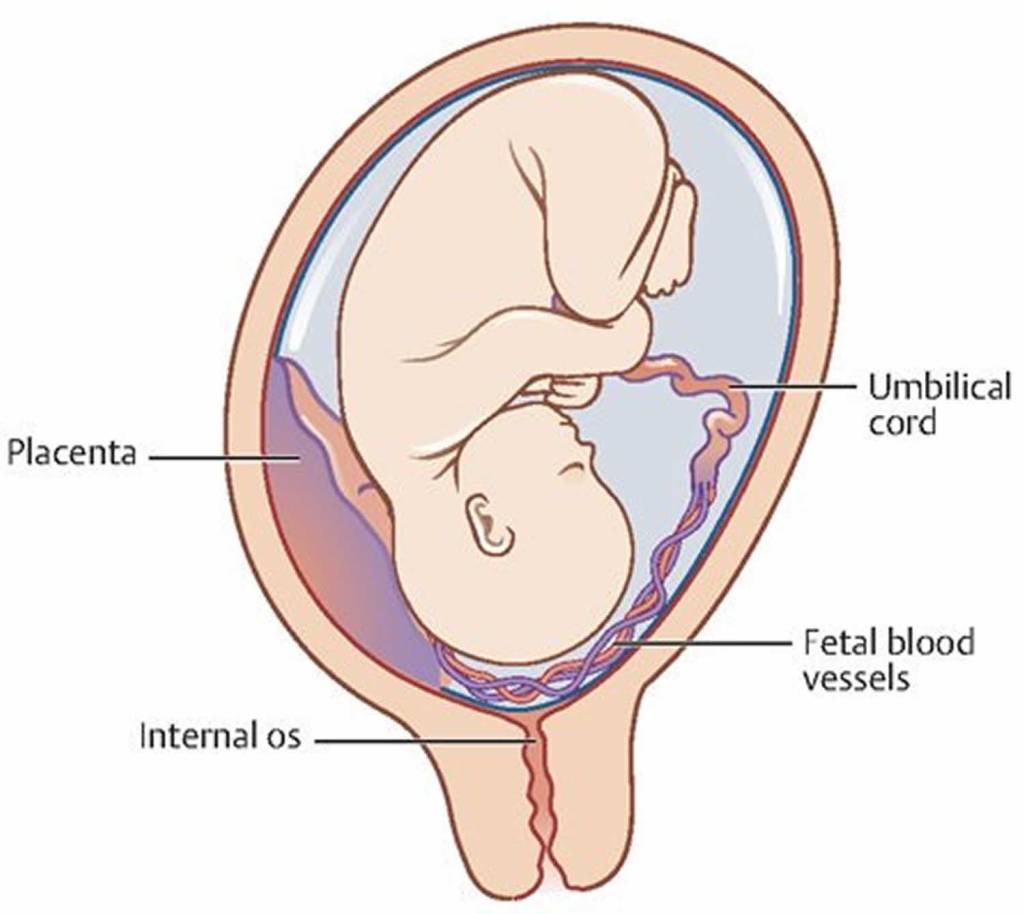
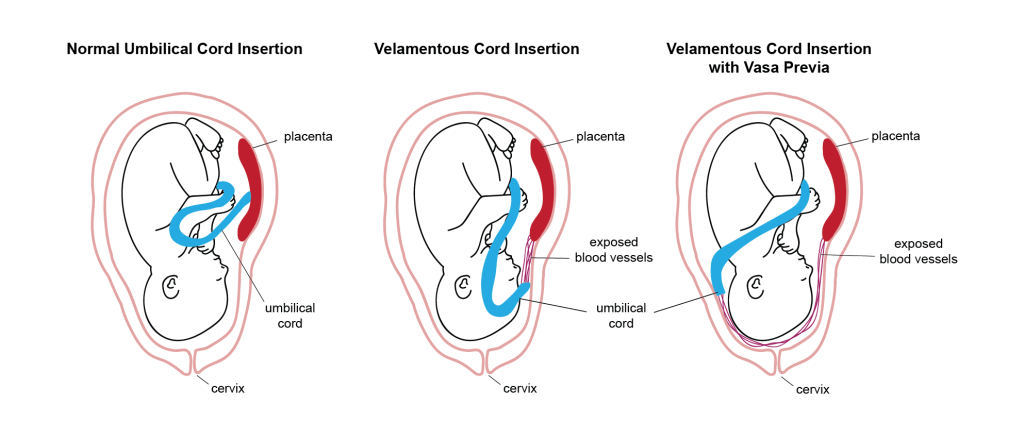
VASA PREVIA
- Tiny stringy vessels abnormally connecting umbilical cord to placenta (aka velamentous cord insertion) will easily be compressed and can rupture, leading to fetal exsanguination and death .. at the very least cut off fetal blood flow (O2) with contractions/fetal descent.
- Planned C/S
- Cannot allow labor or ROM in these pts
- Fetus at higher risk of fatal blood loss than mom.
SMFM Society for Maternal Fetal Medicine update on Vasa Previa:
Publications & Guidelines | SMFM.org – The Society for Maternal-Fetal Medicine
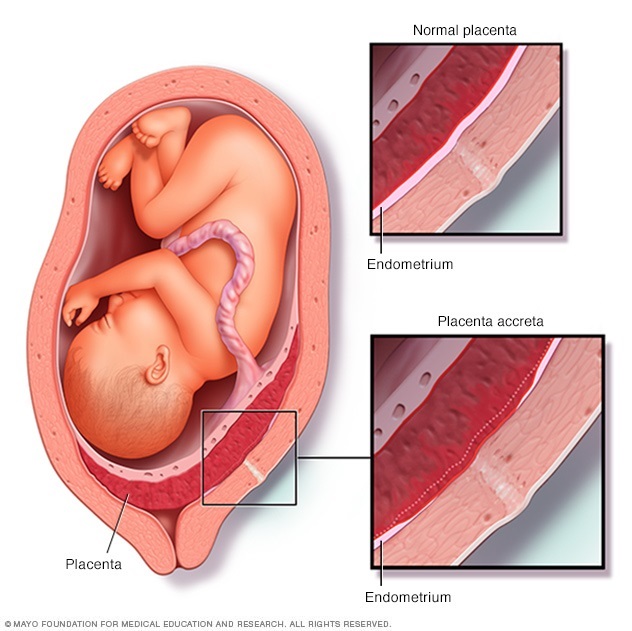
PLACENTA PREVIA
Abnormality of Placental POSITION/LOCATION
- Previa = Problem with placental location: attached low on uterus and covers all, or part of, the cervical os.
- Placenta attaches at Lower Uterine Segment in Previa
- If also Hx prior c/s = high risk of Accreta as placenta sits on top of uterine scar.
- Biggest anesthesia concern: HEMORRHAGE
PAINLESS BRIGHT RED bleeding is hallmark sign
- Previa bleeding occurs 2/2 the lower uterine segment stretching and thinning out as the uterine size increases with a growing fetus. In previa, the placenta is attached to the lower uterine segment (LUS) instead of higher up in the uterus. The lower segment normally forms later in pregnancy in the 3rd TM as it stretches to accommodate a rapidly growing fetus. Normally, this LUS stretching does not cause bleeding, as the placenta is normally attached higher up and is unaffected by LUS. However, in previa, as the placenta its right on top of the LUS, the stretching can cause placental detachment from the decidua basalis, which can tear the placental blood vessels connected to the LUS. This will often cause painless bleeding, but can also cause full detachment/abruption and massive hemorrhage.

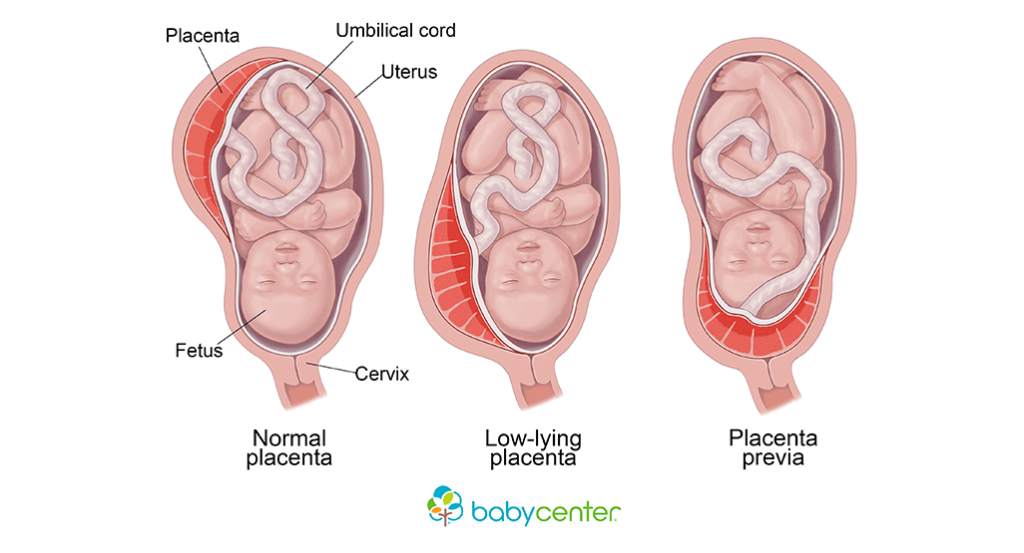
PREVIA pts CANNOT go into labor
- Placenta will bleed/rupture w/ contractions/pressure with labor and fetal descent
- Placenta has lower quality attachment at lower uterine segment- can detach and abrupt more easily
- Contractions, dilation, and effacement can cause placental detachment.
- Cannot allow labor or ROM in these pts
- Planned C/S
Placenta Previa = High risk bleeding:
- Attachment on the Lower uterine segment not only can cause placental detachment, but the thin area of LUS muscle does not contract well.
- Strong muscle contraction is required to clamp down uterine vasculature (maternal spiral/uteroplacental arteries) feeding the placenta and prevent bleeding. When placenta forms over the LUS, the highly vascularized area beneath the placenta also forms on the LUS. Thin, weak muscle = crappy contraction = more bleeding after delivery.
PREVIA ANESTHESIA CONSIDERATIONS
- 2 large bore IVs
- blood T&C, 4 RBC, 4 FFP ON HOLD. Fluid warmer w/ blood tubing set up.
- TXA in rm as well as uterotonics: “hemorrhage kit” (RN provides)
- If accreta also present, accretas will often be a c-hysterectomy. A working epidural should be in place for neuraxial.
- With a severe hemorrhage – have a low threshold to convert to GA while they still have a blood pressure, regardless of quality of neuraxial – severe HOTN won’t tolerate induction —> can use etomidate.
- Give versed with low sevo and 50/50 N20
- 1) sevo relaxes the uterus – minimize %
- 2) neuraxial anesthesia still on board – so surgical stimulus may not be as great (anesthesia to tolerate ETT)
- Give versed with low sevo and 50/50 N20
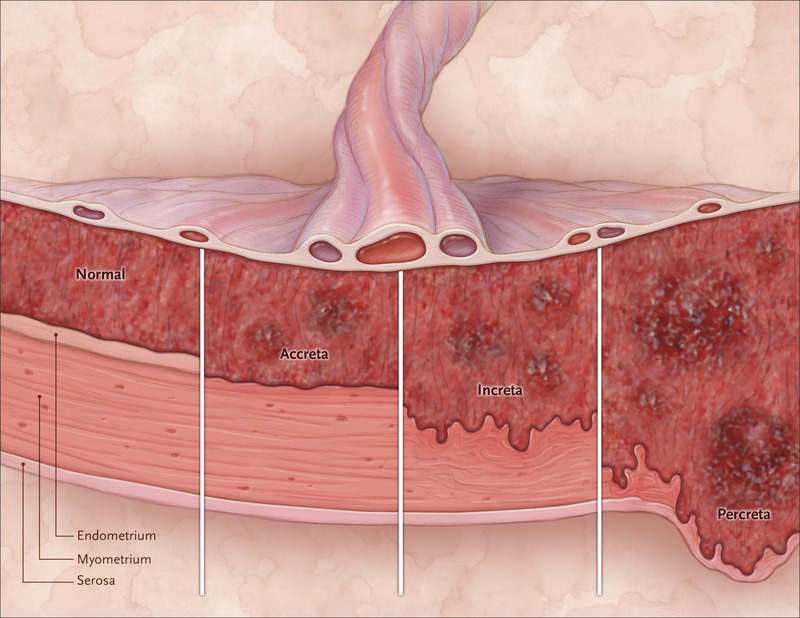
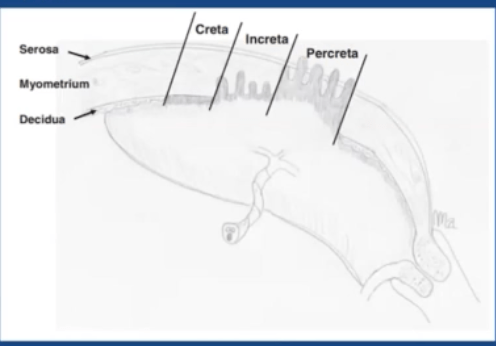
PLACENTA ACCRETA SPECTRUM
Abnormality of placental IMPLANTATION
PAS = Placenta Accreta Spectrum
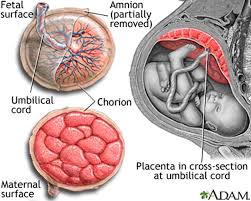
- In normal pregnancy, the endometrial layer becomes “decidualized” when the placenta attaches to it. The decidua becomes an interface for maternoplacental blood flow (O2 & nutrient exchange bc the blood never actually mixes. The Decidual layer also allows clean detachment of placenta after delivery.
- In accreta, there’s no decidual layer between the placenta and myometrium to provide a clean break. The placenta just attaches straight to muscle and creates a *Hemorrhage City* of abnormal vascular remodeling and lacunae, or “placental lakes” leading to massive hemorrhage when placenta is removed/torn out of the muscle where these vascular lakes have formed.
- The cause of accreta is debated – old thoughts were it was an over-aggressive placental trophoblastic invasion through the decidua to the myometrium. But new thoughts are it may more of a problem w the decidua itself where it doesn’t form properly and the placenta attaches to the next logical place – the myometrium.
- Placenta previa is a huge risk factor for accreta (discussed in detail below)
Placenta accreta spectrum-a catastrophic situation in obstetrics
Ultrasound Detection
Best in 2nd TM: sensitivity 90% Specifity 96%.
- Placental LACUNAE/“Lakes” or “Turbulent/pooling lakes” (75-100% predictive value)
- LACK OF U/S FINDINGS DOES NOT PRECLUDE DIGNOSIS OF PAS!!!
- CLINICAL RISK FACTORS IMPORTANT TO KNOW.
- NO WAY TO 100% diagnose and detect accretas with imaging. (Ultrasound/MRI) We have surprise accretas. Estimated 50% are unknown.

One more time for the kids in the back:
THERE IS NO WAY TO 100% diagnose & detect accretas with imaging. (U/S & MRI) We have surprise accretas.
Estimated 50% are unknown.
MFM Article: HALF of Accreta patients were undiagnosed:
Morbidly Adherent Placenta Treatments and Outcomes
Anesthesia Accreta Considerations
- If known accreta – always c/s
- IF high risk for ACCRETA based on PSH of c/s and current previa: prepare for potential accreta discovery as placenta is extracted.
- Extremely high risk of bleeding in all accreta cases
- With multidisciplinary team: Anesthesia, ICU, OBGYN, MFM, UROLOGY/cysto
- Pre-op labs & checklists
- In case of emergent hemorrhage – determine pre-op who will place orders: MTP/OB hemorrhage, coags, CBC, TEG, etc. Can be RN or anesthesia.
- i-stat and intra-op lab testing supplies
- Cell saver?
- 2 lg bore PIV 14 or 16g, blood line and warmer, 4RBC & 4FFP IN OR.
- IF blood antibody+, blood needs to be READY IN ROOM (4 units) before going back to OR – this blood takes longer to prepare and theres no time to wait if she hemorrhages intra-op.
- Rapid infuser available.
- Vasopressors: neo, levo, epi
- A-line when appropriate.
- TLC available
- TEG/ROTEM capability – risk of DIC.
- Bleeding risk is usually AFTER DELIVERY, as placenta is being removed and pulled off of the uterine muscle it’s attached to. Abnormally high vascularity and tissue trauma trying to detach.
- Focal accreta is one small area – can possibly still extract placenta without massive hemorrhage, if very small.
- Often accretas are an indication for hysterectomy d/t risk of lethal hemorrhage.
- In this case of known accreta, placenta is often left in situ after cord clamping and hysterectomy is performed.
- DELIVERY usually 34-36 wks. = preterm. Pt may need Magnesium bolus for fetal neuro protection, and corticosteroids for fetal lungs: both increase risk of pulm edema (esp in setting of possible massive transfusion).
- Pre-term uterus less sensitive to oxytocin. Second-line Uterotonics may be needed. (methergine & hemabate)
- Magnesium can also contribute to uterine smooth muscle relaxation –> increased bleeding
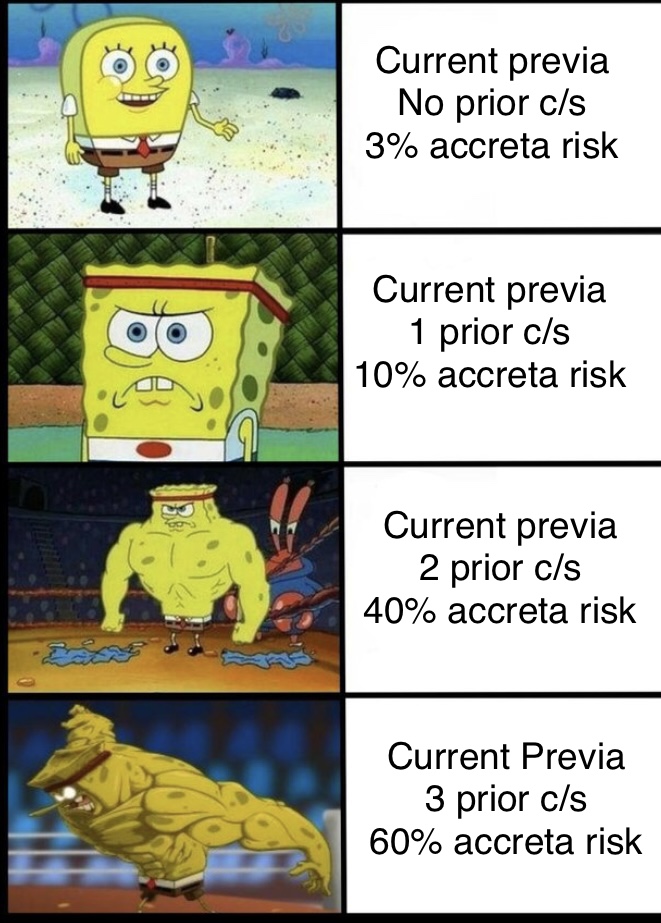
RISK FACTORS FOR ACCRETA
Since accretas, once again, ARE NOT 100% DETECTABLE, the risk factors are AS IMPORTANT for predicting accretas as diagnostic imaging. High risk factors = high risk, regardless of imaging.
- Placenta Previa is a primary risk factor
- Previous Uterine Surgery
- C/S:
- 1 prior c/s = 0.3%
- 5+ prior c/s = 6.74%
- myomectomy for fibroid, anywhere there could be a scar in the uterine muscle
- uterine ablation
- pelvic radiation
- C/S:
- IVF
- (biopsies taken of uterus/endometrium – can leave biopsy scars, also embryo can implant lower on LUS from trans-vaginal/cervical placement approach, vs implanting higher up after dropping out of fallopian tube in normal pregnancy, (LUS implantation has higher risk of previa & accreta)
- Also the chicken or the egg debate: does IVF instrumentation create problems/scarring in the decidua? Or is IVF needed bc there’s already an existing genetic(?) problem with the decidua in the first place which could lead to PAS?
- Elevated AFP (unexplained MSAFP elevation assc w/ PAS)
- Asherman’s syndrome (abnormal buildup of intra-uterine adhesions)
- Multiparity
- Advanced Maternal Age.
- Theoretically any uterine instrumentation like a D&C and IUD removal could increase accreta risk, but data shows the big known players are uterine myometrium surgical scars.
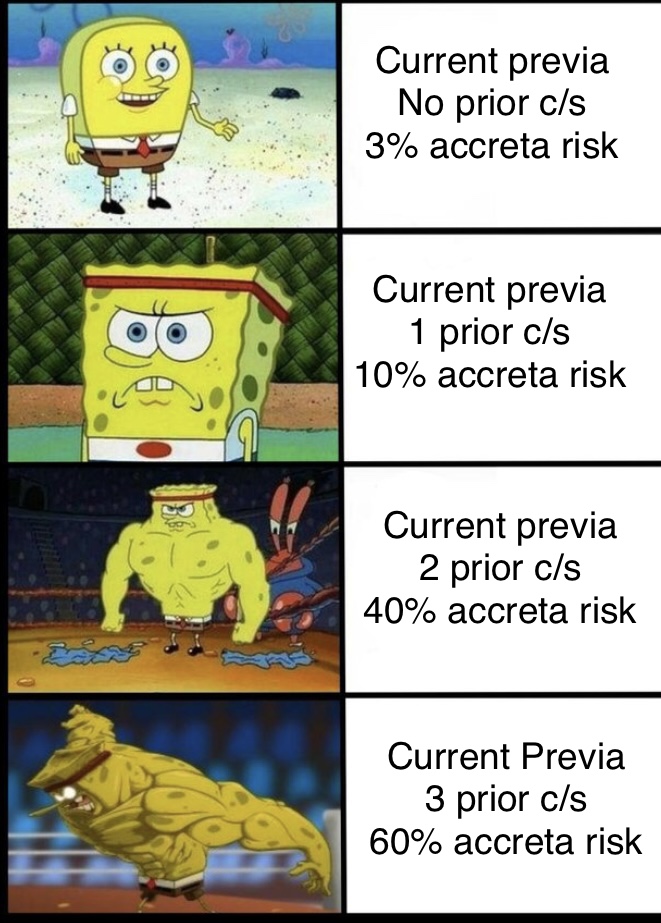
*Placenta Previa is a MAJOR risk factor for accreta *
Know risk stratification despite “no dx of accreta on Ultrasound/MRI imaging” (large % undetectable)
Estimating Accreta Risk:
Remember “3, 10, 40, 60”
- Current previa with no prior c/s = 3% risk of accreta 😥
- Current Previa with 1 prior c/s = 10% risk of accreta 😰
- Current previa with 2 prior c/s = 40% risk of accreta 🥵
- Current previa with 3 prior c/s = 60% risk of accreta 🤯
- Current previa with 4 prior c/s = 67% risk of accreta 🤯
- Previa is a risk factor for accreta bc previa attaches LOW on the uterus at the lower uterine segment
- this lower uterine segment has a thinner endometrium/decidua and a thinner muscle that’s easier to attach to.
- (Lower uterine segments already suck for regular previas even without accreta bc the muscle contracts poorly and allows more bleeding when the placenta detaches — now add an accreta-attachment into the mix and you have a super bloody detachment on a super crappy, thin floppy muscle segment that can’t contract for shit.)
- This reason a current previa w hx c/s is such high risk for accreta is bc the lower uterine segment where previa attached is ALSO the site of scar tissue from previous c/s. So the placenta is attaching right over scar tissue where it’s more likely that the fibrous scar tissue disrupted the decidual layer (barrier) and made abnormal placental attachment more likely.
- So If mom has previa now, with a hx c/s, we know she has a placenta attached on her lower uterine segment (previa) right on top of previous scar tissue. More scar tissue (2/2/ more c/s hx) = higher risk of accreta as the placenta previa attaches right on top of it.

August 2022 SOAP fellow webinar: Placenta Accreta Spectrum (PAS)

LECTURE NOTES:
- Some institutions do accretas in main OR with gyn-onc take over after delivery, or PAS-specialized MFMs d entire case. Some do them in IR-hybrid ORs/C-arm OR for UAE capability.
- High degree of variability with EBL risk: some centers expect < 2L, most expect 2-5L, few expect > 5L. But this will affect pre-op planing
- Some do primarily GA, some regional with planned GA, some GA only if needed.
- 50/50 A-line, all have blood products, TLC in some sites. Probably determined by expected blood loss.
- Historically, institutional variability in naming dx: “placenta accreta, morbidly adherent placenta, abnormal placentation disorder, abnormally invasive placentation, adherent placentation”
- 2018 – this has been normalized to “Placenta Accreta Spectrum (PAS)” per ACOG, SMFM, GYN ONC, Etc.
- PAS includes: Accreta, Increta, Percreta, all now referred to as PAS.
- OLD VS NEW DIAGNOSIS:
- NEW HAS CHANGED TO A GRADING SYSTEM:
OLD grading scale:
NEW = GRADING SCALE. PAS includes all grades.

RATES ARE INCREASING:
- 1970s: 1 : 4,017
- 1980s: 1 : 2,510
- 1982-2002: 1 : 533
- 1998-2011: 1 : 272
AND CONTINUING TO INCREASE:
- Increasing SUBSTANTIALLY at rate of 2% per quarter
- Likely 2/2 rate of c/s (20%) for last 20 years + other factors
- Accreta: 1: 430
- Increta 1:500
- Percreta: 1:3200
RISK FACTORS AND PRE-OP PREP already listed above.
Note on surgical techniques:
- Conservative/expectant management: experimental, involves leaving placenta intact and in-situ, then closing & having pt wait on floor for placenta to involute 1-2 wks. Retrospective studies have shown 22-40% requiring subsequent hysterectomy after surgery.
- PRO:
- significantly less blood loss so far 1/2L v 3L, even if hysterectomy required, still significantly less EBL.
- CON:
- Higher risk of infection, sepsis, DVT,
- This can place pt at risk of requiring emergency hysterectomy during off-hour shifts when we are not well staffed or prepared with the best teams.
- 1-2 weeks of a nervous MFM, patient, anesthesia, etc, bc she may need emergent return to OR at any time.
ANESTHESIA TECHNIQUES:
- GA vs NEUARXIAL:
- Neuraxial may require conversion to GA. (d/t hemorrhage, HD instability, length and complicated surgery)
- TXA:
- Unclear if prophylactic dosing has any benefit.
- TEG:
- Helpful in guiding more specific goal-directed therapy.
- Less incidence of vol overload, TACO, TRALI
Great super quick two-part podcast on accreta – the guest docs on these episodes make it so much easier to understand — 1000% worth listening to, from national accreta experts:
Ep.1: Accreta gold.
Episode 113: Placenta Accreta Part I
Ep. 2: A few tangents about surgical techniques we have nothing to do with – but it comes back around and it has tons of valuable info – and gives a much better understanding of the surgical considerations and what they see when they get in there. Explains why blood loss is so high, as well as risks of different surgical management and preparation considerations. Very clutch. 100% worth listening.
Episode 114: Placenta Accreta Part II
15 minute episode – Speaker has a weird cadence BUT great explanation of WHY the bleeding is so severe. Explains the important differences in how the placenta implants in accreta and also how it’s so difficult to diagnose with 100% accuracy. Esp the first 10 minutes are worth listening to.
PLACENTAL ABRUPTION
There are varying degrees of abruption.. but usually EMERGENT C/S bc FHR tracing is shite.
Risk of: HEMORRHAGE, FETAL DEMISE, DIC
HIGH D.I.C RISK. THIS IS ALMOST ALWAYS EMERGENT. USUALLY GA if no epidural is in place.
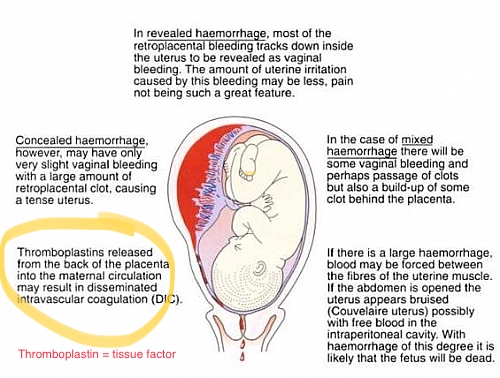
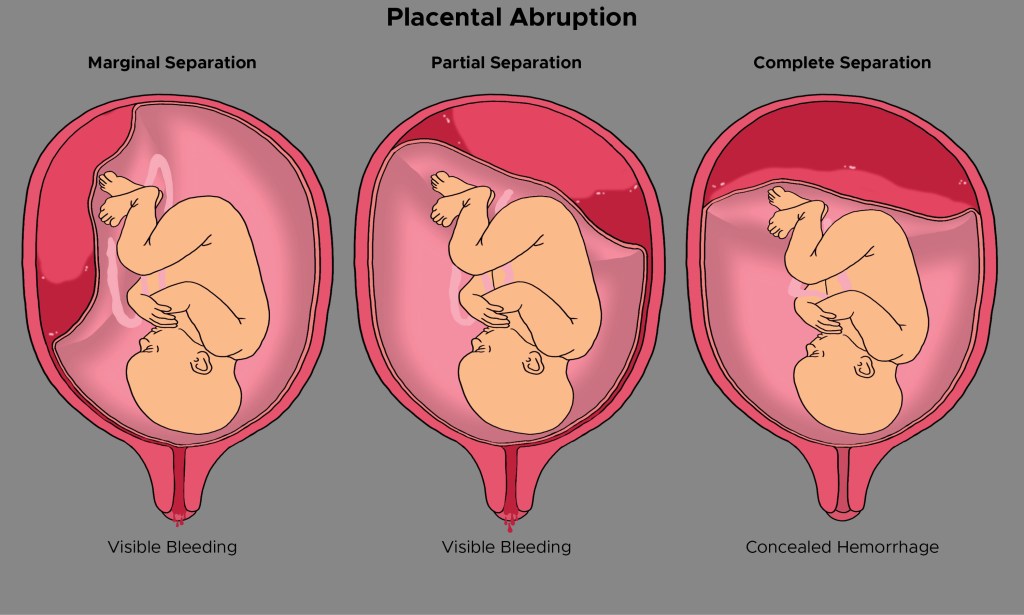
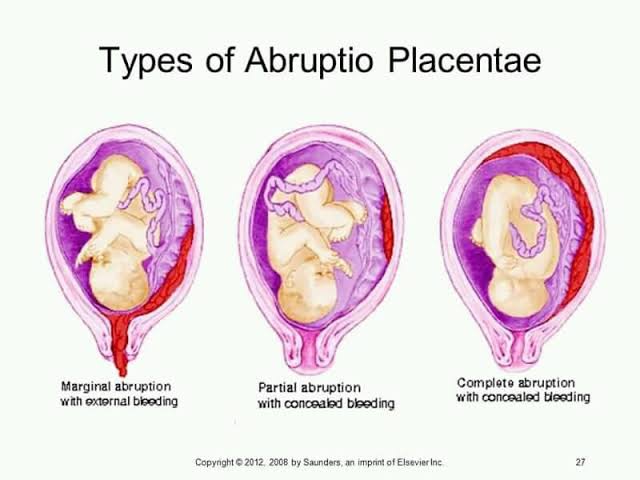
- Abruption is when the placenta detaches from the uterine wall. This detachment impairs fetal blood/O2 delivery, and mom can lose a ton of blood as she hemorrhages into this retroplacental space. Hemorrhage can be visible or concealed.
- Painful DARK RED vaginal bleeding is cardinal sign. Mom may be hemodynamically unstable, and usually FHR strip will look awful bc baby has impaired O2 delivery = EMERGENT C/S
- CONCEALED abruption = no visible bleeding as concealed hemorrhage and retroplacental clot continues forming behind placenta. Pt will c/o pain. Can be mistaken for contractions but pain continues after cxn subsides. OBGYNs can also tell the difference based on FHR and other s/s.
The high risk of DIC makes placing new neuraxial anesthesia extremely high risk.
- Once diagnosis/suspicion of abruption, pt needs NEW LABS: COAGS & CBC before neuraxial placed. Normally there isn’t time for this before we have to go back for c/s under GA.
- Although the the hallmark is painful vaginal bleeding – abruption can be completely concealed with no visible vaginal bleeding – and depending on the size and characteristics of the abruption – pain can vary. So as soon as the OBGYN diagnoses/suspects abruption based on other parameters/FHR strips/clinical indicators —> The plan changes and new labs are needed to see where we are along this potential DIC pathway.
(will repeat this and cover in COAGS: but the DIC risk in accreta comes from TONS of tissue factor(TF aka thromboplastin) accumulating in the giant retroplacental clot/bleed forming as the placenta pulls away abnormally from the uterine wall.. This impairs the maternoplaental interface (where blood NEVER mixes) and can create tiny tears in tissue and vasculature from which some of this accreta blood clot(loaded with TF) can mix with mom’s blood. If the TF enters maternal circulation through a breech in the maternoplacental interface – TISSUE FACTOR is now floating freely & SYSTEMICALLY through mom’s bloodstream —> MASSIVE coagulation STORM *EVERYWHERE.*)
– Whereas placenta previa and Accreta can cause high blood loss —> DIC (bc of course high blood loss means you’ll quickly consume a ton of clotting factors and can possibly go into DIC after you’ve consumed everything.)
Accreta also has this different TF mechanism by which is causes DIC – so its not from just blood loss, its from TF-loaded blood in the retroplacental clot sneakily entering maternal bloodstream where it doesn’t belong and isn’t supposed to go, and wreacking havoc.
Distinguishing 4 Mechanisms of DIC:
DIC from OB hemorrhage = consumption from site of bleed (localized to uterus, bleeding from uterus, clotting cascade activated at uterus, coag factors are consumed at uterus trying to control bleeding.),
DIC from inflammation/infection: systemic endothelial inflammation causes microvascular injury, which activates and consumes PLT/coags (preE, HELLP, IUFD—>Sepsis)
DIC from liver failure: all clotting factors are proteins made in the liver. Liver dysfunction/damage = clotting factor synthesis reduction.
DIC from abruption= placental/decidual/fetal tissue factor goes systemic = cascade activation EVERYWHERE not just uterus. = TF activating coagulation cascade with reckless abandon ALL OVER her body as it circulated freely through her bloodstream.
– Although DIC is DIC, and all ends at the same place, understanding the different ways it can develop will help you understand why the timing of neuraxial is so important. For other conditions presenting DIC risks 2/2 massive hemorrhage – a single-shot-spinal neuraxial technique may be fine if the bleeding risk only comes AFTER c/s delivery – we can better predict it’s onset. With abruption, you have an active pre-partum tearing away of the placenta – which at any time can cause a mixing of maternal and placental blood, so there is no way to predict at what point in the tearing that this maternal blood/ TF mixing would happen.
– Which is why as soon as the dx is made – new coags have to be drawn to see where on the spectrum mom is at the current moment. If cogs are FINE (fibrinogen >400 at least, INR ok, PLT ok) single shot spinal may still be safe for this pt for C/S. Otherwise, we cannot wait for coags to result and just go straight to general. If mom has a TERRIBLE UNSAFE difficult airway- then we have to weigh pros/cons of waiting for coags to result and allowing possibility for spinal.
Normal fibrinogen for non-pregnant pt is 200-400 mg/dL. Normal fibrinogen in PREGNANCY > 300, up to 600 mg/dL. Fibrinogen increases SIGNIFICANTLY in pregnancy, so a “normal” 250 fibrinogen is LOW for pregnancy —> trending toward DIC
- Whereas placenta PREVIA and ACCRETA are usually hemorrhage risk AFTER DELIVERY – ABRUPTION is an emergency bleed BEFORE delivery.
- although previa can still abrupt and bleed, and accreta can bleed before delivery as well.
Anesthesia Considerations in Abruption
By the time ABRUPTION gets recognized – mom and baby have ALREADY LOST BLOOD.
The risk of DIC associated with Abruption comes from potent, concentrated Placental and Fetal Tissue Factor (thromboplastin) from the retroplacental clot forming between the abrupting placenta and uterus, entering materal circulation and causing rapid widespread coagulation cascade activation as it flows freely through maternal circulation.
TF is present on the surface of cells (macrophages, endothelial cells, & monocytes) and is exposed to local, nearby circulation after endothelial injury to initiate the clotting cascade for hemostasis, however it does not normally float freely through circulation. This TF free-for-all causes a widespread, totally inappropriate activation of clotting cascade through all maternal vasculature, rapidly consuming clotting factors
The risk of rapid development of DIC in these pts makes neurxial high-risk.
- If NO COAGS *SINCE* diagnosis – NO NEURAXIAL. GA for C/S in stat situation where we cannot wait for coags. (There may be maternal or fetal instability necessitating urgent/stat C/S)
- If pt HAS COAGS *SINCE* diagnosis of abruption – and fibrinogen, coags, PLTs fine, then spinal is probably OK, and plan to convert to GA if severe instability/long case duration etc.
- Etomidate may be better for induction of GA – hypovolemia from blood loss can be masked by catecholamines in compensated shock.
- If epidural already in place from before abruption dx, dose incrementally. Hypovolemia will not tolerate rapid sympathectomy.
- HD instability should have low threshold for hanging BLOOD PRODUCTS.
- istat H/H, venous samples for coags.
- Important to consider abruption pt has ALREADY LOST BLOOD. We are always starting from behind.
- Expect instability from concealed hemorrhage.
- Have Blood, FFP, PLT in room, cryo
- 2 x lg bore PIV.
- If epidural catheter is in place from before abruption (labor) LEAVE in place until stable coags/teg/PLT. DO NOT REMOVE catheter. – can still use to bolus for c/s if catheter already in place.
DIC article – covered again in Coagulation Disorders of Pregnancy Page.
MISC:
Rare disorders: 👀👁🧠
Visual changes in pregnancy/postpartum:
PRES (posterior reversible encephalopathy syndrome)
- can be 2/2 preE/HTN)
vs
RCVS (Reversible cerebral vasoconstriction) (can be 2/2 valsalva/pushing)
- tx is CA++ channel blockers (nicardipine, nimodipine, clevidipine)