Mean PA Pressure (mPAP) >/= 20mmHg
Right Vent Systolic Pressure (RVSP) >/= 40mmHg
PHTN is a CONTRAINDICATION to pregnancy with no established safe cutoff of pressure.
WHY?
- HIGH maternal & fetal mortality rate ~20-50%!!!
- If Eisenmenger’s present – up to 50% mortality!!
- Either pregnancy happens against medical advice, or PHTN is new dx during pregnancy.
- Termination recommended.
- IUDs useful in preventing pregnancy, but vasovagal rxn from insertion may be poorly tolerated. Women with pHTN should have IUDs implanted in-hospital
- High risk of early delivery via cesarean 2/2 high maternal risk
- Most fatalities PERIPARTUM btwn 1 month pre-delivery & 1 month post-delivery
- Most dangerous time 24-48h postpartum 2/2 highest C.O.
- Can cause rapid decompensation.
- Maternal options in RV failure refractory to medical management include: ECMO and heart & lung transplant.
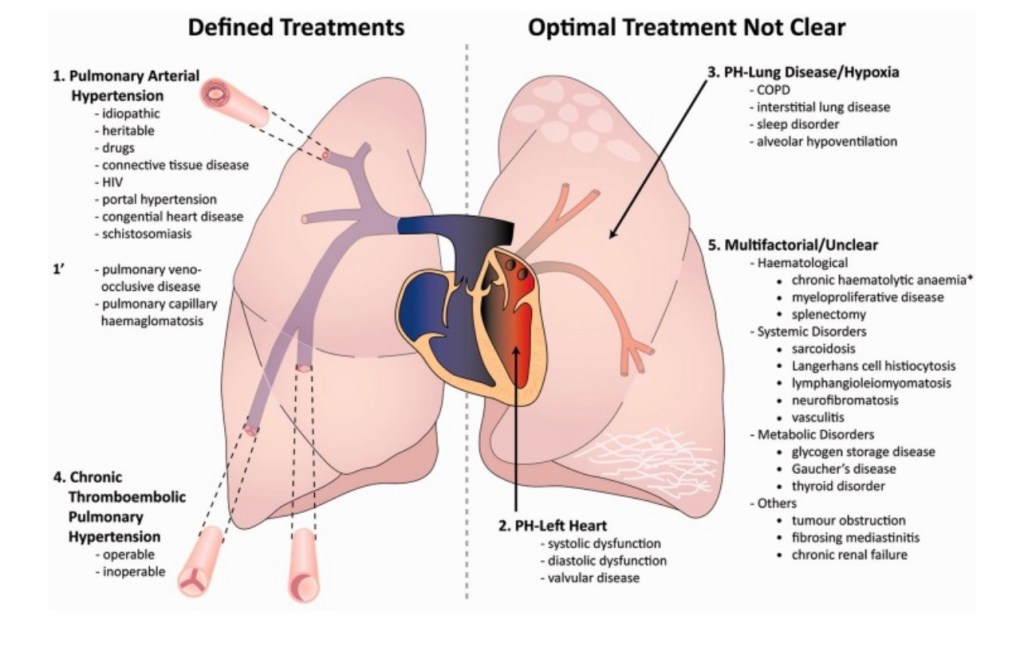
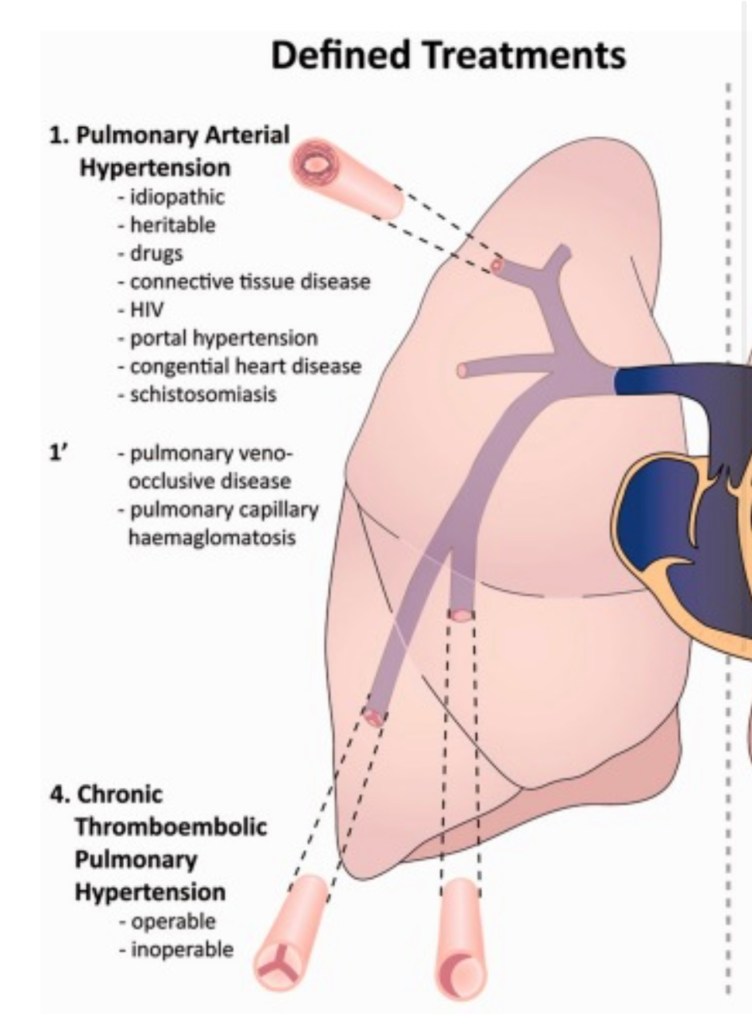
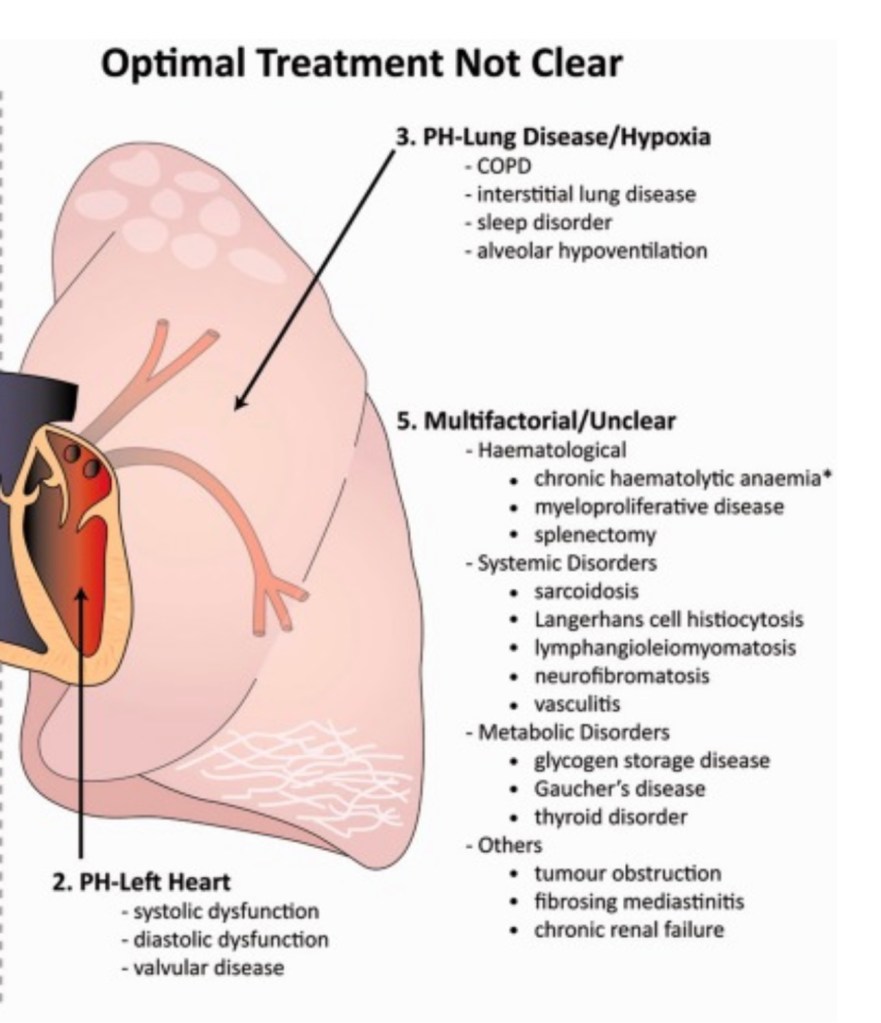
5 Types of PHTN
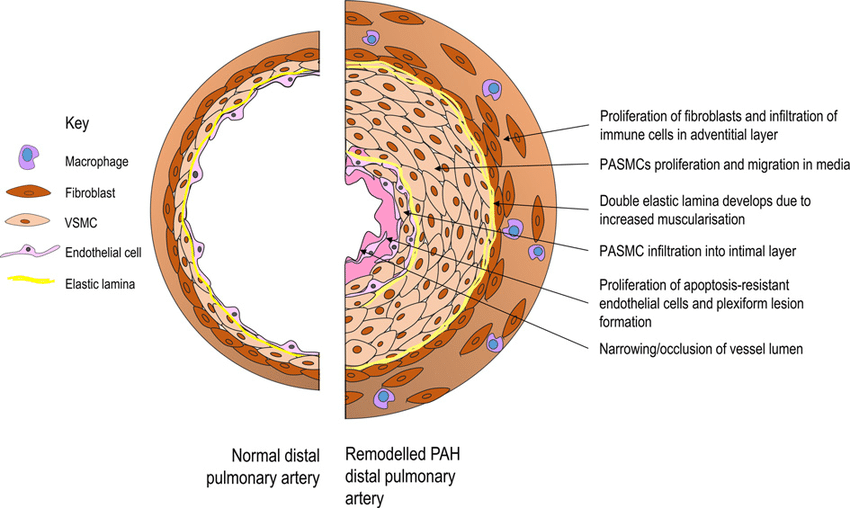
- Group 1: Pulmonary Arterial Hypertension (PAH)
- Idiopathic causes: thickening of pulm arteries.
- Heritable causes: genetic, CHD.
- Group 2: Left Heart Dysfunction
- Group 3: Lung Disease
- COPD, ILD, pulm fibrosis, OSA
- Group 4: Chronic Thromboembolic PHTN
- May require pulm thromboendarterectomy (factor 5 Leiden)
- If Hx of PE – should have ECHO prior to delivery
- May require pulm thromboendarterectomy (factor 5 Leiden)
- Group 5: unknown causes or a disease process
- sickle cell, sarcoidosis, chronic hemolytic anemia, splenecotmy, metabolic diseases, etc
pHTN IN PREGNANCY & ANESTHESIA CONSIDERATIONS FOR DELIVERY:
READ THESE 2 PAPERS!!:
Pulmonary hypertension in pregnancy-the Anesthesiologist’s perspective – ScienceDirect
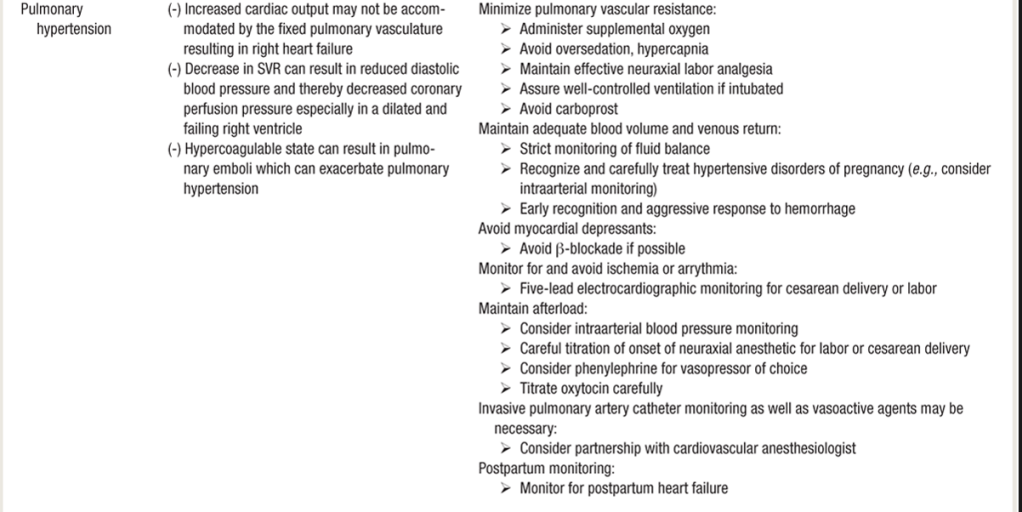
pHTN EXACERBATION IN PREGNANCY
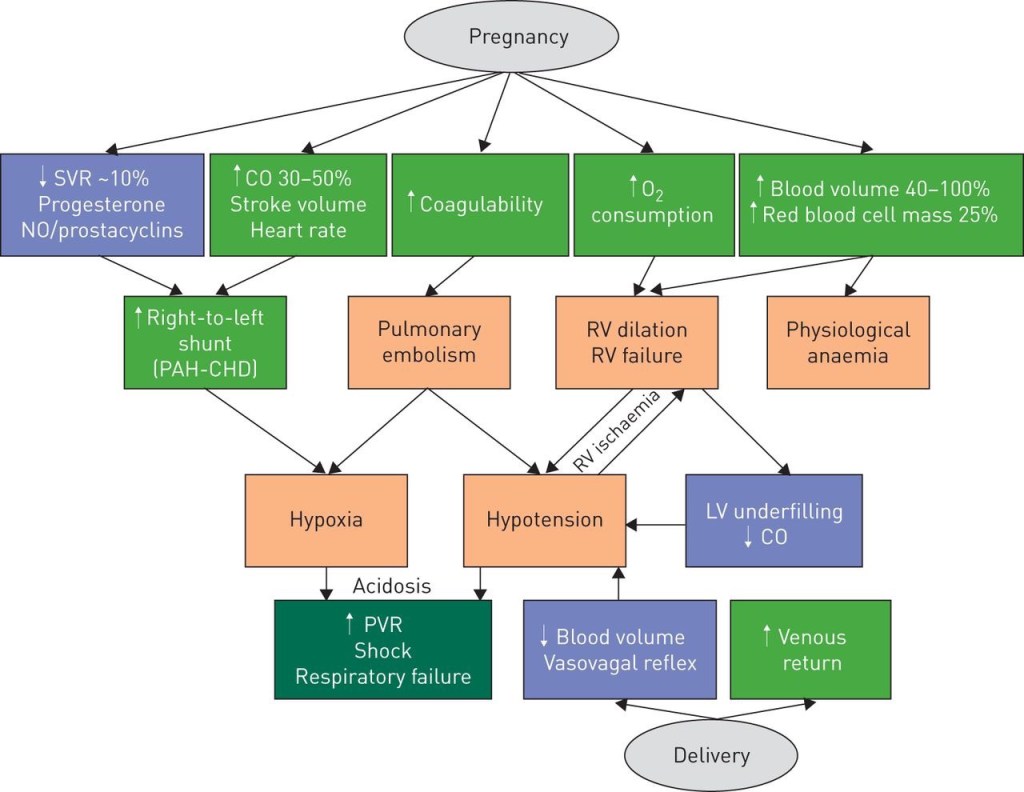
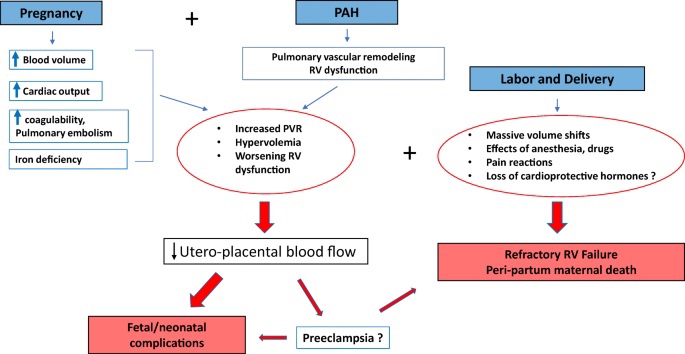
- In normal pregnancy:
- Increased plasma vol. & decreased SVR => increased C.O.
- Normally, in healthy women, PVR decreases to accomodate increased CO
- In PHTN, pulmonary vascular disease prevents PVR from falling —-> leads to increased PAP 2/2 increased CO.
- Ultimately, the necessary ^^ in CO demanded by pregnancy cannot be achieved —> leads to RV failure.
- As RV fails, volume & pressure increases 2/2 inability to overcome pulmonic valve afterload from high PVR in pHTN,
- Leftward shift of interventricular septum —> impairing diastolic filling of the LV and further compromising C.O.
- HYPERCOAGULABILITY of PHTN
- Diseased pulm vasculature pro-thrombotic
- hypercoagulability of pregnancy ^^ the risk of pulm emboli and pulm artery thrombosis. Also ^^venous pressure and stasis from failing RV —> DVT.
- Pts may be on ANTICOAGULANTS LMWH requiring neuraxial planning.
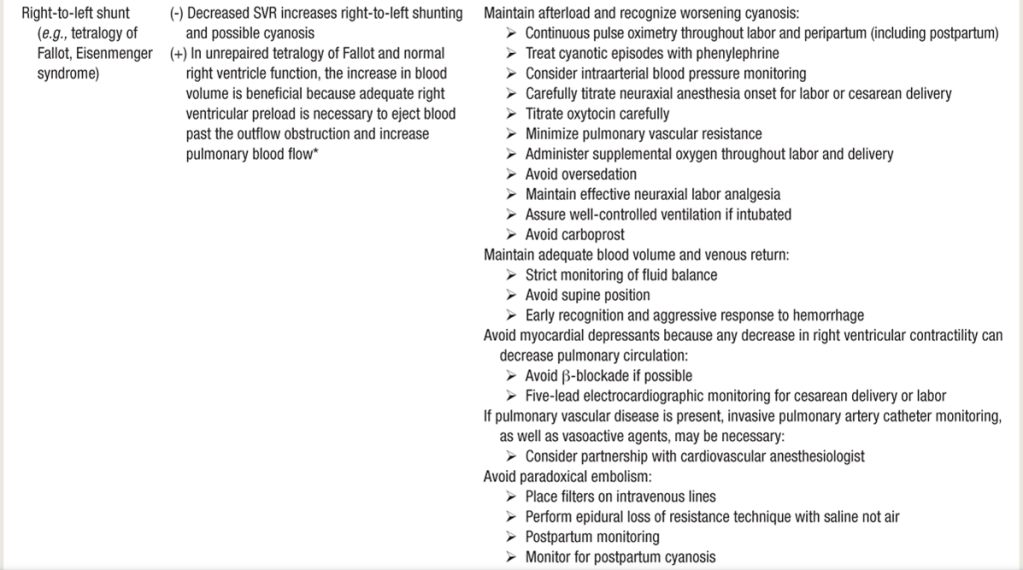
- Paradoxical emboli risk in women with PFO or Eisenmenger syndrome —> hypoxia —> ^^ pulm vasoconstriction and RV failure
- Hypoxia can also cause syncope & sudden death in these pts.
- IN LABOR:
- volume shifts 2/2 blood loss and autotransfusion (during labor cxns, or after delivery)
- Increased CO at full dilation
- vasovagal rxn to pain
- Also Valsalva of pushing reduces venous return and compresses ventricles
- Vaginal delivery not absolutely contraindicated, but not ideal – assc w/ vol changes during cxns —> problematic bc right heart can’t increase C.O. to accommodate vol changes. Also pushing can have adverse hemodynamic effects. And a stat c/s would be a shitshow lose/lose situation.
- If Stat C/S – won’t tolerate quick neuraxial HD swing of spinal or rapid epidural bolus, and GA isn’t ideal bc of 1) PAP increase in response to intubation, 2)PPV increasing PVR and decreasing venous return.
CAUSES of PHTN / TYPES
SIGNS/SYMPTOMS:
- Chest pain 2/2 RV ischemia.
- Syncope 2/2 low C.O.
- S/S RV failure: hepatomegaly, ascites, and ankle edema (can resemble normal pregnancy).
PULMONARY HTN ANESTHESIA MANAGEMENT:
- MULTIDISCIPLINARY TEAM!!
- OB & Cardiac Anesthesia, OB&MFM, perfusionist/ECMO, hematology, cardiology(PHTN), ICU intensivist.
- ECHO: TTE to DX & ASSESS
- May need continuous POCUS/TTE during delivery w/ cardiac anesthesia*
- ECMO TEAM CONSULT: May require V-A ECMO if CV collapse*
- ECHO: TTE to DX & ASSESS
- BIGGEST RISK IS RIGHT AFTER DELIVERY as C.O doubles 2/2 increased preload and blood volume from autotransfusion (~700cc) puts huge strain on Right heart.
- Diuretics and inotropes (dobutamine, milrinone) are first line tx, be proactive and do not delay administration! Do not wait until signs of heart failure and decompensation to use these! Use them on delivery to support the huge cardiac strain we know is coming!
- DO NOT wean off any inotropes/CV meds needed during C/S, as cardiac strain from doubled C.O. and fluid volume shifts persists for days postpartum…she will continue to need the inotropic support –> transfer to ICU so she can stay on these gtts and be closely monitored**
- PLAN ICU post-delivery for monitoring/cardiac IV meds continued post-partum at least 48h
- 5-lead EKG
- A-line for HD monitoring. TLC CVP can be monitored, Swann has higher risks (more fragile vasculature in pregnancy & higher risk of vessel rupture)
- Can use Continuous CO monitoring if you have this available to assess effect of autotransfusion post-delivery on C.O. and also effect of diuresis and inotropic support
- Maintain pts prescribed pulmonary vasodilators
- Maintain Euvolemia** LIMIT FLUIDS! she will get enough of a fluid overload from auto-transfusion post-delivery.
- If normally using 500cc pit bag (we use 30u in 500cc, the 10u bolus = ~ 166cc over 10 minutes) this is too much of a fluid bolus..
- Instead dilute 10units pit into 10cc saline and give 3units (3ccs) every 3 minutes to effect, and OB can also use IU pitocin.
- Use smaller volume dilutions for antibiotics, and administer slowly.
- If normally using 500cc pit bag (we use 30u in 500cc, the 10u bolus = ~ 166cc over 10 minutes) this is too much of a fluid bolus..
- C/S with slow-dosed epidural is best, gentle onset to sympathectomy
- Will not tolerate huge HD swings.
- Vasopressin shown to be superior to phenylephrine in pHTN, as neo found to indiscriminately constrict pulmonary vasculature beds more than vasopressin does.
- NO CARBOPROST/HEMABATE: if bronchospasm occurs, carboprost will increase PVR 100%, and PAP 125% but HUGELY problematic in pts at risk of bronchospasm with pHTN
- AVOID METHERGINE: vasconstricton/HTN can worsen pHTN and cardiac strain.
- Pitocin and misoprostol(cytotec) safe.
- Avoid hypoxia (^^PVR 2/2 HPV reflex) – Give supplemental O2.
- Avoid hypercarbia – minimize narcotics.
- utilize adjuncts: NSAIDs, local/regional/TAP block
- Avoid ketamine – increases PVR
- Avoid N2O – increases PVR
- Avoid uterine exteriorization if possible:
- Any pt w/ pulmonary HTN or right heart compromise – ask obgyn not to exteriorize uterus after delivery – it causes tiny micro air emboli which in normal people isn’t going to cause huge issues, but in compromised pts will increase pHTN and exacerbate right-sided atfailur /PFO shunting.
Vasopressin vs Phenylephrine:
PRE-OP:
- Cardiac meds & team, adequate access, adequate IV channels, A-line, possible TLC for CVP, inotropes, pressors, PHTN meds.
IV INFUSION PLAN:
- (Pts often on oral sildenafil & neb iloprost)
- START PULM VASODILATOR MEDS PRIOR TO C/S.
- IV prostanoid low-dose:
- e.g.) 2 mcg/h of iv iloprost for 2h prior to C/S and continue 48-72 hours post-delivery.
- Manage fluid balance with SBP and CVP pressure at pre-delivery levels for first 24 h.
- Keep Hb> 9, ideally 10 g/dl.
- A rising CVP r/o fluid overload —> diuretics.
- Failure to respond to diuresis may mean RV struggling and needs inotropic support. (Frank-Starling curve)
- increase dose of iv prostanoid & can add of low-dose Dobutamine
- e.g.) 2 mcg/kg/min dobutamine & titrate to response.
- If pt still deteriorating despite increased doses of pulmonary vasodilators and inotropes w/ the development systemic HOTN
- add norepi & r/o other causes for deterioration – sepsis?
- increase dose of iv prostanoid & can add of low-dose Dobutamine
- Failure to respond to diuresis may mean RV struggling and needs inotropic support. (Frank-Starling curve)
**PLANNING BLOOD LOSS MANAGEMENT:**
- NO HEMABATE: bronchospasm would be catastrophic.
- NO METHERGINE d/t HTN
- Managing bleeding:
- Uterotonics: intra-uterine pit as 1st line!!
- No IV bolus pit dose to avoid both decreased SVR & the extra 166cc fluid bolus with the 10u IV pump bolus (at our hospital).
- Oxytocin 5u/hr gtt without bolus. Surgeon can give IU pitocin, less HOTN than IV.
- TXA may not be best choice – depending on coagulation status – may be hypercoagulable, esp F5Leiden with pulmHTN 2/2 clot burden
- B-lynch uterine compression suture for uterine atony
- Post-op JADA device to suction down uterus, or Bakri for tamponade
POST-OP:
- most dangerous period is POSTPARTUM.
- ICU CARE – MAINTAIN IV cardiac medication/inotrope support through post-partum period
- careful postpartum monitoring x minimum 48hrs
- VTE prophylaxis
- Stool softeners to prevent valsalva.
- Vaginal delivery not absolutely contraindicated, but not ideal – assc w/ vol changes during cxns —> problematic bc right heart can’t increase C.O. to accommodate volume changes with autotransfusion (300-500mL each contraction). Also pushing can have adverse valsalva hemodynamic effects. And a stat c/s would be a hot mess:
- If no epidural in place, or no time to slowly dose epidural (huge, rapid HD swings of spinal poorly tolerated) Cardiac stable induction of GA with etomidate & succs/roc
- Planned C/S delivery better choice: Epidural or low-dose CSE (intrathecal fent ~20mcg, and small dose bupi ~5mg max)
- GA disadvantages: cardiodepression by VAs, ^^ PVR during intubation & PPV.
124. Cardio-Obstetrics: Pregnancy and Pulmonary Hypertension with Dr. Candice Silversides