- Contents:
- Signs & Symptoms
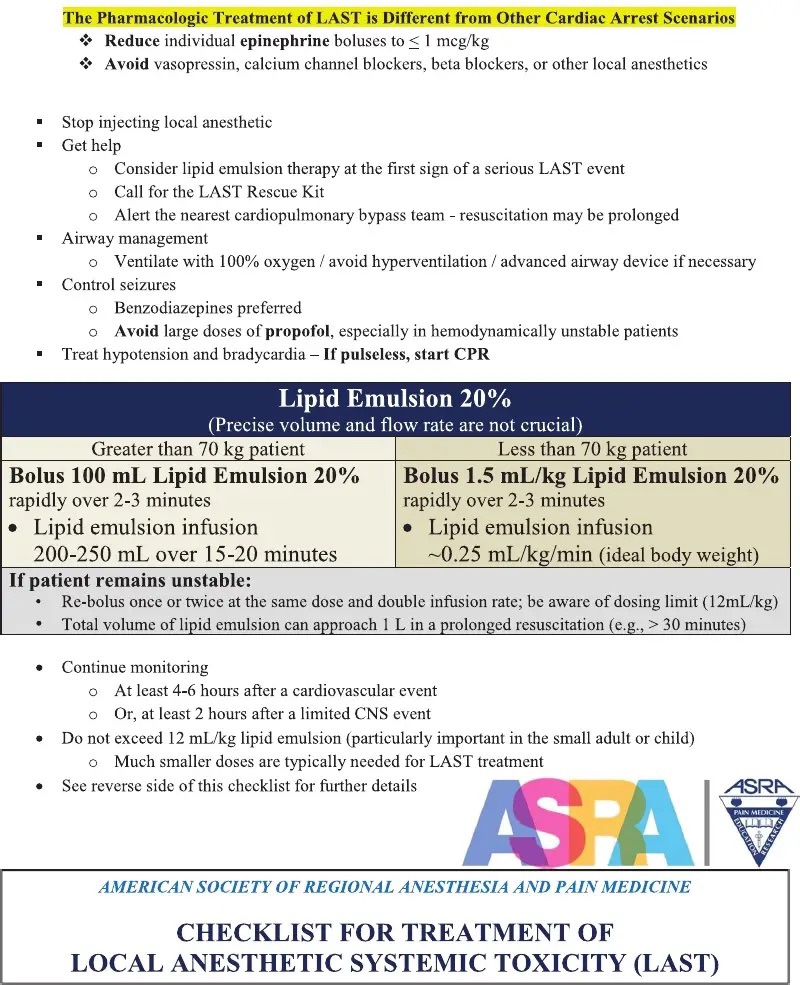
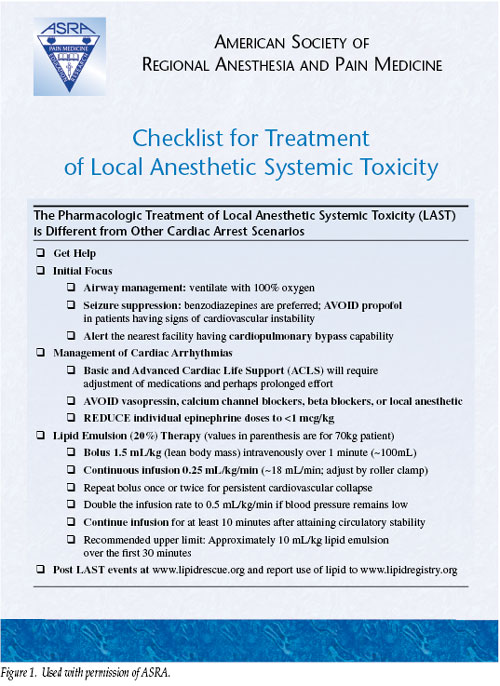
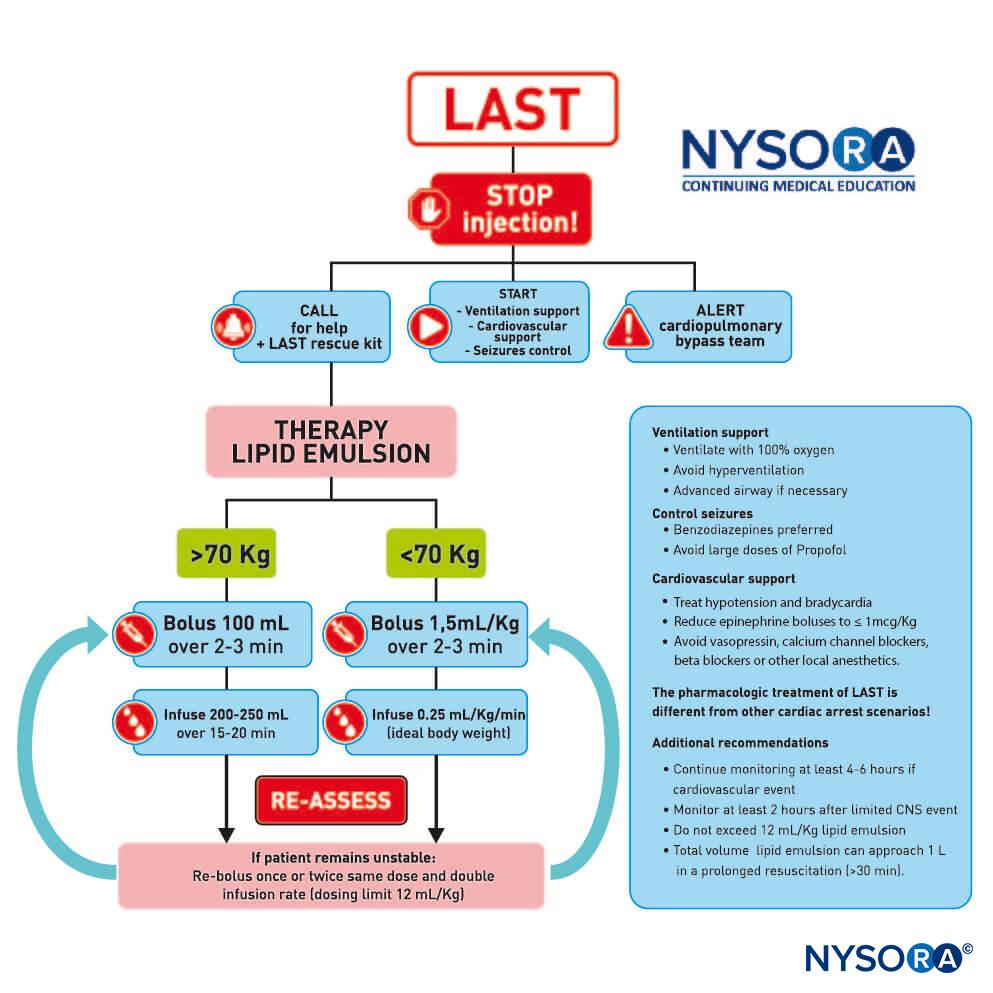
- LAST management & Established Algorithms
- Critical ACLS diffrences in L.A.S.T
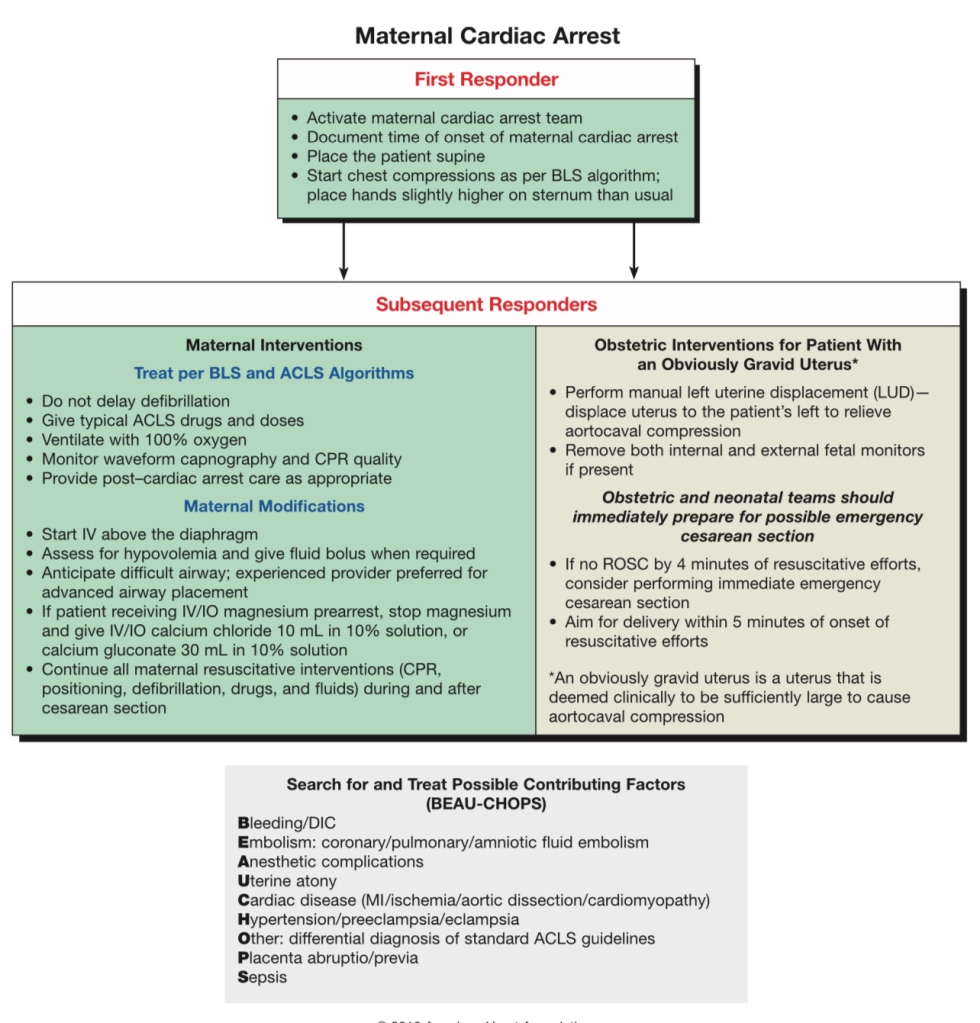
- Maternal Cardiac Arrest Algorithms
- IV LA Prevention
- 3% 2-Chloroprocaine
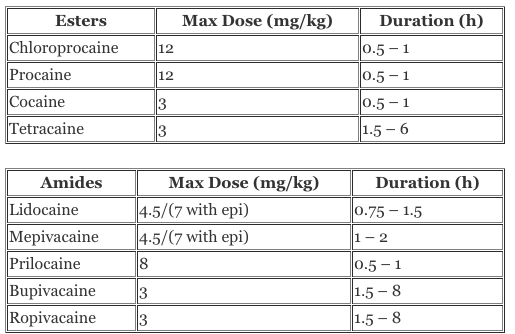
- Dosage Tables
- The Nitty Gritty of L.A.S.T:
- L.A. Mechanism Of Action
- Toxicity Physiology & Considerations: CNS, Cardiac & Hepatic
- Signs & Symptoms Explained
- Pregnancy Physiology & It’s Increased Risk Factors
LAST is most likely when using large LA lido bolus to convert labor epidural to surgical block for C/S using 20cc 2%lido w/ epi 1:200,000 (=400mg). This dose is greater than the max dose of IV lido, and pregnancy physiology makes women more sensitive to LA toxicity.
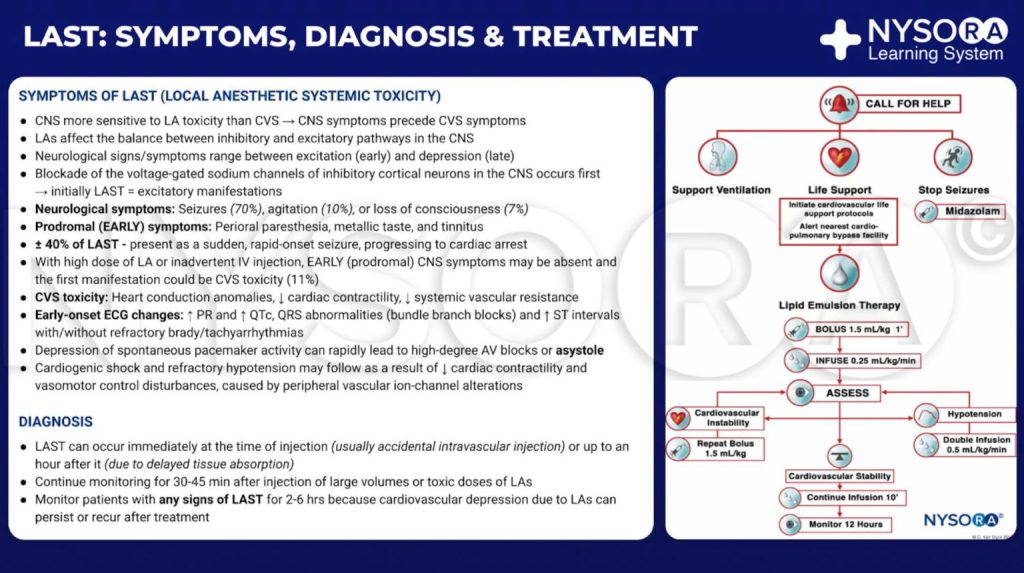
MANAGING L.A.S.T:
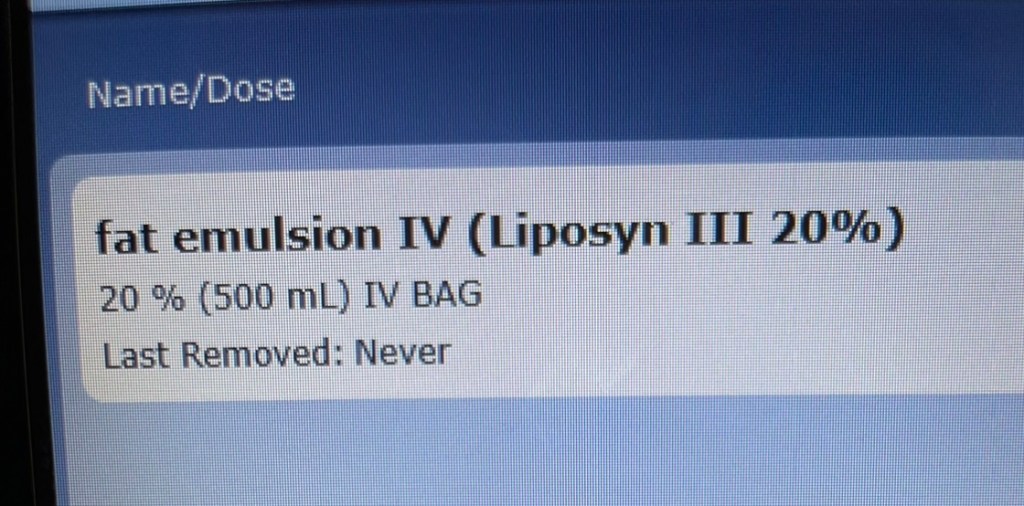
USE INTRALIPID/FAT EMULSION AS MAIN TREATMENT. (stored as “fat emulsion” in HH Pyxis)
DOSING: 1.5mL/kg BOLUS x 1 min, 0.25mL/kg/min INFUSION, RE-BOLUS 1.5mL/kg x 1 min, Increase to 0.5mL/kg/min if HOTN persists
In CV Collapse:
INTUBATE & USE CPR TO CIRCULATE FAT EMULSION, AND CONTINUE CPR UNTIL INTRALIPID DOSING EFFECTIVE WITH ROSC, OR CPB MUST BE INITIATED:(ACLS: SMALL* doses EPI. NO vaso/BB/CCB)
LEFT UTERINE DISPLACEMENT IN OB CPR
STAT Cesarean delivery if mom has CV collapse > 4min
- STAT C/S is to increase maternal survival via improved CPR without gravid uterus, not for fetal prioritization. Mom surviving is the priority here.
- Perimortem stat C/S at 4 minutes if ROSC not achieved – covered further down
*CRITICAL ACLS DIFFERENCES IN L.A.S.T*
- NO VASOPRESSIN:
- across all sources it’s recommended to avoid vasopressin – associated with poor outcomes – [also one source claimed it can cause pulmonary hemorrhage] Likely 2/2 high SVR impairing cardiac output. Avoiding high SVR may also be reason behind smaller epi dose recommendation.
- SMALL EPI ACLS DOSES –1mcg/kg
- ~ 70-100 mcg for most pts (= 1cc of 10cc bristajet syringe: (1mg in 10 cc: 1000mcg10cc = 100mcg/cc)
- If seizures – GIVE BENZO
- (avoid propofol – can worsen acidosis and cause cardiac depression/HOTN)
- AVOID CCB and BB therapy – worsens cardiac function.
- IF VENTRICULAR ARRHYTHMIA —> GIVE AMIODARONE 300mg 1st dose, then 150mg 2nd dose if needed
- IF VENTRICULAR ARRHYTHMIA —> GIVE AMIODARONE 300mg 1st dose, then 150mg 2nd dose if needed
INTRALIPID THERAPY GUIDELINES
1.5mL/kg BOLUS x 1 minute
0.25mL/kg/min INFUSION
CPR to circulate meds
RE-BOLUS 1.5mL/kg x 1 minute
Increase to 0.5mL/kg/min if HOTN persists
RE-BOLUS 1.5 mL/kg if peristant CV collapse.
Continue CPR to circulate meds and allow them time to work.
Continue CPR —> if no ROSC —> Cardiac bypass until LA has cleared.
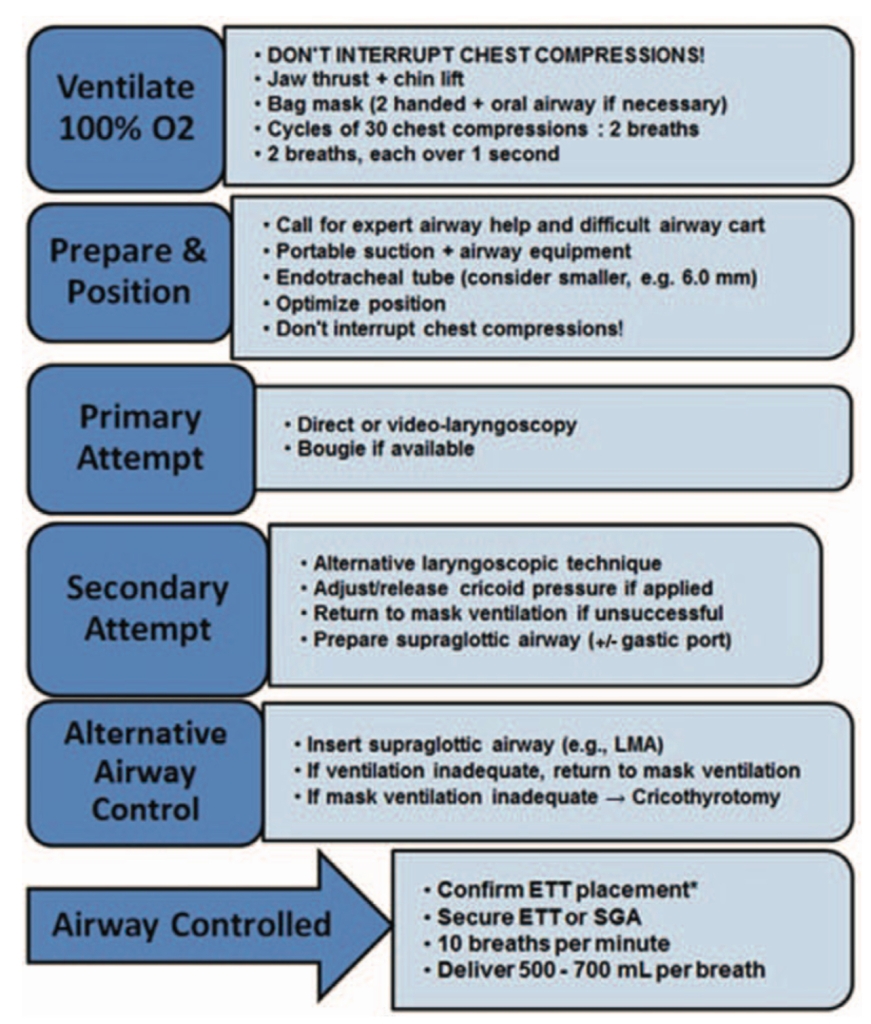
- Initial management of LAST should be focused on airway management, circulatory support, and reduction of systemic side effects.
- Immediate ventilation & oxygenation to prevent hypoxia and acidosis can facilitate resuscitation and reduce likelihood of progression to seizures or CV collapse.
- If seizures do occur, immediate administration of benzodiazepines is recommended, to prevent injury & acidosis.
- Propofol or thiopental ok if benzos unavailable. However, these may worsen any assc HOTN or cardiac depression. If these meds cannot control tonic-clonic seizure movements, small doses of succinylcholine should be intermittently administered to stop muscular activity, and further acidosis.
- Quick Note: WHY succs and not Roc? In status epilepticus succs can allow determination of whether seizure has been controlled. With Roc, risk that pt may have unobservable ongoing seizure activity which is still causing brain damage. (although subsequent succs doses may produce ++ bradycardia – glyco should treat this) HyperK+ 2/2 to rhabdo takes time to develop, so status epilepticus of short duration (<15-20 min) itself is not a contraindication to succs. HOWEVER for a pt who presents to the ED with seizure of unknown duration, Roc is safer (unknown K+, unknown rhabdo status). Alternatively, this may be one situation in which sedative-only intubation may be a reasonable approach (in otherwise HD stable pt), as high-dose propofol will typically provide good intubation conditions provided that it breaks the seizure.
- Propofol or thiopental ok if benzos unavailable. However, these may worsen any assc HOTN or cardiac depression. If these meds cannot control tonic-clonic seizure movements, small doses of succinylcholine should be intermittently administered to stop muscular activity, and further acidosis.
Rapid Sequence Termination (RST) of status epilepticus
MATERNAL CARDIAC ARREST
If no ROSC in 4 minutes – Emergent crash C/S bedside no matter where you are – could be in L&D room. C/S is to facilitate Maternal CPR and rescucsitation for maternal survival, not for fetal benefit.
Podcast episode – worth the listen: When mom codes and needs a crash section:
SOAP Maternal Cardiac Arrest algorithm:
SOAP algorithm for Airway Management during CPR:
Intravascular LA Prevention:
ASPIRATE EVERY CATHETER PRIOR TO INJECTION. CAN FLUSH WITH 1-2cc PRIOR TO ASPIRATION, BUT ALWAYS ASPIRATE.
- Look for s/s IV epi: HR/BP increase You won’t always be able to aspirate blood back in an IV epidural catheter, but signs of IV epi: increased HR/BP, along with signs of IV lido: tinnitus, metallic taste in mouth can clue you in. Additionally an IV catheter will NOT give epidural block coverage.
- “Intravascular test dosing, specifically with epi, is a reliable method of prevention. If within 1 min of injection, HR increases by 10+ bpm, or the SBP rises by 15+ mmHg, 10 to 15 micrograms/ml of intravascular test dosing with epinephrine has a sensitivity of 80%. But certain pt characteristics which can render this test unreliable. Eg: pts under GA or neuraxial anesthesia, sedated pts, elderly, or pts taking beta-blockers.”
WHAT ABOUT 3% 2-Chloroprocaine?
- 3% 2-Chloroprocaine (ESTER) has relatively no protein binding, so this element of increased sensitivity 2/2 less protein binding does not apply, additionally rapid plasma metabolism by pseudocholinesterases drastically reduces risk of systemic toxicity.
- 3% chloroprocaine = 30mg/cc. 20cc for epidural conversion = 600mg, is below regional max dose.
- The max dose of chloroprocaine for infiltration, or PNB:
- plain: 11 mg/kg, not to exceed 800 mg.
- with epi 1:200,000: 14 mg/kg , not to exceed 1000 mg.
- The max dose of chloroprocaine for infiltration, or PNB:
- 3% chloroprocaine = 30mg/cc. 20cc for epidural conversion = 600mg, is below regional max dose.

Chloroprocaine – StatPearls – NCBI Bookshelf
https://www.ncbi.nlm.nih.gov/books/NBK499964/#_arti
Local Anesthetic Toxicity – StatPearls – NCBI Bookshelf
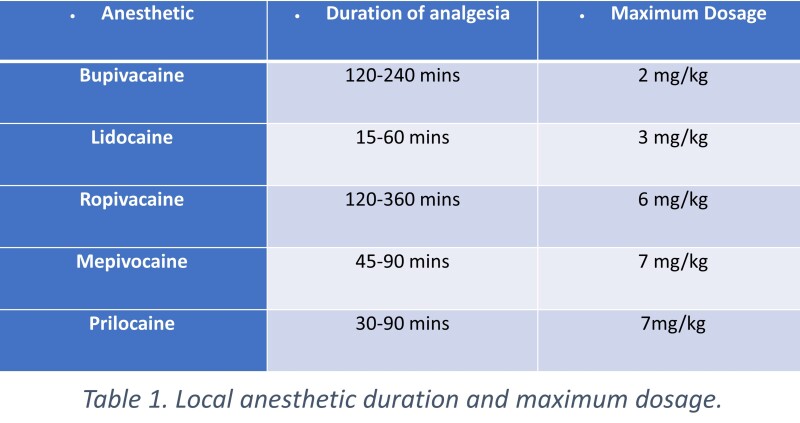
DOSAGE TABLES
- *LAs also have differing intrinsic vasoactive effects. Levobupivacaine and ropivacaine have dose-dependent vasoactive properties that may potentially prolong duration and slow systemic absorption, as opposed to bupivacaine which has vasodilatory properties and may lead to more rapid systemic absorption.



THE NITTY GRITTY OF L.A.S.T
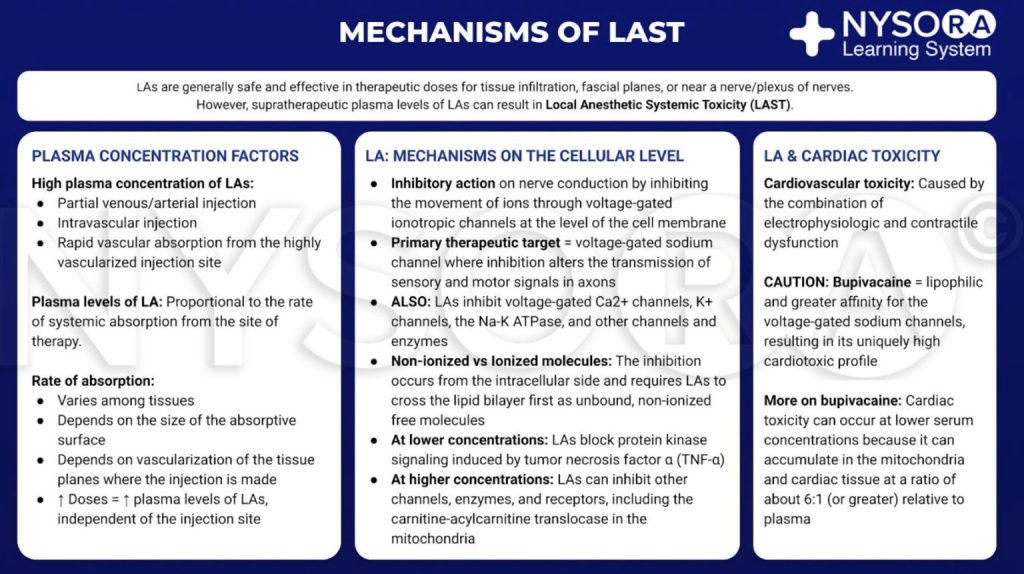
- LA agents exert their effect by attaching to the intracellular domain of the NaV channel. This inhibits neuronal ion transfer and depolarization, and prevents neuronal transmission.
- LAs may also bind to and block K+ channels, Ca2+ channels, the Na+–K+ ATPase channel, as well as several other targets.
- Notably, LAs can interfere with intracellular and transmembrane cell signaling, affecting the metabolic processes of cAMP, protein kinase B (Akt), and 5-adenosine monophosphate activated protein kinase (AMPK), among other stimulatory kinases.
- LAs have also been shown to impair mitochondrial metabolism, ATP production, inhibit the ryanodine receptor at the sarcoplasmic reticulum, and reduce Ca2+ sensitivity of myofilaments.
- The many LA targets (Figure 2), below, explain the complex mechanistic and clinical picture of LAST.

Published online 2018 Aug 8. doi: 10.2147/LRA.S154512
Toxicity Physiology & Considerations: CNS, Cardiac & Hepatic
CNS Toxicity
- Increasing plasma concentrations of LA 1st compromises cortical inhibitory pathways via NaV channels blockade, disrupting inhibitory neuron depolarization.
- Inhibiting these pathways leads to excitatory s/s of sensory & visual changes, muscular activation, and subsequent seizure activity.
- As the plasma concentrations of LA rise, excitatory pathways are affected, producing a depressive phase of neurological toxicity, with loss of consciousness, coma, and respiratory arrest.
- CNS toxicity is another important consequence of LAST. While it is comprised of many initial prodromal features, it most often manifests as seizures.
- One mechanistic theory is centered around Twik-related acid-sensitive K+ channels (TASK).
- These pH-sensitive channels generate neuronal potassium “leak” currents.
- Local anesthetic inhibition causes membrane depolarization and increased neuronal excitability. As these channels are expressed throughout the brain, this is the suggested mechanism for seizures in this setting.
Cardiovascular Toxicity
- The many LA molecular targets produce complex toxic features in the CVS: conduction disturbances, myocardial dysfunction, & lability of peripheral vascular tone.
- Primary effects likely arise from rhythm disturbance, with other CVS effects being secondary. Normal conduction disrupted by direct Na+ channel blockade, chiefly at the bundle of His.
- By driving the resting membrane potential to a more negative level, action potential propagation is impaired, leading to prolonged PR, QRS, and ST intervals. Re-entrant tachyarrhythmias and brady-arrhythmias ensue, which may be worsened by further K+ channel blockade, prolonging the QT interval.
- Primary effects likely arise from rhythm disturbance, with other CVS effects being secondary. Normal conduction disrupted by direct Na+ channel blockade, chiefly at the bundle of His.
- Myocardial dysfunction has several contributory mechanisms.
- Ca++ channel and Na+–Ca2+ exchange pump blockade diminishes contractility by reducing intracellular Ca++ stores.
- The net result of interruption of Akt(protein kinase B), AMPK(5-adeonosine monophosphate activated protein kinase), thereby interrupting insulin-driven intracellular glucose metabolism, along with the reduction of intracellular ATP reserves, and impaired cAMP production further contributes to reduced myocardial contractility (Figure 2).
- A direct pH-related suppressive effect of LAs is exerted on the neuronal control mechanisms of baroreceptors, as well as a negative effect on systemic vascular tone.
- Patients with severe cardiac dysfunction are particularly susceptible to LA-induced myocardial depression and arrhythmias due to reduced hepatic and renal perfusion leading to reduced metabolism and elimination, respectively.
- Poor perfusion to the injection site may reduce the peak plasma concentration of LA, but if circulation time is prolonged, the detection of an intravenous injection of LA (by detection of a tracer substance such as epinephrine) may be delayed.
- Dose reduction is unnecessary in mild–moderate heart failure where tissue perfusion is preserved, but is recommended in severe heart failure.

Hepatic Dysfunction and LAST
- Isolated hepatic dysfunction does not necessitate dose adjustment for single-shot regional anesthetic techniques despite a reduced hepatic clearance of LAs.
- A larger volume of distribution and maintenance of α1-acid glycoprotein synthesis provide a safety margin in pts with hepatic disease.
- However, in pts receiving repeated boluses or continuous infusions of LA, or those with coexisting cardiac or renal disease, dose reduction is recommended
SIGNS & SYMPTOMS
- Early recognition of CNS & cardiac toxicity critical.
- After single LA injection, LAST presented within 50 sec in 50% of cases studied, and within 5 mins in 75% of cases. If potentially toxic dose administered, should observe pt for at least 30 mins.
- LAST can have DIVERSE, ATYPICAL S&S, but most commonly presents with CNS changes.
- ~ 40% of LAST presents atypically
- ~ 30-80% CNS toxicity, primarily as seizures.
- ~ 20% isolated CV distrubances: variable features: dysrhythmias, conduction deficits, HOTN, and eventually cardiac arrest (usually asystole)
- Initial S&S LAST:
- Agitation, confusion, dizziness, drowsiness, dysphoria, audito-visual changes, tinnitus, perioral numbness, metallic taste, & dysarthria, dysgeusia(altered taste), or reduced LOC.
- Without adequate recognition & treatment, these s/s can progress to seizures, respiratory arrest, cardiac arrest and/or coma.
- While CNS toxicity often presents with the above initial features, most common consequence is seizures. Esp with IV injection – seizures can be the initial presentation.
- Historically, LAs thought to often show CNS tox befor CV tox, but with more potent LAs, cardiac tox can arise concurrently with seizures or even before.
- HOTH and bradycardia often 1st signs of cardiac tox. But arrhythmias are responsible for most reported cases, most commonly bradyarrhythmias.
- More s/s cardiac tox: hypertension, dyspnea, pain, wide complex, ST-segment changes, asystole, tachycardia, and ventricular ectopy/tachycardia/fibrillation.
PREGNANCY INCREASES RISK OF LA TOXICITY:
- 20cc 2% lido = 400mg IV lidocaine if catheter is Intravascular.
- Max dose lido for Local infiltration = 5mg/kg, 7mg/kg with epi.
- But these recommendations are for non-IV administration, as epi would constrict capillaries and reduce speed of systemic uptake. Versus an IV injection where epi vasoconstriction would have no effect on vascular uptake…as we’re injecting this right into a larger vessel…
- For comparison, IV recommendations for lido gtts include a 1-3mg/kg bolus (LESS THAN HALF OF LA INFILTRATION MAX DOSE) followed by up to 1.5 mg/kg/hr continuous IV infusion.
- These IV doses are SIGNIFICANTLY lower than the max doses we learn for regional/neuraxial blocks.
- So for a 70kg non-pregnant woman, 350mg is the max dose for local… but 400mg is routinely given to convert labor epidurals, and could be a toxic dose if given IV.
- These IV doses are SIGNIFICANTLY lower than the max doses we learn for regional/neuraxial blocks.
- The max dose of plain chloroprocaine for infiltration, or PNB is 11 mg/kg, not to exceed 800 mg.
- with epi 1:200,000: 14 mg/kg , not to exceed 1000 mg
PREGNANCY-SPECIFIC PHYSIOLOGY CHANGES & LA TOXICITY
- Epidural vein engorgement makes IV catheter migration more likely
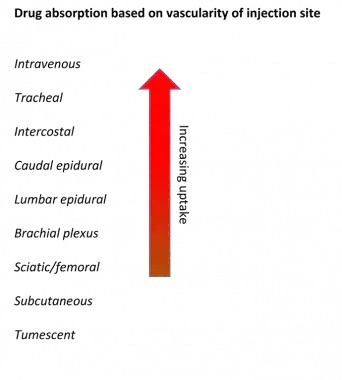
- Higher C.O. in pregnancy increases perfusion of potential vessel-rich-group target sites –> more rapid uptake&absorption –> toxicity
- Mom’s pH is at slightly higher end of normal from respiratory alkalosis 7.4 -7.45 (resp alkalosis from progesterone stimulating respiratory centers) (metab acidosis; kidneys excrete more bicarb to compensate for low PaCO2~32 mmHg): higher pH can also theoretically increase non-ionized free bioavailable fraction of weak-base LA (pKa)
- Decreased AAG (Alpha1 acid- glycoprotein) in pregnancy: less protein binding of LA weak base = increased free fraction of drug
- If cardiac arrest develops in parturients, resuscitation complicated by above-mentioned physiological changes of pregnancy, including aortocaval compression by gravid uterus (reduced venous return and C.O, causing HOTN and aggravating the pathophysiology of the cardiac arrest.)
- Thus, even with minor suspicion of LAST, these pts should be managed aggressively to prevent morbidity and mortality.
- Hormonal effects of estradiol & progesterone appear to alter cardiac myocyte electrophysiology enough to increase risk of arrhythmias, and of cardiotoxicity in general.
Local anesthetic systemic toxicity: current perspectives – PMC