CONTENTS:
- Nerve fiber type review
- Labor stages and associated nerve pathways
- Differential blockades in neuraxial anesthesia
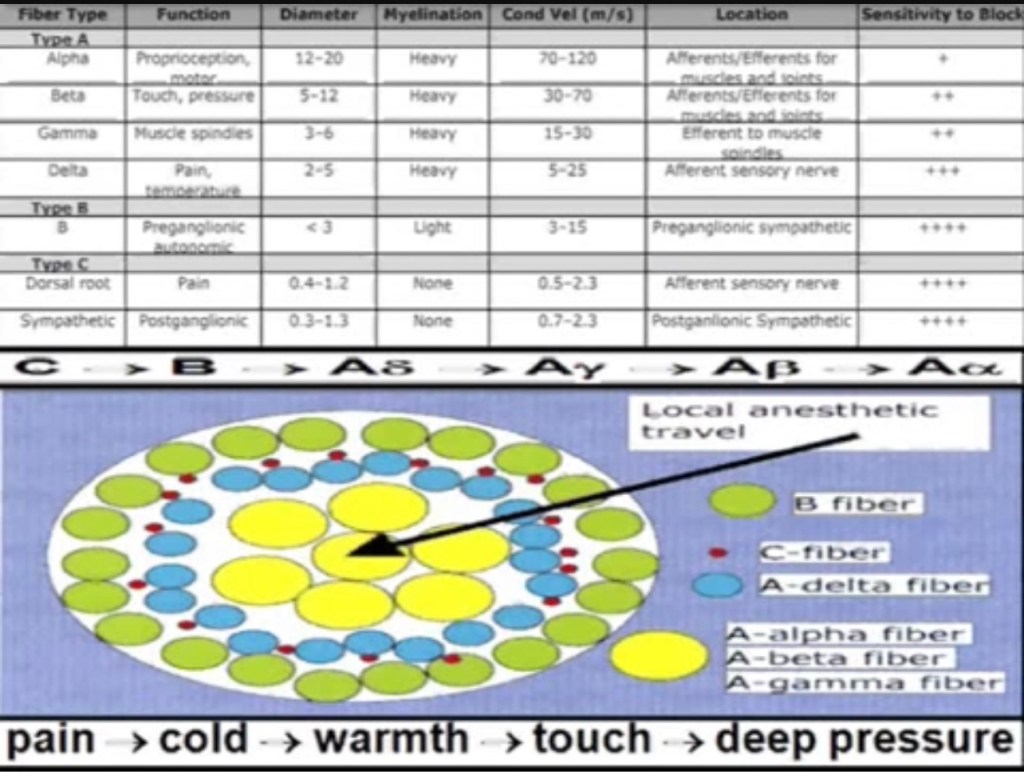
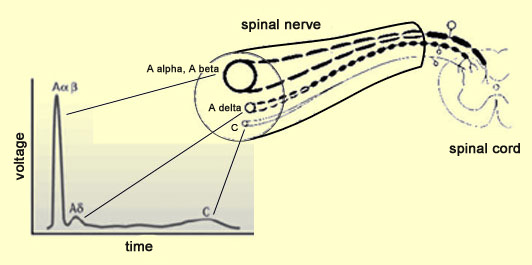
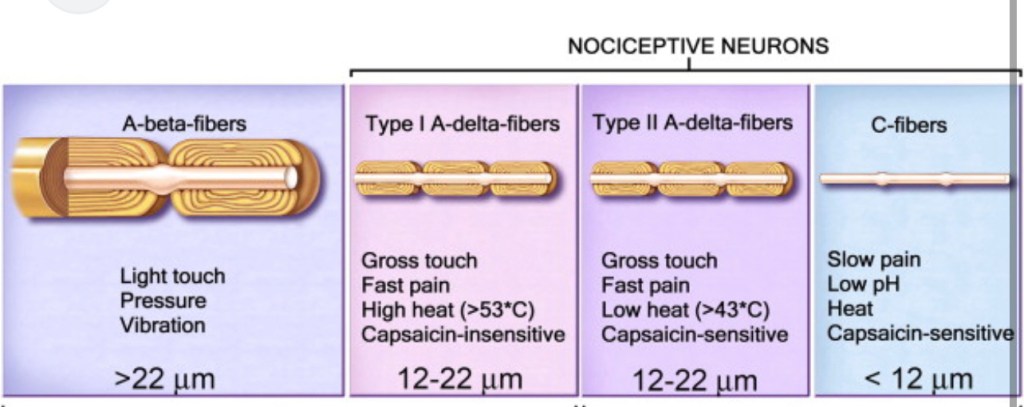
LAs block voltage-gated Na+ channels to inhibit action potentials in nociceptive fibers, blocking transmission of pain impulses to the dorsal horn. Importantly, A-delta fibers carrying nociception (sharp pain from tissue damage), and C fibers (dull slow pain). Somatic pain is dull pain from bones/joints/tendons/muscles – similar to visceral pain. Nociceptive pain is sharp pain from tissue damage (surgery)
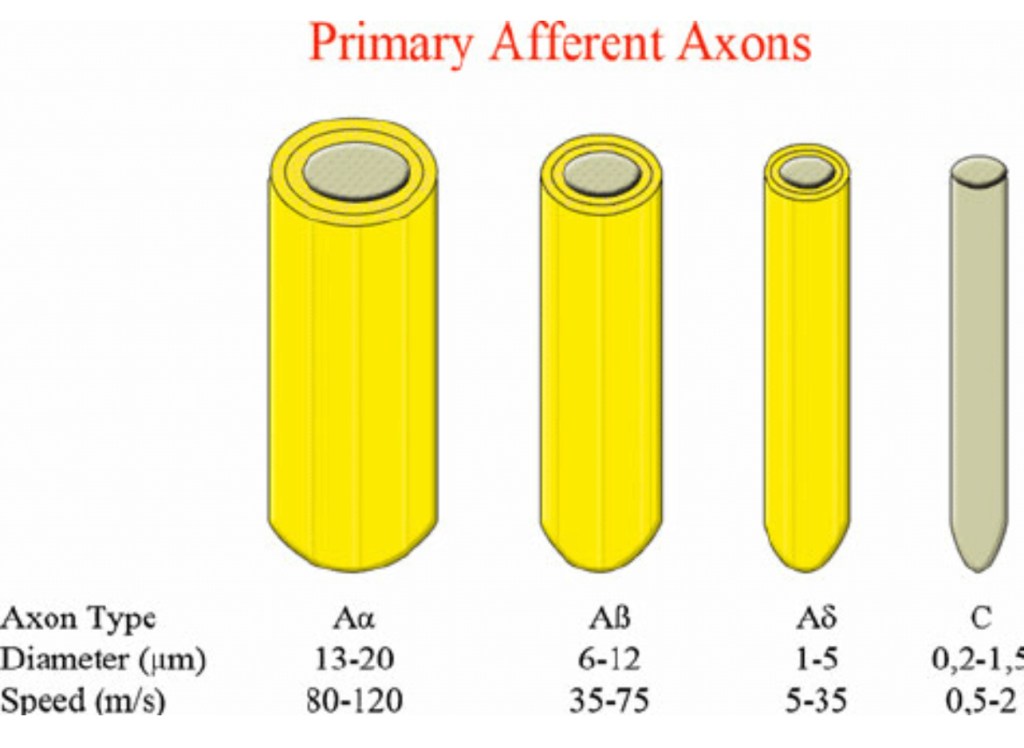
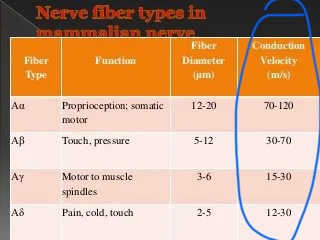
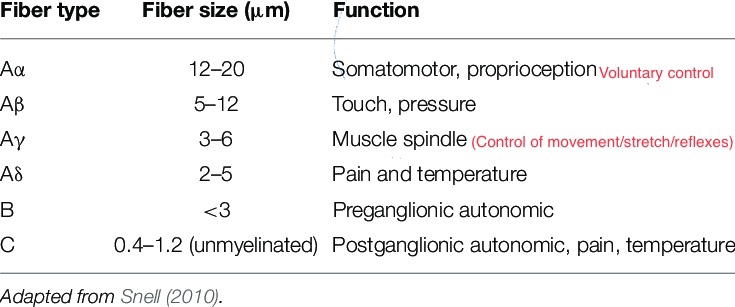
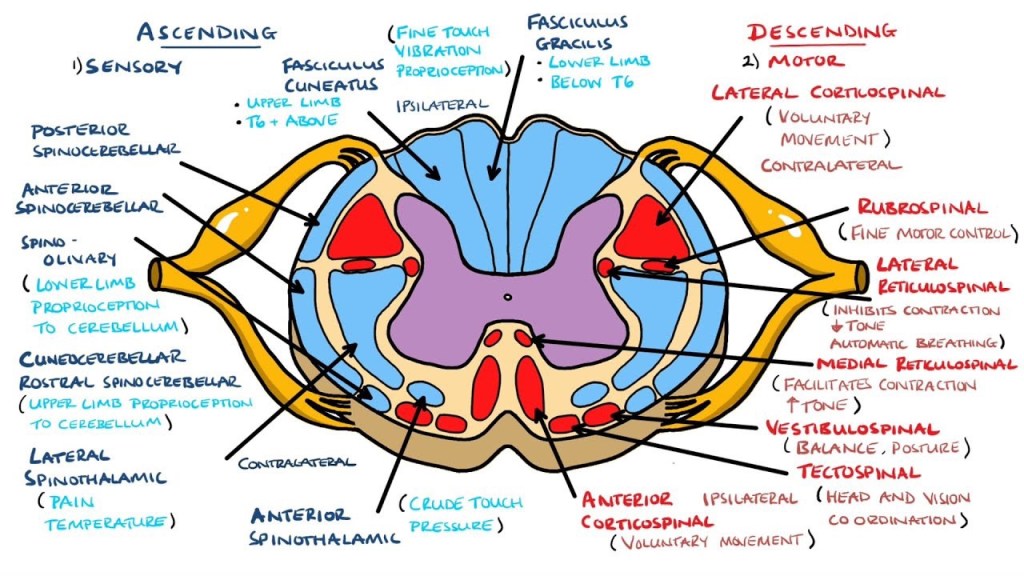
- Aα fibers: supply skeletal muscle: motor and proprioception
- Aβ fibers transmit tactile sensation (pressure, touch)
- Aγ fibers provide innervation to muscle spindles
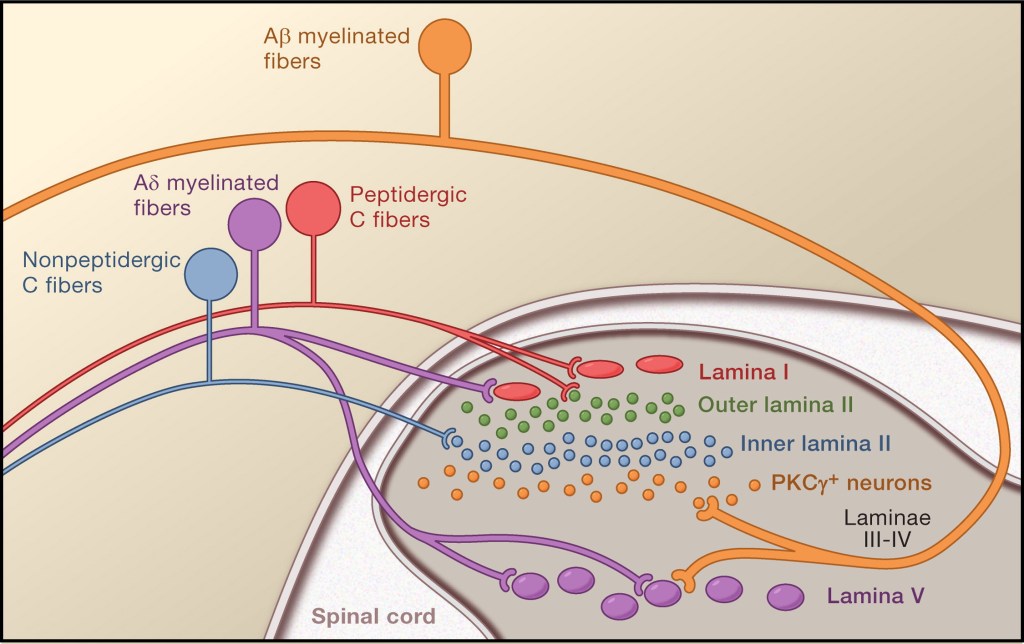
- Aδ fibers transmit nociception(pain) and cold.
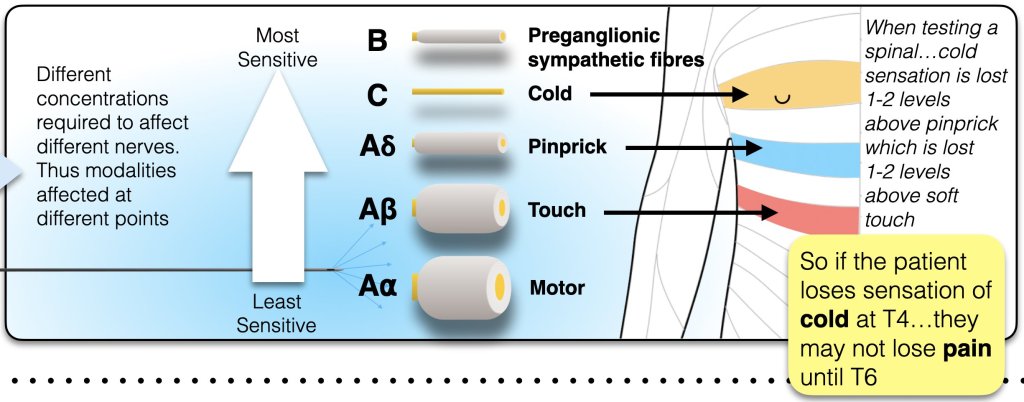
Block occurs in step-wise fashion, with smallest diameter and unmyelinated fibers easiest to block:
- 1st: small diameter Myelinated Autonomic (B-fibers) —> vasodilation
- Then unmyelinated C fibers first (cold, dull, slow pain & visceral pain )
- Then myelinated sensory impulses (A-delta) – sharp pain
- Then myelinated A-beta (pressure)
- Then myelinated motor (A gamma, A-alpha)
PHARMACOLOGY OF EPIDURAL BLOCK
NYSORA:
“An understanding of the physiology of nerve conduction and the pharmacology of LAs is essential for successful epidural block. Potency and duration of LAs, preferential block of sensory and motor fibers, and the anticipated duration of surgery or need for postoperative analgesia are factors that should be considered before initiating epidural block. This section covers several practical aspects of attaining effective epidural anesthesia and analgesia.
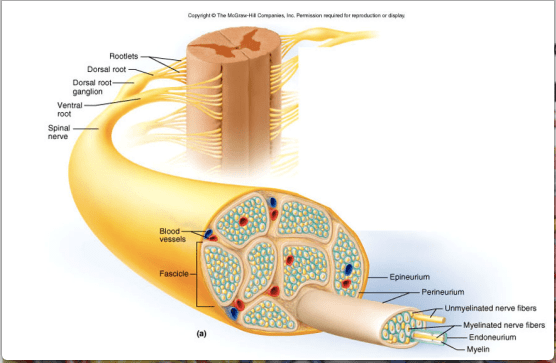
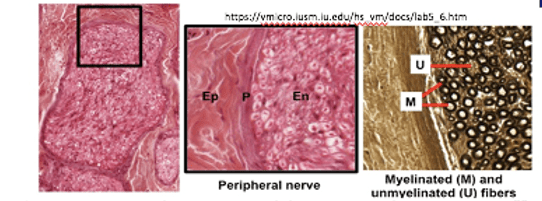
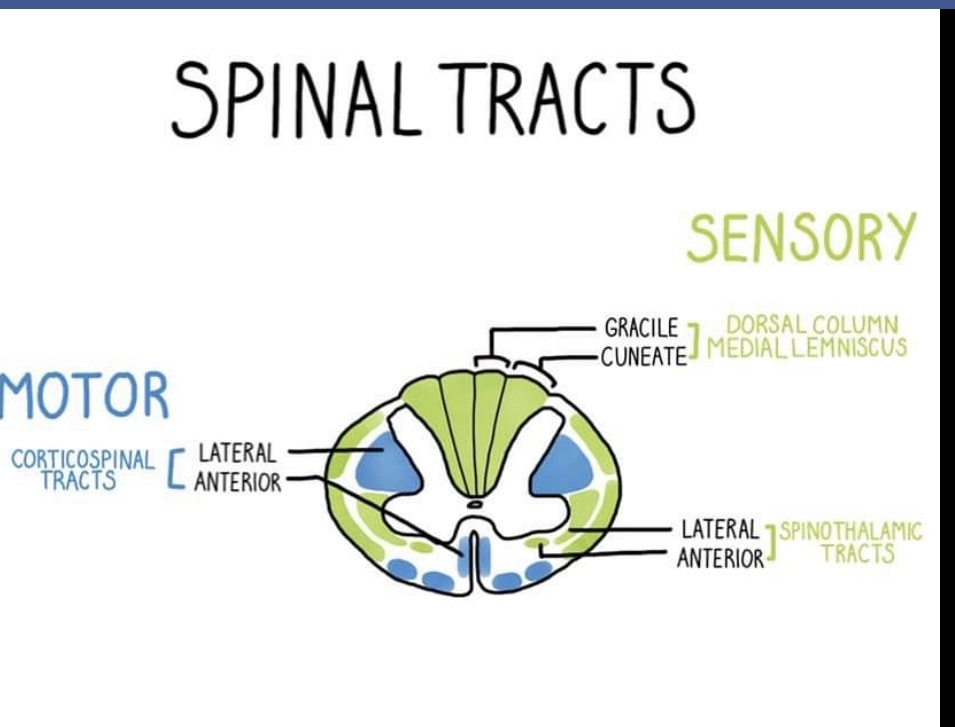
Epidural solutions may contain an LA with or without an adjuvant drug. Dose, volume, and concentration, as well as site of injection, of the LA solution vary, resulting in different pharmacodynamic effects. A, B, and C nerve fibers vary in size and in the presence of a myelin sheath. A-delta and C fibers are responsible for temperature and pain transmission. B fibers are autonomic fibers. The larger A fibers (especially A-alpha fibers) are motor fibers. C fibers are unmyelinated and smallest in size. Because they lack a protective myelin sheath and diffusion barrier, they are blocked rapidly. A and B fibers are myelinated and larger in size than C fibers. B fibers are responsible for autonomic nervous system transmission. They are smaller in size than A-delta fibers, but larger than C fibers. It is widely accepted that autonomic fibers are more susceptible to LA nerve block than sensory fibers. Epidurally administered LA preferentially nerve blocks sympathetic neural function; this explains the more extensive sympathetic dermatomal block when compared with sensory and motor nerve blocks. However, Ginosar et al recently suggested that sensory function was more susceptible to block than sympathetic function. Several other studies concurred. The dose and concentration of LA used may account for the different findings in these studies. Because of their thick myelin sheath, motor fibers require much more LA and much more time before an adequate nerve block is achieved.
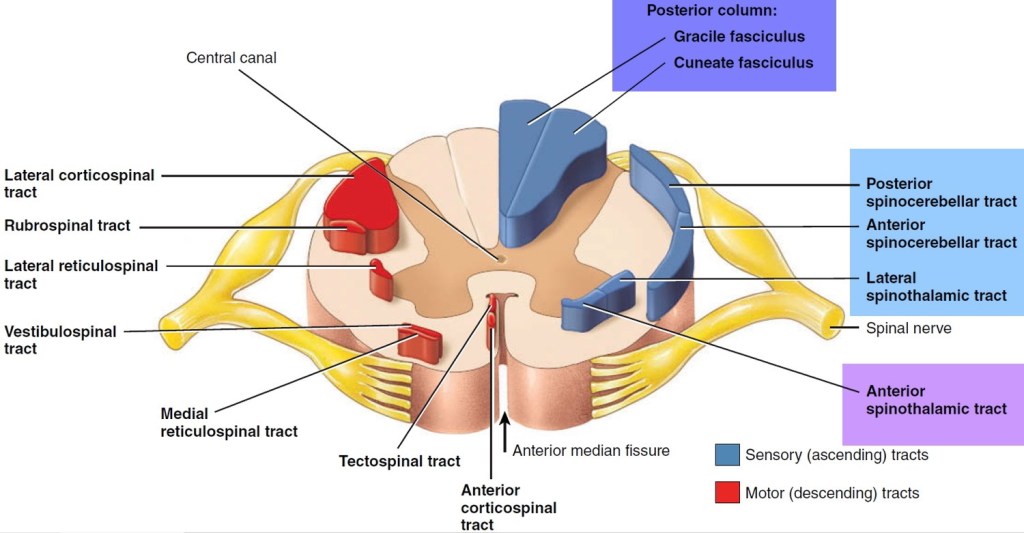
Local anesthetics produce reversible nerve block by blocking sodium passage through the nerve membrane. When LA is injected into the epidural space, several things occur. Most of the injected LA is absorbed into the venous blood, and a large part is retained in epidural fatty tissue. The primary sites of action of an epidurally administered LA are the ventral and dorsal nerve roots that pass through the epidural space. However, based on studies using labeled LAs, LAs can cross the dura and penetrate the spinal cord, but to a lesser extent than their penetration into the spinal nerve roots. The segmental nerve roots are mixed sensory, motor, and sympathetic nerve fibers. Hence, all three types of fibers will be affected (to varying degrees).”
Episode 76: Pain Pathways with Mark Bicket
STAGES OF LABOR & ASSOCIATED FIBERS/PATHWAYS
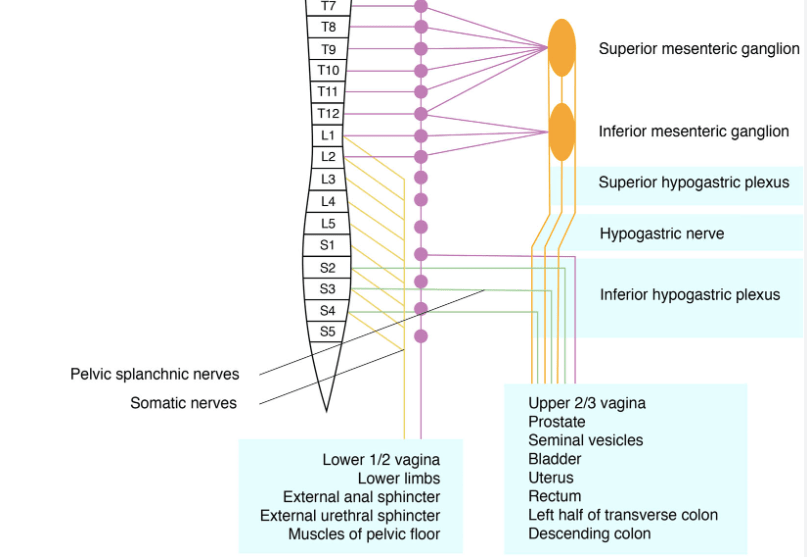
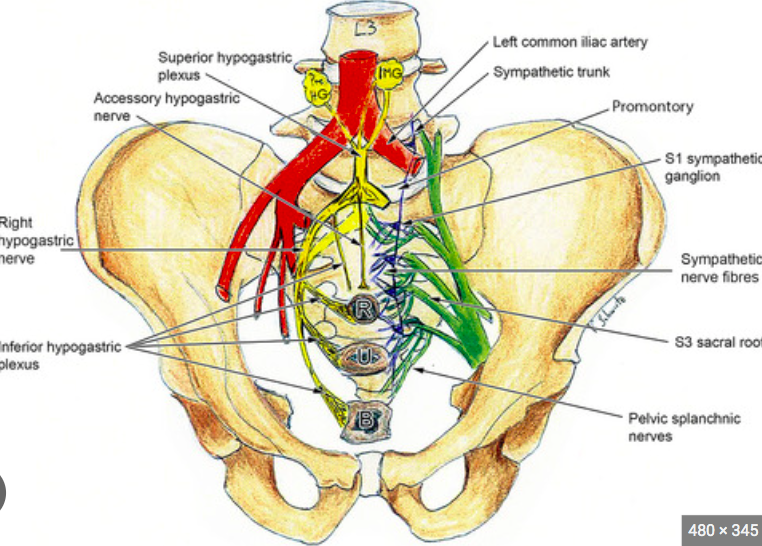
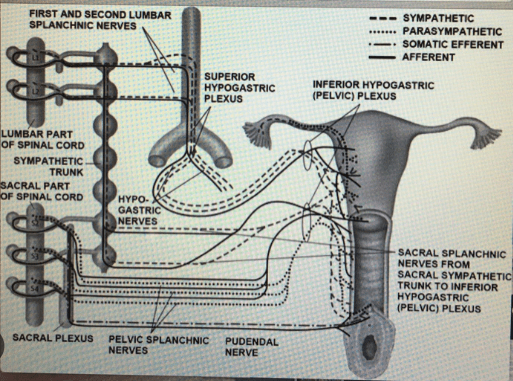
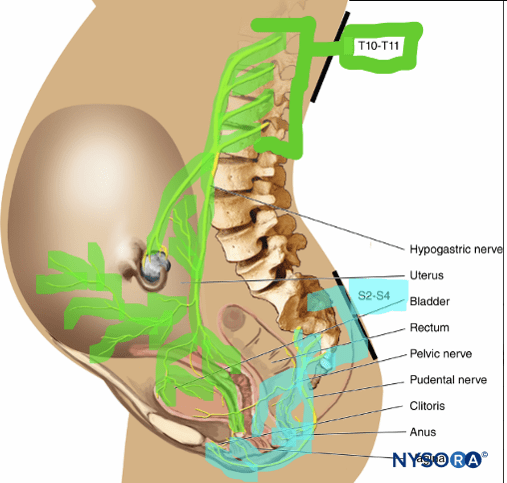
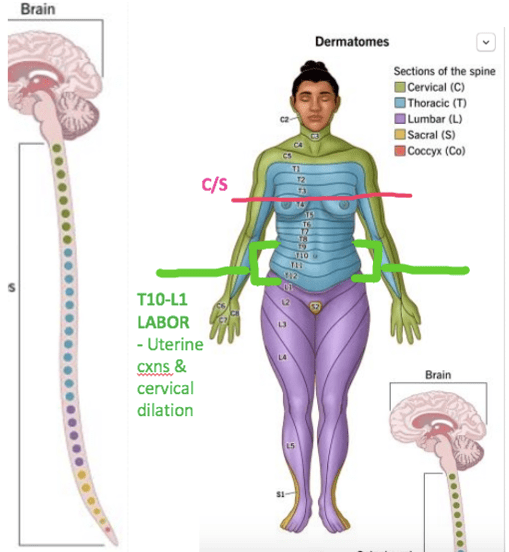
- 1st stage of labor (0-6cm, cervix slowly dilating & effacing)
- pain is caused by distension of the cervix and low uterine segments in combination with isometric contraction of the uterus.
- Visceral pain (C-fibers) also A-delta
- Dermatomes T(11) & T(12) in the early stage of labor, spreading out to T(10) & L(1)
- Covers paracervical & hypogastric plexus: stemming from superior and inferior and mesenteric ganglion.
- All originating from lumbar sympathetic chain
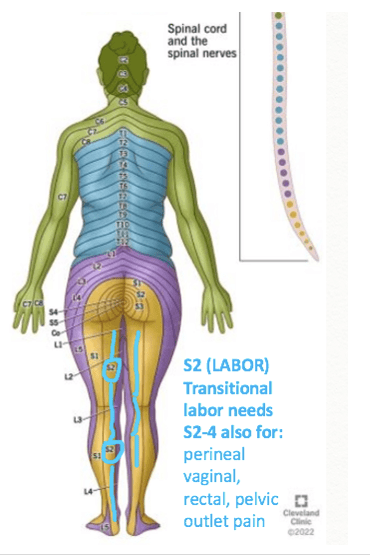
- 2nd stage of labor eventually involves dermatomes S2 – S4 (pudendal nerve).
- Somatic pain (A-beta, A-delta) also C-fibers still carrying visceral pain signals & ischemic pain
- Pain from tissue damage in pelvis & perineum from stretching tendoms, ligaments & tissues. Activation of nociceptors partly resulting from ischemia. (Uterine cxns release: bradykinin, histamine, 5HT, leukotrienes, prostaglandins, substance P & lactic acid that act on chemoreceptors. Thought to be result of myometrial ischemia)
- Activates C-fibers from cervix & lower uterine segments, and afferent A-delta and C-fibers from pelvis, pelvic organs and perineum. A-beta (large diameter fibers) carries pressure signals, which may explain prevailing pressure in late labor despite working epidural, requiring additional fentanyl for relief.
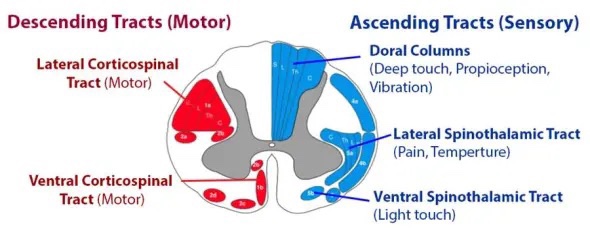
Differential Sensory Blockade
LA penetrating and blocking nerve fibers depends on various factors:
- Size, surface area, & degree of myelination
- Not all nerve fibers blocked at identical concentrations
- ie: not all sensory modalities blocked at identical concentrations
- sympathetic B-fiber blockade highest (2-6 levels higher than sensory)
- 2-6 dermatomes lower: anesthesia to cold (C-fibers)
- 2 dermatomes lower*: anesthesia to pinprick*(A-delta)
- 2 dermatomes lower: anesthesia to touch (A-beta)
- 2 dermatomes lower: motor blockade (A-alpha)