CONTENT:
- Pre-op Interview
- Contraindications to Neuraxial
- About Spinals/Neuraxial – NYSORA
- Local anesthetics & doses we use
- Placement tips
- Management of Cesarean Sections
- Room Setup
- Case breakdown & highlight reel for cesarean under neuraxial anesthesia
- Anesthetic Management
- Physiologic Responses to Neuraxial
- High Spinal/Total Spinal
- Failed Epidural & Failed Spinal
- Physiologic Changes After Delivery
- How to Manage a Spinal Wearing Off
- Post-op Considerations r/t neuraxial anesthesia: Pruritis & hypothermia

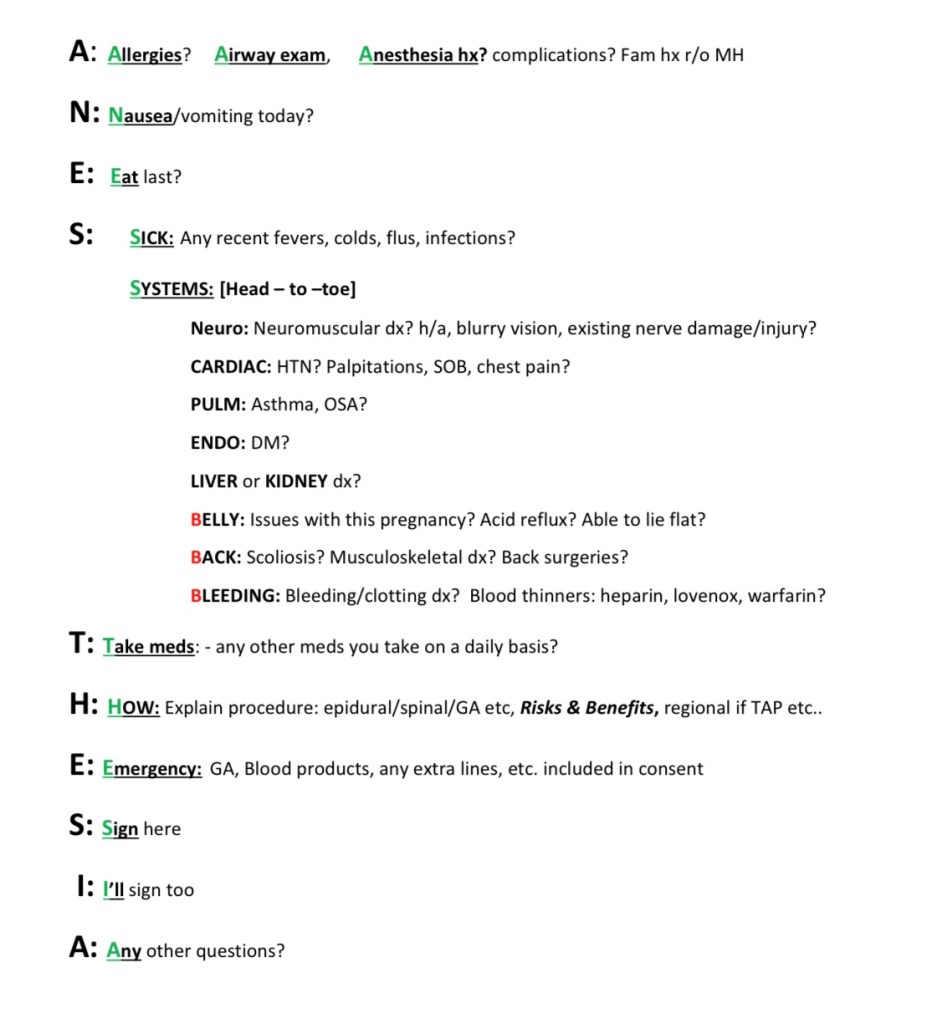
EFFICIENT PRE-OP METHOD
spell ANESTHE..SIA
A. AIRWAY, ALLERGIES, ANESTHESIA hx
- Airway: assessment
- Allergies
- Anesthesia hx: r/o MH – hyperthermia, cardiac events under GA – personal or family hx
N. NAUSEA/vomiting?
- Antiemetics needed? RSI needed? (Always RSI for OB but consider for non-OB pts)
E. EAT – NPO time
- Ideally 8hrs but in emergency we still just do neuraxial
- safer than GA w high-risk airway & full stomach
- Labor Epidurals
- clear liquids after placement, can technically eat up until point of placement per ASA, but labor floor has them on clears once they go into labor.
- Neuraxial for C/S
- Ideally wait 8hrs for fatty meal, 6hrs light meal.
- If mom is in labor & contracting, but full stomach, we still proceed to OR and perform spinal without waiting for NPO time.
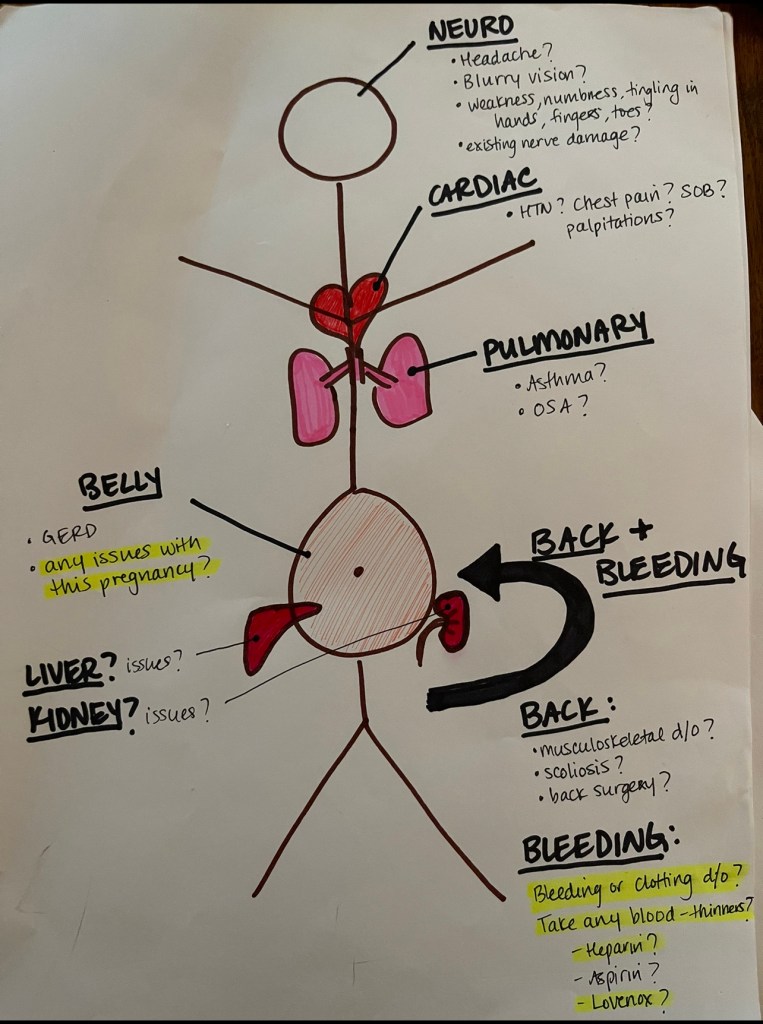
S. SICK & SYSTEMS
◦ SICK: Recent fevers flus colds infections?
◦ SYSTEMS: head-to-toe straight down
- Neuro:
- headaches, dizzy, blurry vision?
- weakness/numbness/tingling in hands/fingers/toes? existing nerve damage?
- Cardiac:
- HTN, chest pain, palpitations, SOB?
- Lungs:
- asthma, OSA?
- Endocrine?- DM?
- Liver or kidney problems?
- Belly:
- Any issues with this pregnancy? (PreE, GDM, etc)
- GERD? Previous abdominal surgeries?
- *BACK & BLEEDING:*
- Back:
- musculoskeletal dx? Scoliosis? Back surgery?
- Bleeding:
- Bleeding or clotting disorders?
- Blood thinners? Heparin? Aspirin? Lovenox?
- All aspirin doses OK for neuraxial
- Back:
T. TAKE MEDS:
- Any other meds you take on a daily basis aside from prenatal vitamins?
H. HOW:
- Anesthesia plan: Neuraxial Vs GA
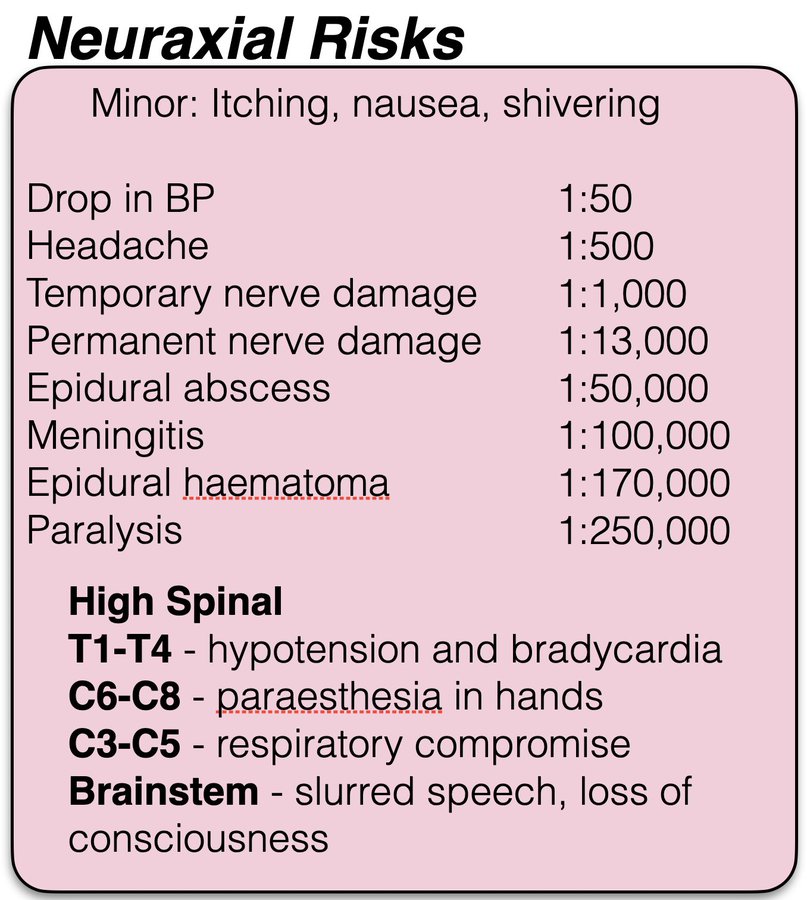
- Neuraxial Risks & Benefits
- Risk of bleeding minimal without bleeding disorder, just bruising
- Risk of infection – sterile procedure.
- Risk of headache:
- Epidural: 50-80% chance headache if wet tap
- Spinal: – 1/1000 headache risk from dural puncture.
E. EMERGENCIES:
- Consent for GA & BLOOD for all procedures in case of emergencies.
S. Sign here (patient)
I. I’ll sign too (provider)
A. Any other questions? All set.
Department Guidelines on Neuraxial: spinal/epidural and PLTs/labs:
Contraindications to Neuraxial (Spinal/Epidural)
(➡️GA if c/s needed)
Absolute Contraindications
- Pt refusal or inability to consent or cooperate
- Local infection at Neuraxial site – risks meningitis
- Systemic infection:
- pathogens can enter BBB – risks meningitis.
- BBB may be more permeable during pregnancy 2/2 VEGF and PLGF
- Eg) sepsis, PRIMARY (1st ever) HSV outbreak if untreated (1st exposure outbreak is systemic, subsequent outbreaks are localized and OK for neuraxial.
- pathogens can enter BBB – risks meningitis.
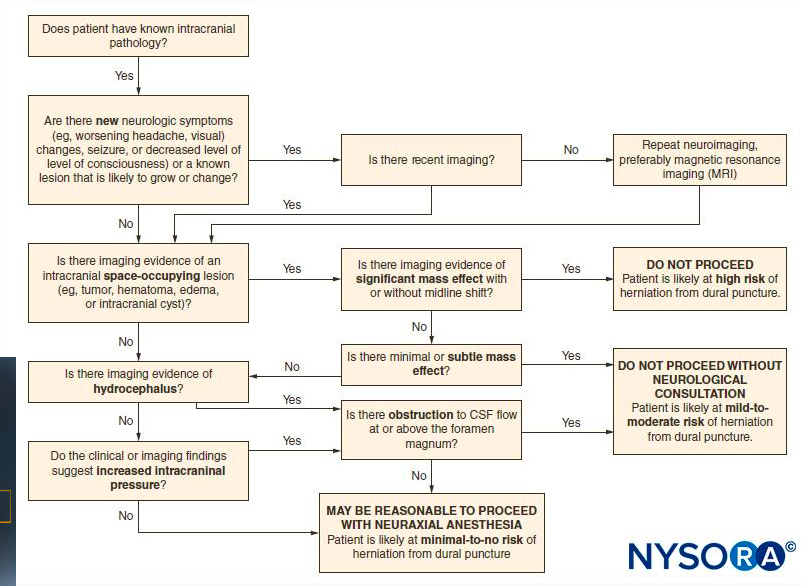
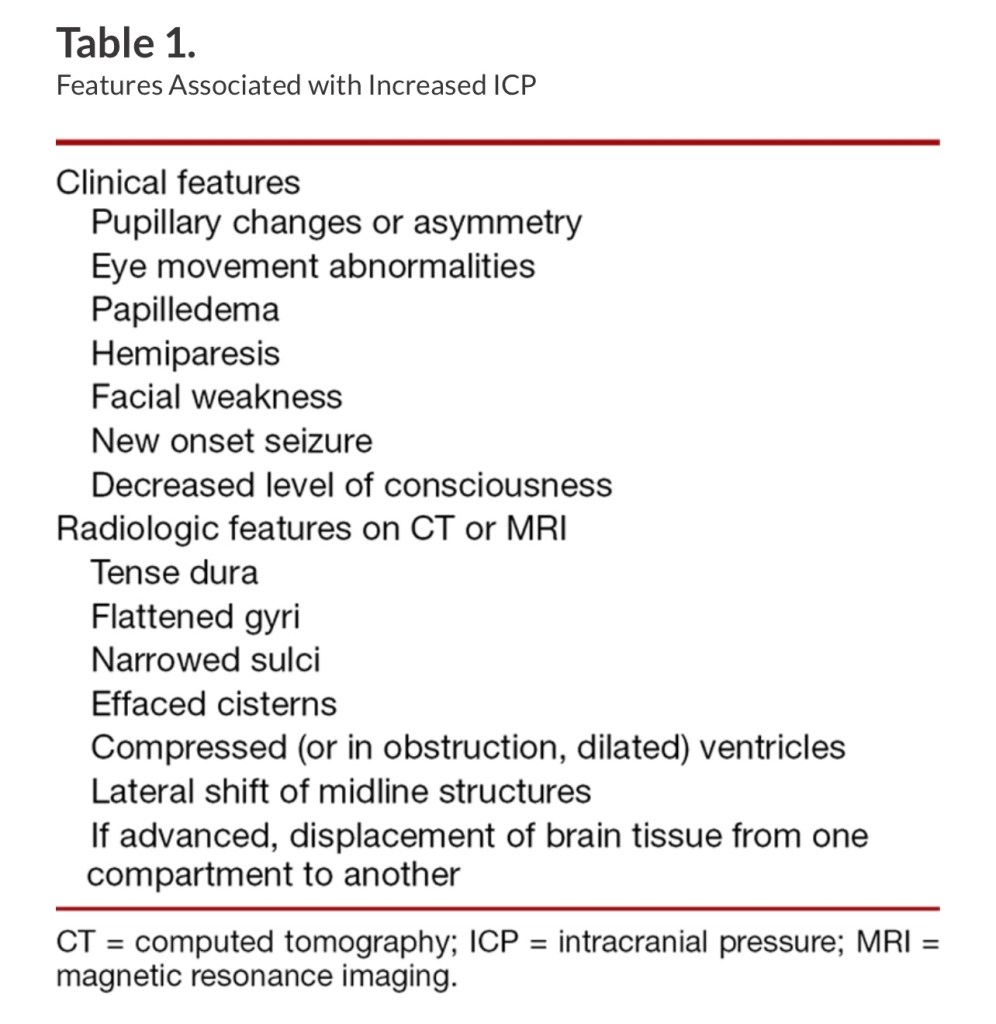
- Intracranial pathology: Increased ICP/exhibiting MASS EFFECT
- ^ICP and mass disrupting CSF flow
- needs Neuro consult
- Pseudotumor cerebri usually ok, as well as chairi malformation type 1, as long as they don’t have s/s ^^ICP (see NYSORA ICP & Neuraxial flowchart below)
Relative Contraindications
- Allergy to Local Anesthetic
- Active anticoagulant therapy
- Coagulopathies (PLT < 70k) or DIC, or clotting factor abnormalities/deficiencies (eg. liver disease) —> Coags (PT/PTT/INR,fibrinogen), CBC(PLTs), TEG may also be appropriate. (Heme consult for bleeding disorders)
- Aspirin ok for neuraxial, ibuprofen/toradol ok if taken postpartum before blood patch
- Fixed cardiac output state
- Severe Aortic stenosis, severe mitral stenosis, LVOT obstruction (HOCM)
- Spinal cord abnormalities:
- ex syringomyelia with chairi malformation, neurofibromatosis, spinal cord disorder prohibiting potential wet tap or spinal needle dural puncture (neuro consult)
- Profound hypovolemia or active maternal hemorrhage (which also could progress to DIC—>epidural hematoma)
- hypovolemia won’t tolerate sympathectomy.
- *Placental abruption*
- High risk of DIC if tissue factor in retroplacental clot enters maternal circulation.
- Once diagnosis of abruption is made or suspected, new coags &cbc should be drawn before neuraxial (spinal*) considered. Existing Epidural catheter can be dosed for section, but no new epidural should be placed.
- If coags & cbc normal, can maybe do single-shot spinal and plan to convert to GA if needed. Otherwise if no epidural in place and there’s no time to wait for new labs (for potential spinal) —> go straight to GA for c/s.
- Epidurals are higher bleeding risk than spinals due to large Tuohy needle AND catheter that can puncture an epidural vessel. (Small spinal needle has lower risk of vessel puncture – still both contraindicated in frank coagulopathy, but sometimes between a rock a hard place a spinal is safer bleeding-wise – ex: if pt has known difficult airway and GA is a worse option than neuraxial, you have to weigh risk v benefit & risk of airway compromise usually higher than risk of hematoma)
NYSORA ANTICOAGULATION guldelines for spinals/epidurals:
**ASRA COAGS APP is also amazing and what I always use*** ($7? purchase – please just buy it and use it – it’s invaluable)
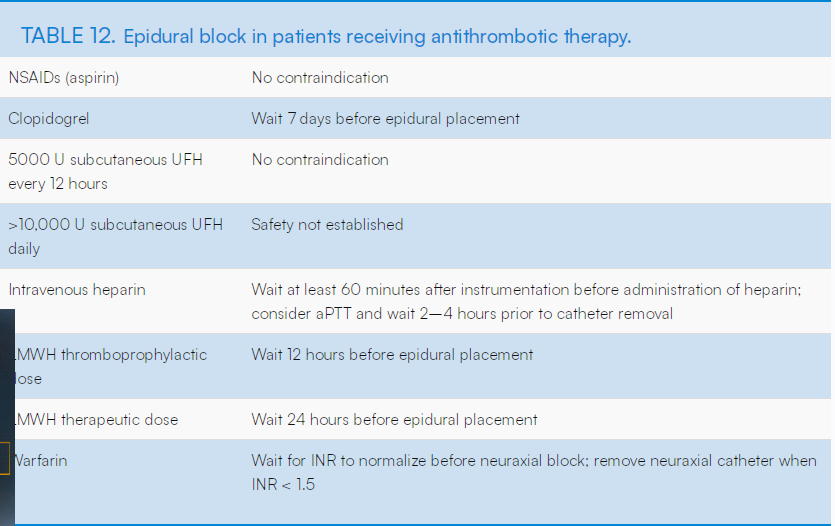
ASRA online Guidelines (but the app is better/easier to use):
NYSORA ICP & NEURAXIAL FLOWCHART:
HSV & Neuraxial
- Pts with untreated primary (1st ever) HSV usually not candidates for neuraxial 2/2 risk of seeding neuraxium. HSV does not usually breech CNS, but neuraxial can introduce HSV into CNS.
- Pts with reactivation, or treated HSV are OK for neuraxial bc no viremia present.
- TX: primary or recurrent infection during pregnancy: Acyclovir 400mg TID x 7-10 OR Valacyclovir 1000mg BID x 7-10D
- Pts with recurrent infections may be on prophylaxis.
- Neuraxial morphine increases risk for oral herpes labialis reactivation. Prevalence of HSV1 in women of childbearing age is 56-73%.
Ehler’s Danlos Syndrome & Joint Hypermobility
- Resistance to local anesthetics has been seen in Ehlers-Danlos syndrome and pts with joint hypermobility. This has been noticed especially in dental procedures.
- Many theories including: sodium channelopathy/mutation, increased CYP450 enzyme function, upregulation of nociceptive receptors creating a “wind-up” effect, and genetic differences in nociceptive receptor properties .
- Evaluate pt history of LA effectiveness, and discuss/manage expectations with labor epidural.
- Consider when placing spinal or dosing lido for c/s, their pathology may decrease length of spinal & pt may require GA or ketamine/versed to finish case.
- Esp if pt has a known history of LAs not working – Discuss with OBGYN that this c/s should ideally be as quick as possible as spinal anesthetic may wear off sooner and be less effective, and epidural top offs may also show decreased efficacy. Case may have a low threshold to convert to GA. (And position airway perfectly before starting the case** if she needs a little ramp, needs hair ties/accessories taken out to allow adequate neck extension etc…)
Resistance to local anaesthetics administered via epidural, intrathecal and pudendal injections
Ehlers-Danlos syndrome – British Dental Journal
Albinism & Hermansky-Pudlak Syndrome
- Albino trait is a characteristic of HPS, which is a syndrome including thrombocytopenia and qualitative platelet dysfunction (albinism, visual impairment, & bleeding diasthesis)
- Neuraxial contraindicated. They have normal PLT counts but the PLTs are completely dysfunctional.
- PLT transfusion and PLT function test/TEG can be considered for safety of neuraxial if GA is exceptionally dangerous for some reason – provider discretion.
- Adding insult to injury: HPS (10 subtypes) subtypes 1,2, & 4 likely to develop Pulmonary Fibrosis. Similar histology as idiopathic PF but manifests much earlier at age 30-40. No successful FDA -approved TX to prolong life aside from lung transplant. If Pulmonary fibrosis is present – TTE may be appropriate to assess for pulmonary HTN/RV strain prior to delivery…
Hermansky–Pudlak syndrome in a pregnant patient
Planning for Birth for a Patient With Hermansky-Pudlak Syndrome
Pulmonary Fibrosis in Hermansky-Pudlak Syndrome – PubMed
Seizure Hx
- Pts on seizure meds should have taken their seizure meds before surgery. If taking Keppra and haven’t taken dose today – can order IV dose from pharmacy and give prior to c/s. Call pharmacy if you need it quickly. Childbirth and surgery is a huge physiologic stress that could potentially trigger a seizure – this is not the say to skip a dose. No consistent data on ketamine affecting seizure threshold. If it’s needed for neuraxial wearing off, it should be fine especially since we always give benzo (versed 1st.)
Spine Surgery & Neuraxial
- Prior spine surgery/ hardware not a contraindication to neuraxial. It may make make neuraxial more difficult 2/2 scar tissue at the surgical level affecting tactile feedback, epidural space scar tissue affecting spread of block, and inability of the pt to position properly to gain access to epidural space, but it’s not a contraindication. CSE or dural puncture technique may be helpful to confirm placement and give more reliably even spinal block (labor CSE)
- Any pt with HARDWARE needs discussion in consent about hardware infection. Meticulous sterility is necessary
- *LUMBAR LAMINECTOMY removes the spinous process, and often a portion of the ligamentum flavum, making epidural placement inadvisable at that surgical level/levels d/t absence of normal ligaments and tactile feedback.
- Go a level or two above or below until you find an non-operative interspace between two spinous processes.
- LUMBAR FUSIONS with rods/hardware – (eg: scoliosis repairs) can make it technically difficult/impossible, but it’s always worth at least trying.
- Risk of hardware infection should be discussed in consent.
- SCOLIOSIS: The good news is scoliosis is often corrected at thoracic levels and the lumbar region is spared from hardware. Lumbar spine might still be a little malrotated and challenging, but usually do-able. Give generous local to these pts bc midline isn’t always a straight shot and you’ll get into muscle tissue on either side of the interspinous ligament- which hurts. With Epidurals, be patient and reassuring as you reposition Tuohy and navigate their sometimes skewed anatomy. These pts often request anesthesia consults, and this is a good time to highlight the benefits of asking for an epidural before they’re in excruciating pain – the anatomical challenges are only made worse by an inability to position themselves & hold relatively still.
ABOUT NEURAXIAL ANESTHESIA
NYSORA: SPINALS PAGE
Modern Neuraxial Anesthesia for Labor and Delivery

Helpful 3D Anatomy Spine Model
(more anatomy review in Labor epidural section)
Lumbar Spine – 3D model by walshlab
TYPES OF SURGICAL NEURAXIAL BLOCKS:
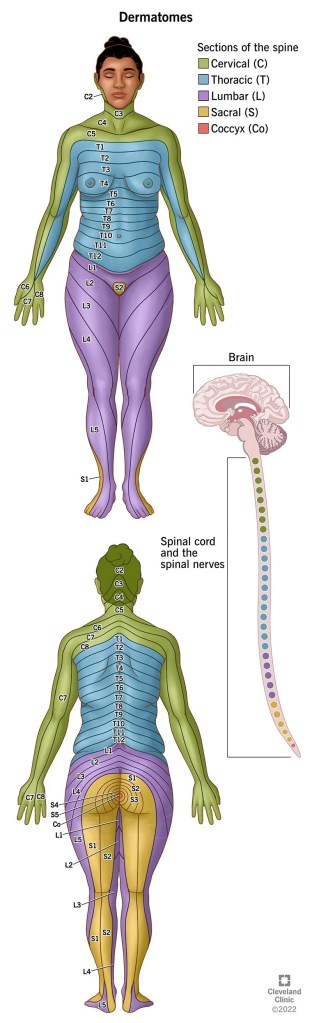
A T4 (nipple line) bock height (blocked cold sensation) is required to cover the C-fiber mediated visceral pain of peritoneal traction/manipulation during cesarean. This will cover the visceral pain of uterine/bladder/cavity manipulation and uterine exteriorization. Somatic pain (sharp, skin, deep tissue, muscle injury) carried on A-deltatype1&2 will be covered with a T10 block (uterine innervation, abdominal wall involved with surgery (up to T6 needed) & low transverse incision site would be covered.)
A-beta fibers, which also carry deep pressure and vibration, carry light touch (assessed by cotton swab/gauze) while A-delta and C-fibers carry noxious stimuli (pain & cold). Important to have COLD abolished at T4 – this will cover C-fiber mediated visceral pain, and loss of cold sensation (C-fibers) will be 2 dermatomes higher than loss of pinprick/sharp pain (A-deltatype1&2).
SPINAL for C/S
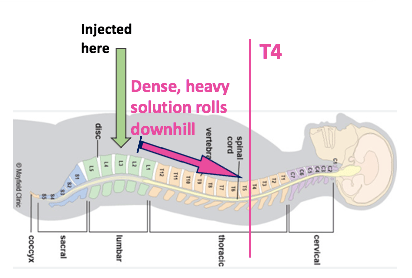
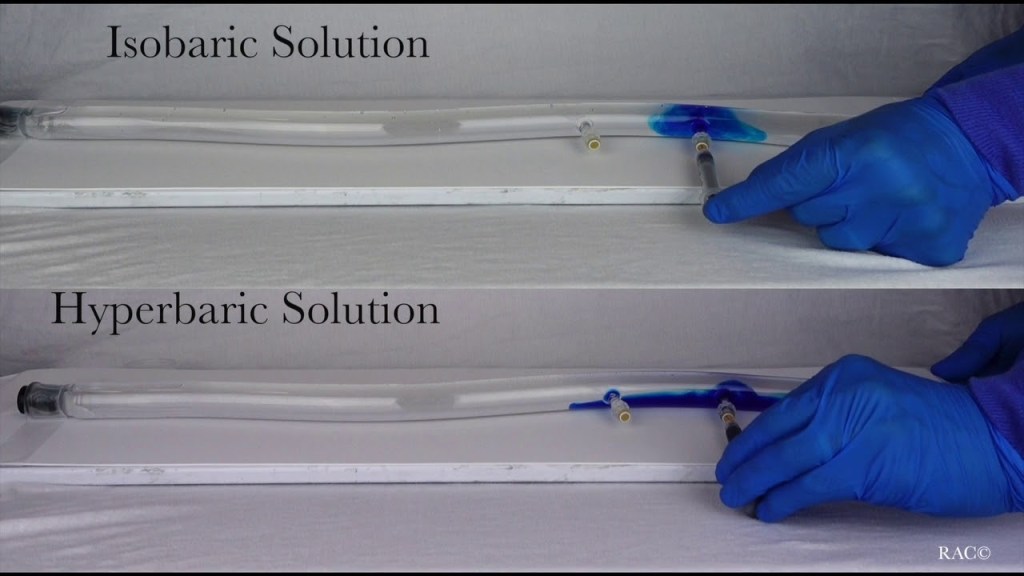
Single shot into CSF ~ 2hrs-2.5hrs block time (most C/S much shorter than this). When pt lies supine after spinal injection, the heavy, hyperbaric LA solution will flow “downhill” along thoracic curvature to T4 block height. Block height achieved by pt positioning and solution baricity relative to CSF.
- Pros: rapid, dense block. Reliable and evenly spreads through CSF.
- Cons: rapid, rapid sympathectomy—> Hemodynamic consequences, risk of high spinal.

REVIEW OF SPINAL ANESTHESIA MEDS/MECHANISMS OF ACTION & PHYSIOLOGIC RESPONSES:
Current Issues in Spinal Anesthesia
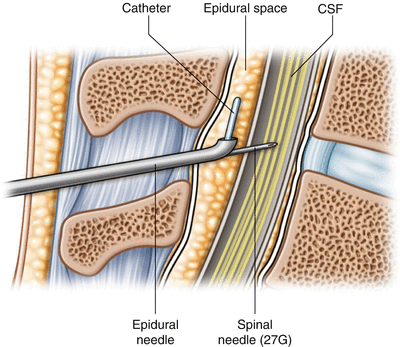
EPIDURAL for C/S
Large dose into epidural space to bathe bilateral spinal nerve roots as they exit the spinal cord through the epirudal space. Can re-dose for as long as needed to maintain surgical block. Labor epidurals can be dosed with high-volume, high-concentration LA to surgical-level block, or can be used for planned c/s in cardiac pts as they provide a slower, more gentle sympathectomy onset than spinals. The block density is based on concentration, and block height is based on VOLUME, not solution baricity (as a spinal).
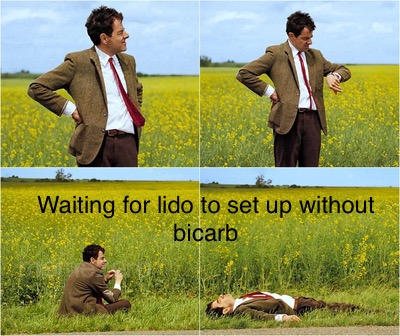
- Initial dose: 20cc 2% PF lidocaine with/without 1-2cc bicarb. Given in 5cc doses every 3-5 mins or so to pt response/T4 block to cold.
- If a slower-onset block/sympathectomy is needed to avoid rapid hemodynamic swings (HTN/PreE/cardiac pts) then don’t add bicarb.
- For normal pts, however, a faster block is fine, and adding bicarb allows it to set up in about 5 minutes. We use this a lot for stat c/s. Lido/bicarb or 3% 2-chloroprocaine, all 20cc, ~5cc at a time.
- Epidural Pros: more control over speed of sympathectomy. Safer for HTN/cardiac patients/pts who cannot tolerate large hemodynamic swings.
- Epidural Cons: Slower block set-up, can be one-sided and patchy (less common with these large volume doses) higher incidence of failing to provide adequate, reliable coverage than spinal.
CSE for C/S
A Combined Spinal-Epidural is performed like a normal epidural, but when epidural space is reached with LOR, a long, Tuohy-compatible spinal needle is placed through the Tuohy, a bit further, into the subarachnoid space to give spinal dose into the CSF (2 hr block). The Tuohy is left in place as the spinal needle is removed from the Tuohy, and an epidural catheter is threaded through the Tuohy into the epidural space. Now if surgery lasts longer than 2-2.5 hrs, we can dose the epidural catheter to maintain the surgical block level.
Pros: Benefits of reliable spinal dose, & ability to extend block time with epidural dosing. Great for longer surgeries (longer dissection time in morbid obesity, adhesions from prior c/s or abdominal surgeries, planned c-hysterectomy).
Cons: Skill-level required to thread catheter quickly before hyperbaric spinal dose settles sacrally (and wouldn’t reach needed T4 level). Cannot test epidural catheter (discussed further down) due to time crunch and confounding spinal sympathectomy-related factors. Epidural catheter can fail or be IV. We don’t have the time to change the catheter/re-thread before the spinal dose settles too sacrally, so now we just have a spinal.
- (*In LABOR CSE (a little different – small isobaric 2.5-3mg bupivicaine intrathecal dose – spinal dose can mask a poorly working epidural – which may be risky for certain labor pts – explained further in Labor Epidural & Analgesia page)
DOSING FOR SURGICAL NEURAXIAL BLOCKS
Dosing Spinals for Cesarean
- 1.6-2cc 0.75% bupivicaine = 7.5 mg/cc = 12-15mg
- 10 mcg intrathecal fent (0.01mg)
- 100 mcg (0.1mg) intrathecal PF Duramorph.
- ** in c/s CSE, we often just dose the full 2cc/15mg 0.75% bupivicaine – this is bc 1) the larger dose extends the block time some (the whole point of putting in a CSE), and 2) some of that hyperbaric dose will settle sacrally as they continue sitting upright while we thread the epidural catheter, so we expect to “lose a little” to the sacrum.
- * We don’t do an epidural test dose in c/s CSEs: 1) no time as that dose settles into the sacrum 2) sympathectomy s/s ^^HR can be confused with TD s/s…. Just place the spinal, thread the catheter, and we test the catheter IF we need to use it later in the case.
- OB c/s surgical spinals use 0.75% PF bupi. mixed w/ dextrose (makes it hyperbaric). Gives “dextrose swirl” w/ aspiration of CSF.
- After spinal placed, immediately lay pt supine so heavy hyperbaric solution flows downward along thoracic curvature to ~ T4. Otherwise, if pt remains seated, the hyperbaric solution will sink down to the lower lumbosacral nerve roots and not provide high abdominal coverage needed for cesarean.
- If 0.5% bupivicaine used at BJI for ortho spinals, it’s prepared with saline (makes it isobaric), no swirl will be present, only increased volume with CSF aspiration
Dosing Epidurals for Cesarean
[if existing, working epidural in place.]
- Risk of L.A.S.T if accidentally given IV through intravascular epidural catheter
- 18cc 2% PF lidocaine w/ 2cc Bicarb, and 1:200k epi (5mcg/cc) = 360mg lido, 90mcg epi
- or 20 cc PF 3% 2-Chloroprocaine, +/- bicarb
- + 100 mcg epidural fent for quick surgical block density (not post-op pain)
- After delivery: 3 mg epidural PF duramorph for post-op pain control. OSA pts require post-op SpO2 monitoring.
Give LA in 5-10 cc increments, and assess. Needs 5 min or so to set up.
- Lidocaine dose almost 400mg total = huge dose if given IV
- Max dose lido for blocks normally: 300mg, 450 if mixed with epi. (still not IV)
- Chloroprocaine’s RAPID PLASMA metabolism (<1min) places pt at significantly lower risk of LAST should the catheter have migrated IV.
- Short duration of action means it will have to be re-dose ~40 min, or can re-dose with lido/epi and bicarb, as re-dosing means the catheter worked for a while and wasn’t IV..
- Always aspirate every epidural catheter before bolusing. (for whatever it’s worth – you probably still won’t get blood back even if its intravascular, but would need to rely on the s/s of IV lido: metallic taste in mouth/ringing in ears. And tachycardia/HTN if lido mixed with epi.
-
- Epinephrine will extend the duration of the block, and decrease the risk of toxicity. ALSO if we give ~20cc of lido mixed with 1:200,000 epi (5mcg/cc) this is 90-100mcg epi!! NOBODY gets 100mcg epi IV and has no CV symptoms. SO while YES in these situations of an unplanned c/s, especially a STAT c/s, is reasonable for the pt to get anxious, and maybe have a high BP reading and some tachycardia from nerves – BUT BE SUSPICIOUS OF IV EPI (aka IV LIDO) IF you see significant tachycardia >140 combined with HTN in an otherwise non-hypertensive pt. This is why I prefer to dose the catheter in the OR on monitors if its not a STAT case – so I can keep an eye on signs of IV epi.. (and also monitor HOTN from this rapid sympathectomy that will decrease placental perfusion pressure in an already distressed fetus)… so IF its a true STAT and we’re running down to the OR and dosing her up in the hallway on the way, then chloroprocaine is a safer agent to use for its lower risk of LAST due to rapid plasma metabolism.
- But get a BP immediately on arrival to the OR! (I’d push 1cc or 2cc of phenylephrine as I’m dosing the epidural as well to mitigate this.. bc you’ve given her a huge sympathectomy (if the catheter is working and not IV) and potentially dropped placental perfusion pressure – which in an already stressed fetus (the resaon we do most STAT c/s) is just going to further compromise fetal oxygenation and increase acidosis..
- And finally, in weird situation where there ARE signs of IV epi, but ALSO the block is working well – I’d leave it alone. Just switch to Chloroprocaine. Maybe one orifice of the catheter is IV and the other two are in the epidural space. This means if she IS getting IV lido/epi, she’s only getting 1/3 of the dose IV.. and enough is still going into the epidural space to give her an adequate surgical block…Still beats risking airway manipulation in GA (and not ideal for a stressed fetus if we can reasonably avoid it). Use your judgement though.
- Epinephrine will extend the duration of the block, and decrease the risk of toxicity. ALSO if we give ~20cc of lido mixed with 1:200,000 epi (5mcg/cc) this is 90-100mcg epi!! NOBODY gets 100mcg epi IV and has no CV symptoms. SO while YES in these situations of an unplanned c/s, especially a STAT c/s, is reasonable for the pt to get anxious, and maybe have a high BP reading and some tachycardia from nerves – BUT BE SUSPICIOUS OF IV EPI (aka IV LIDO) IF you see significant tachycardia >140 combined with HTN in an otherwise non-hypertensive pt. This is why I prefer to dose the catheter in the OR on monitors if its not a STAT case – so I can keep an eye on signs of IV epi.. (and also monitor HOTN from this rapid sympathectomy that will decrease placental perfusion pressure in an already distressed fetus)… so IF its a true STAT and we’re running down to the OR and dosing her up in the hallway on the way, then chloroprocaine is a safer agent to use for its lower risk of LAST due to rapid plasma metabolism.
- Remember while spinal surgical block should have even coverage bilaterally, an epidural surgical block can have windows and different block heights/density bilaterally so b/l block assessment is important.
- If Emergency w/ decompensating fetus – use chloroprocaine (less fetal transfer/ ion trapping, and less risk of LAST in mom of epidural catheter is IV)
Current Issues in Spinal Anesthesia
Neuraxial med doses for spinals & epidurals:
LA options, Opioids, Adjuvants: dexmedetomidine, epi, clonidine:
Statement on Neuraxial Medication Shortage and Alternatives
Neuraxial Narcotics
- All pass to fetus but in higher ionized (inactive) fraction 2/2 normal fetal pH 7.25-7.45
- Exception is Remifentanyl: very minimal transfer 2/2 plasma esterase metabolism
FENTANYL
- Given to set up dense sensory block quickly, as lipophillic profile causes rapid diffusion across nerve fiber membranes. = Fast onset, short-acting. Not useful for longer-term post-op pain control (that’s what the neuraxial morphine is for).
- Can cause itchiness (central pruritis), but should only last a few hours.
- Also helps in labor epidurals with pressure sensations in transitioning stage of Labor (8-10cm) (50-100mcg epidural). (Thick A-beta fibers carrying pressure sensations harder to knock out with LA alone in labor analgesia doses)
- Minimal fetal transfer when given in epidural space, and fent has short duration of action.
- Has some systemic uptake and placental transfer, but proven safe for fetus/newborn: APGAR scores seem to be unaffected. No active metabolites
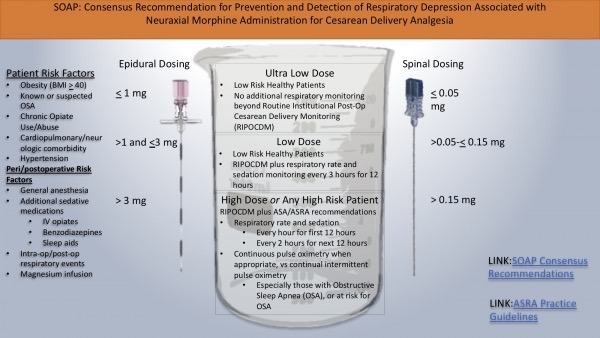
DURAMORPH (Preservative-free Morphine)
- (MORPHINE) has biphasic response with intrathecal administration:
- Must be PRESERVATIVE -FREE if given neuraxially
- Intrathecal dose peaks at 2h, AND 6-12hrs – so only used for post-op pain. Provides 12-24 hours additional pain control due to hydrophillic nature – stays in CSF longer. Can cause longer-lasting itchiness (central pruritis – addressed further down in post-op considerations)
- NOT useful for intra-op pain control – takes too long to take effect (that’s what the neuraxial fentanyl is for)
- Biphasic response = concern for LATE respiratory depression as Morphine drug effect peaks again ~ 6-12 hrs after intrathecal administration.
- In epidural doses, there is some diffusion into intrathecal space, as well as systemic IV uptake in epidural vasculature. IV Morphine duration of action is 2-4h, but the biphasic response is specific to fraction of drug that has passed into intrathecal space and is circulating around brainstem/CNS
- (periaqueductal-periventricular gray matter, ventromedial medulla, & spinal cord. Most Mu binding sites in posterior amygdala, hypothalamus, thalamus, caudate nucleus, putamen, some cortical areas, & in spinal cord on terminal axons of 1o afferents in substantia gelatinosa)
- In epidural doses, there is some diffusion into intrathecal space, as well as systemic IV uptake in epidural vasculature. IV Morphine duration of action is 2-4h, but the biphasic response is specific to fraction of drug that has passed into intrathecal space and is circulating around brainstem/CNS
- Biphasic response = concern for LATE respiratory depression as Morphine drug effect peaks again ~ 6-12 hrs after intrathecal administration.
- Duramorph can pass to fetus as both med and active metabolite (morphine-3 glucuronide & Morphine 6-glucuronide) – can cause bradycardia and prolonged or delayed resp depression in neonate, poor feeding, etc
- Minimal fetal transfer when administered intrathecally with spinal, but epidural for c/s dose delayed until fetus is delivered (for best possible outcomes)
- Duramorph in patients with OSA requires post-op SpO2, and Q1h monitoring x 12h, Q2h monitoring x 12h d/t risk of delayed respiratory depression.
Intrathecal Morphine – StatPearls – NCBI Bookshelf
Morphine (AVINza, Duramorph) | Davis’s Drug Guide
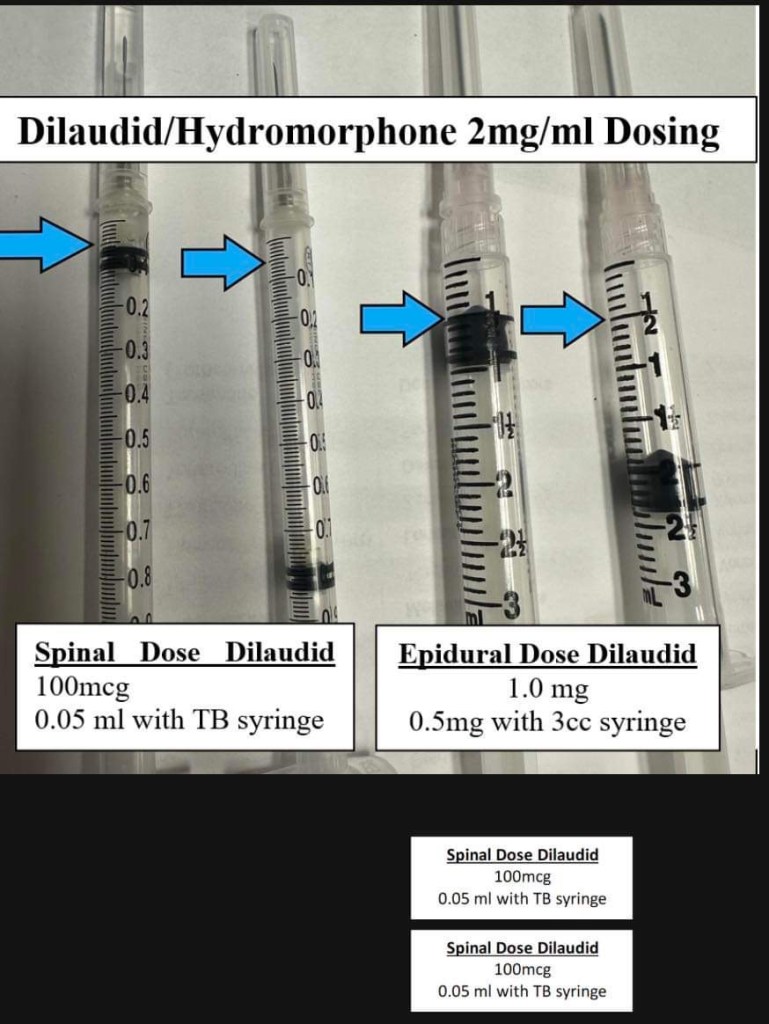
HYDROMORPHONE (DILAUDID)
- We’ve had some duramorph shortages and used Hydromorphone for spinals and epidurals:
- Doses: (1st syringe is the correct dose, 2nd syringe is a better look at the marking on the syringe without the black rubber in the way. This is from a 2mg/mL vial of dilaudid.)
pKa
- pKa = 50/50 amount ionized v non-ionized form
- non-ionized is active med
- pKa ~ speed of onset (lower PKA = faster onset at physiologic pH)
- All local anesthetics, including 2-chloroprocaine, are weak bases:
- weak base = pKa > 7.0
- all LAs have pKa > 7.4 (physiologic pH)
- Lower pKa is assc w/ a greater % of nonionized (active) drugs at physiologic pH, which gives a faster onset of action.
- pKa 3% 2-Chloroprocaine 8.7, pH of mom 7.4. = higher ionized (inactive) fraction at physiologic pH than lido (pKa 7.8), however the high 3% concentration is responsible for rapid onset 2/2 high concentration/diffusion gradient.
- 3% 2-Chloroprocaine technically sets up fastest [difference may be trivial in clinical reality- lido/bicarb seems to set up just as fast]
- 3% 2-Chloroprocaine lasts ~ 45 min, may need re-dose ~10 cc.
- 2-Chloroprocaine is an ester-linked LA metabolized by plasma esterases – less fetal transfer. Rapid plasma metabolism in both mom & fetus. Et1/2 <1 min
- Chloroprocaine still can be arguably used with severe fetal distress since theoretically less fetal transfer 2/2 rapid plasma cholinesterase metabolism. Distressed acidotic fetus = more ion trapping with amides/lido AND acidosis causes right shift of fetal hgb dissociation curve = less oxygenation.
- 3% 2-Chloroprocaine is for EPIDURALS. There is a spinal formulary of 2-Chloroprocaine but it’s 1% PF, and not often used.
Adding Bicarb to Lidocaine
- Mixed 18cc 2% lido with 2cc bicarb. {pKa lidocaine = 7.8}, bicarb increases pH for a higher % non-ionized fraction, and rapid onset.
- Lidocaine PLAIN takes about 10+ minutes to fully set up in epidural space, but lido w/ bicarb* sets up in minutes, in reality it’s not much slower than 3% 2-chloroprocaine.
- Bicarb only used with lido – not mixed with bupivicaine to buffer/speed onset of bupivicaine, as it will cause precipitation (not that we use bupi for epidural c/s anyway – we use lido or chloroprocaine bc bupi takes too long to set up) And onset speed of 3% 2-chloroprocaine is due to concentration gradient, not pKa.
^Lipid soubility = ^ potency
^ Protein binding = ^ duration of action
pKa = onset of action: lower pKa = faster onset at physiologic pH

Comparison of Chloroprocaine Versus Lidocaine With… : Anesthesia & Analgesia
Chloroprocaine – StatPearls – NCBI Bookshelf
Physiology, Fetal Hemoglobin – StatPearls – NCBI Bookshelf
Table 1. Physiochemical properties of all Local Anesthetics
https://www.bjaed.org/action/showFullTableHTML?isHtml=true&tableId=tbl1&pii=S2058-5349%2819%2930
EPIDURAL vs SPINAL:
CARDIAC PT CONSIDERATIONS
For cardiac patients, uncontrolled HTN patients, pulm HTN – planned epidural better option than spinal. Make sure epidural is working prior to c/s, it provides more gentle onset to sympathectomy w/ slower, more controlled dosing. Lessens initial BP drop by allowing more time for cardiac compensation/treatment.
• Esp for heavily beta-blocked pts w/ preE/gHTN, the baroreceptor reflex of ↑ HR may be blocked leading to more profound HOTN after spinal sympathectomy (*↓ placental perfusion) (*esp preE -intravascularly dry)
• ALSO for pts w HTN going for urgent/stat c/s for decels** with epidural in place – May be better to dose in OR w/ monitors on, or at least close to OR. Want to keep moms BP at baseline so BP drop doesn’t decrease placental perfusion and cause huge decel. If you start dosing in labor room/hallway you have no FHR or maternal monitor in place to see effects of dose. Esp in HTN pts (PreE) – keep BP at baseline to keep MAP-dependent placental perfusion at baseline. These pts are also intravascularly dry and a sympathectomy can cause exaggerated HOTN from a relative hypovolemia. In an already distressed fetus this can cause further acidemia/hypoxemia.
• Lido/bicarb or chloroprocaine/bicarb works so fast, dosing in/near the room on monitors is usually still fine, esp w these more fragile patients – but start dose immediately on arrival to OR.
- 10cc initial dose. Allow a few mins to reach desired effect. Test skin to sharp and cold touch. If more needed, dose rest in 5cc increments, testing after each.
Neuraxial Placement Tips
How to scrub the back:
- FIRST, when scrubbing back, scrub well over planned insertion point, staying away from the butt cheeks please.
- SECOND scrub out in concentric circles, never crossing back over the center point where you will insert the needle. Don’t make the area so huge that you’re scrubbing between butt cheeks and then dragging all those germs up and around and over your neuraxial site, please and thank you.



- Orient to L4 interspace with hip crests/tuffiers line. You may still be a level higher than you think, so always feel out the level below especially in shorter and heavier patients. L4-L5 might be your widest interspace.
- Positioning is EVERYTHING. Remind pt throughout procedure to push out their back against your finger/hand (flexion). They’ll subconsciously pull away the whole time and extend/arch their back. Esp after you numb them bc that lido really burns. Once they’re numb, reposition them again.
- PDPH can happen from spinals too! Especially if you accidentally poke through dura (possibly multiple times) with the long local “finder” needle without realizing… (larger bore cutting needle)
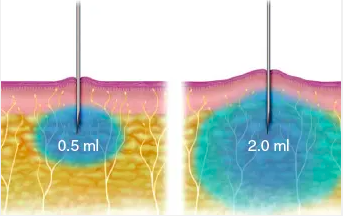
MAKING LOCAL INJECTION LESS PAINFUL:
Go straight in, through dermis and inject into Sub Q. Do not insert at an angle – you’re only cutting across more nerve endings.
- Nerves in the dermis are like trees with sensitive leaves, and in the fat are like branches and trunks. Injections in the dermis hurt more than in subcutaneous fat, because you irritate more “leaves” with the pressure of intradermal injection. Inject just under the dermis instead of in the dermis.
- Inserting the needle perpendicular (90 degrees) to the skin hurts less than if you come in parallel to it, because you pierce fewer nerve endings with the sharp needle tip on the way to the subcutaneous fat.

- As soon as the needle is inserted, blow in a visible bleb of 0.5 ml under the dermis (in SubQ fat), not in the dermis. The needle should be inserted at 90 degrees so that fewer nerves are pierced. At a 90-degree angle, the patient will feel less pain than if the needle is inserted at a 45-degree angle. (From Strazar AR, Leynes PG, Lalonde DH. Minimizing the pain of local anesthesia injection. Plast Reconstr Surg 132:675, 2013.)
- After you have injected 0.5 ml in the subcutaneous fat, hold still at least 15 seconds. Ask the patient to tell you when the sting of the needle is all gone. The first subcutaneous bleb or wheal must be visible or palpable under the skin in order for the needle insertion site to be properly numbed. After the patient tells you the sting of the needle is gone, inject an additional 1.5 ml very slowly without moving the needle. (From Strazar AR, Leynes PG, Lalonde DH. Minimizing the pain of local anesthesia injection. Plast Reconstr Surg 132:675, 2013.)
- Source: https://musculoskeletalkey.com/chapter-5-how-to-inject-local-anesthetic-with-minimal-pain/
REDIRECTING NEEDLES:
- When hitting os or vessels (or pt complaining of sharpness on one side) with the introducer or spinal needle, you’ll need to redirect…If hitting os with spinal needle: REMOVE THE SPINAL NEEDLE before redirecting.
- That spinal needle is SO flimsy you will never be able to re-direct from the skin – it’ll just bend around in the tissue. You need to re-direct the introducer and re-insert it in a straighter path, then re-insert the spinal needle.
- The first thing I do to check my angle is let go of the introducer completely and see if it’s leaning in one direction or another. It won’t fall out. I also re-assess the pt position. We can get tunnel vision working in this little sterile window and the pt can meanwhile be leaning forward, arching their backs, leaning sideways, etc etc making the procedure more challenging. So I first see if the needle obviously is slanted, and then I reposition my pt and go around to the side of the bed and check her positioning from there to make sure she’s not eating forward.
- When you re-direct your needle it’s kind of like correcting a parking space. It’s already engaged in a lot of connective tissue that doesn’t have a lot of elasticity or wiggle room, so it’s not as easy as just changing the angle from the skin. You can wiggle the portion outside the pt around but you’re really just bending the needle (and some of those introducer needles are SO flimsy) but the tip won’t move – instead you need to pull back to SSL and re-insert/re-engage in a straighter path. It’s like when you’re parked between two cars and have to correct – you can’t do much inside the space – you have to pull back out and reposition your car straighter, and pull straight in.
*If having a lot of difficulty with spinal, can also try using CSE kit to find epidural space first with pulsator LOR syringe (what we have available in OR without opening entire epidural kit).
- Sometimes in obese pts the Tuohy acts like a longer introducer for the spinal needle. Its tissue feedback will give you a better idea of where you are as you go through ligament layers.
- When you get LOR, all you have to do is put the CSE-compatible long spinal needle through to intrathecal space.
- *USUALLY have to hub CSE spinal needle in Tuohy. The spinal needle only comes out 2cm or so past the end of the Tuohy, and you want to ensure you’re actually intrathecal and not injecting the spinal dose into the epidural space (which won’t have any effect).
- If using saline for LOR, 10mL flushes & vials are in pixis (ask someone to squirt it sterile into a well in your kit. Don’t dilate the space with saline before giving spinal dose – want to make sure fluid coming back through spinal needle is CSF and not saline from the epidural space. Can absolutely use saline for LOR, just don’t push the rest of it in yet after your LOR. Then use CSE spinal needle from kit to confirm CSF and deliver spinal dose through Tuohy. No need to thread an epidural catheter unless you want an actual CSE. BUT with such a difficult placement, might as well just thread a CSE catheter as a safety net.
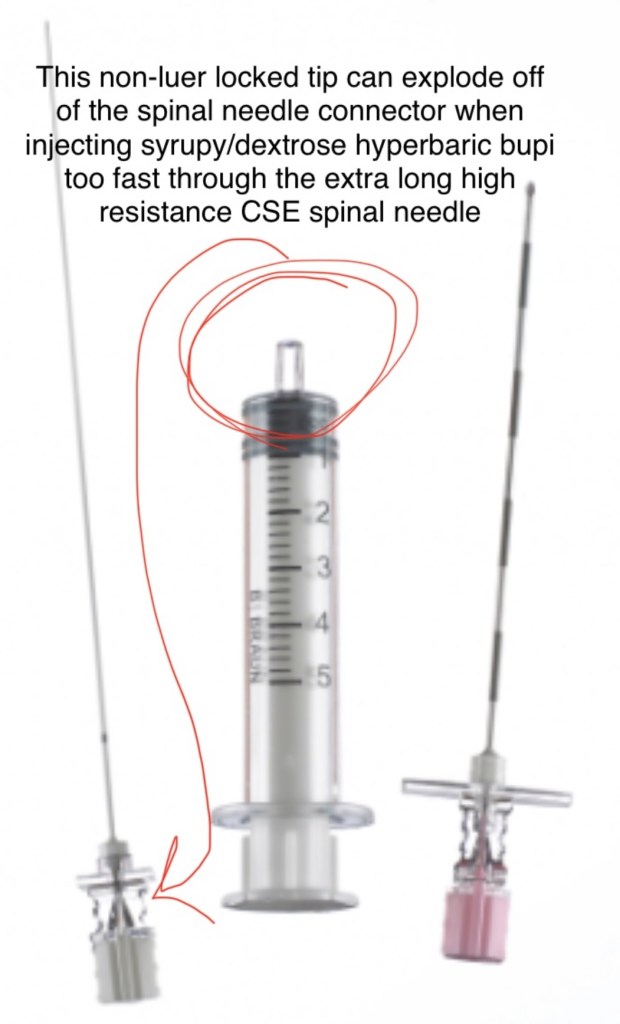
The CSE kits have compatible Tuohy and Spinal needles – you have to use both together and NOT mix and match. The CSE kits are not interchangeable, you must use that specific Tuohy with that specific spinal needle to guarantee they fit each other.
- This ensures the spinal needle:
- 1) fits through that gauge Tuohy
- 2) is long enough to come out past the end to reach the intrathecal space. The regular spinal kit needles are not long enough to reach the end of a Tuohy needle. You need the CSE kit extra-long spinal needle.
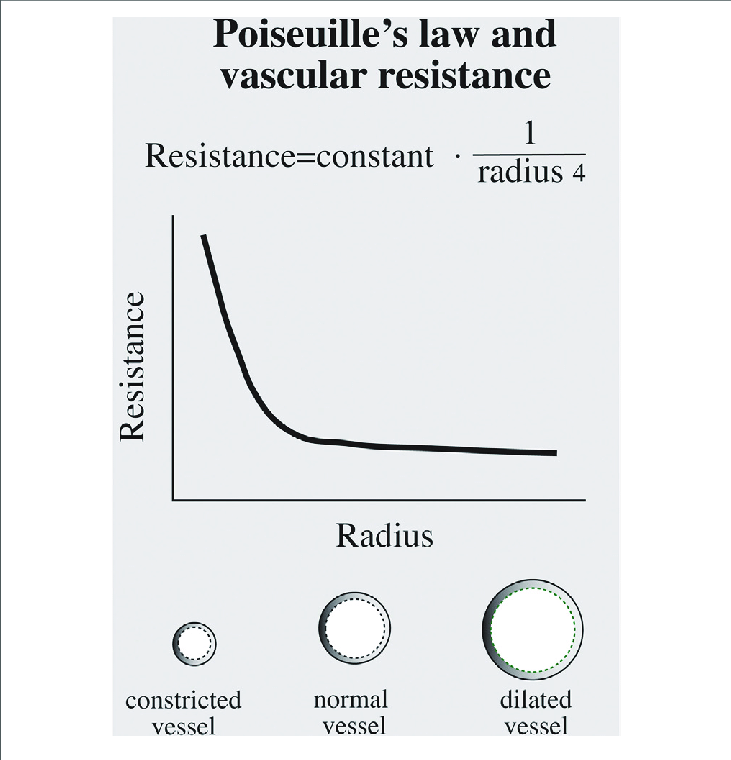
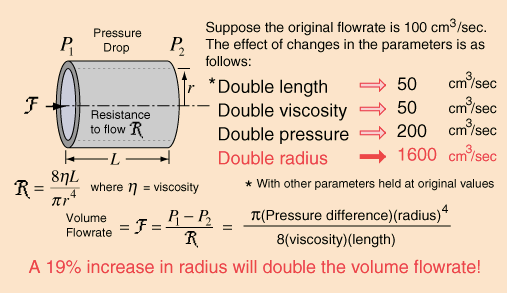
- Since CSE spinal needles are longer, they’re HIGHER RESISTANCE (Poiselle’s Law) so inject spinal dose more slowly and carefully. Especially that hyperbaric spinal bupi- the dextrose makes it syrupy and it’s very high resistance to push it through that long CSE needle – especially if you don’t have a leur lock spinal syringe. (Many CSE kits and spinal kits include a glass spinal syringe that has no leur lock – this syringe connection can explode apart off of the spinal needle when the spinal dose is injected from the high pressure, leaving your pt with no spinal dose – it has happened to ALL of us – but it makes us look like bumbling idiots and we have to re-draw up another spinal dose and it’s a whole thing – so a work-around is just dropping a 5cc luer lock syringe onto your sterile field and drawing up the spinal dose with that syringe instead.)
- At our institution, keep the peace and don’t draw up the spinal dose with the 3cc syringe instead – I know that’s the obvious answer but it just confuses everyone bc we always use that 3cc syringe for plain lido local and that’s just the established culture we have to roll with – we have too many new learners and people coming in and out that we just stick to one way of drawing things up so if anyone has to take over the procedure at any point, at any hour of the night – everything is standardized: Local in 3cc syringe, Spinal dose in 5cc syringe.
- Can drop a sterile 5cc luer lock into your field instead if you want to use that for the spinal dose and minimize spinal syringe confusion.
- At our institution, keep the peace and don’t draw up the spinal dose with the 3cc syringe instead – I know that’s the obvious answer but it just confuses everyone bc we always use that 3cc syringe for plain lido local and that’s just the established culture we have to roll with – we have too many new learners and people coming in and out that we just stick to one way of drawing things up so if anyone has to take over the procedure at any point, at any hour of the night – everything is standardized: Local in 3cc syringe, Spinal dose in 5cc syringe.
- Braun makes these stupid cursed syringes:
HOW TO MANAGE CESAREAN SECTIONS
———————————————————————
SET-UP for C-SECTION:
————————————————————————
Room setup
Monitors:
- 3-5 lead ekg
- NIBP
- SpO2
- Skin temp probe
Equipment for every single case:
- Working, HISSING suction
- Airway supplies:
- (towel bundle: prepared 6.0 & 7.0 standard ETT & glidescope ETTs, OPAs, MAC&Miller 3&4, OGT)
- LMA 3,4,5 & bougie in room (LMA still part of difficult airway algorithm in pregnancy)
- Bair hugger blanket
- Tape
- Alcohol pads (to assess block height)
Meds:
- Pre-op reglan, bicitra, H2 blocker given by RNs
- Spiked pitocin gtt [start as soon as baby delivered – program 10 unit rapid bolus dose over 10 min (999mL/hr)]
- Fent & duramorph spinal or epidural doses
- 8 mg zofran (give before neuraxial)
- 4 mg decadron (give after neuraxial- perineal burning?)
- Phenylephrine sticks (give 1 cc immediately after spinal placed to minimize HOTN)
- Ephedrine sticks
- Glyco – 2nd line n/v
- Ketorolac 15-30mg (at end of case)
- Antibiotics: Ancef always +/- azithromycin if ROM (azithro brought in by RN if membranes ruptured)
Emergency meds available:
- epi
- atropine ~1mg
- propofol
- succinylcholine
- ketorolac
- TXA
- pressor bags in pyxis
- Additional Uterotonics brought to OR by RNs
Available Emergency Equipment:
- Large bore IV setup, blood tubing, fluid warmer and tubing, A-line supplies & kit.
*AIRWAY EXAM *
- *Optimize every airway prior to surgical incision – ramp appropriate pts for all c/s even if GA not planned. Emergencies are usually not planned, and OB has high rates of difficult airways, PRepare every case for the worst case scenario.
- – Can use OR blankets/towels in warmer to improve airway position.
- Pregnancy causes mucosal capillary engorgement –> swollen airway
- PUSHING can increase airway swelling dramatically
- (esp if c/s after mom has been pushing, or if taking mom back to OR for retained placenta after vaginal delivery.)
- PreE, HELLP, and redundant airway tissue of obesity can increase airway swelling dramatically.
- PUSHING can increase airway swelling dramatically
- Pregnancy causes mucosal capillary engorgement –> swollen airway
- EVERYONE will ALWAYS help you ramp pt/ adjust ramp when they lie down after neuraxial placed, or after moving pt over from floor bed when coming in for an urgent/emergent/stat section. AIRWAY TRUMPS ALL. These are high risk of swollen, difficult airways on a full stomach with low FRC. Respect the airway.
- Ask every pt when they lie down to briefly raise their chin to the ceiling to assess adequate neck extension.
- If neuraxial fails or pt needs ETT for any reason, it’s more difficult to adjust pt position once drapes are up and surgery is underway. By then, half the room is donning sterile gloves. ALSO if intubation and ventilation fails – we need emergent neck access for cricothyrotomy… make sure you can see EVERY patient’s neck before the case starts.
- With that being said, if pt needs intubation and requires adjustment, there’s still enough staff in the OR to help you position pt behind the drapes and help you ramp/adjust, but this wastes a lot of time in a failed airway situation – these pts desaturate IMMEDIATELY.
- If neuraxial fails or pt needs ETT for any reason, it’s more difficult to adjust pt position once drapes are up and surgery is underway. By then, half the room is donning sterile gloves. ALSO if intubation and ventilation fails – we need emergent neck access for cricothyrotomy… make sure you can see EVERY patient’s neck before the case starts.
- Women with lots of thick hair/thick braids need to ensure they can put their head flat on the pillow and extend their neck. Large buns/braids/etc need special attention to position neck/airway and allow good neck extension. Hair ties/clips can come out prior to start of case. Part hair down middle if necessary to allow head to rest flat on pillow. Shoulder rolls can help.
- There are stories of failed airways due to thick hair impairing normal neck extension to obtain view for intubation. Add OB respiratory physiology and this could be fatal. This cannot happen.
Special Airway & Respiratory Considerations
- Pts can have increased airway swelling and engorged, friable tissues requiring smaller ETT and careful intubation (7.0 or 6.0). Especially *after pushing* airway edema can worsen, & preE/HELLP increase swelling even more.
- *NO nasal airways or NGTube- nothing nasal- nose off limits
- friable tissues —> epistaxis, bloody airway.
- Their DEcreased FRC and INcreased MRO2 leads to RAPID desaturation. Add OSA & obesity = even more precipitous desat. You need the best airway position possible BEFORE an emergency arises, as you do not have the usual amount of time to manage this, and full stomach increases risk of aspiration w/ mask ventilation.
- Have glidescope in OR for appropriate patients at START of case.
- Make sure you have ALL emergency supplies: pitocin, prop, succs, epi, at least 2 vials atropine (~1mg total), phenylephrine, ephedrine, 2 Zofran vials, and ketorolac available in room prior to start of case.
- High spinal or benzold-jarisch reflex would be evident at start of case – epi/atropine should be available in room before spinal administered.
- LOC = intubate without induction meds – they are unconscious. Minimize masking d/t full stomach, use cricoid pressure & OPA for masking to reduce liklehood of gastric insufflation.
Case Highlight Reel for C/S under Neuraxial Anesthesia :
- Nausea/vomiting unfortunately common in c/s – turn mom’s head to the side, give her the emesis basin, and suction her mouth/basin. Clean her off as much as possible/ place clean towel over any emesis on sheets. Treat BP, give glyco if normotensive.
- Do not fluid overload her. < 1L IVF appropriate for C/S.
- Normal blood loss 300-500cc vaginal delivery, 800-1L for a C/S.
—————————
1. Baseline vitals: SpO2 & NIBP Q 1min cycle until delivery.
2. Give 6-8mg ondansetron prior to spinal (can test if IV is working well with this*) [Ondansetron 6-8mg shown to reduce HOTN from spinal, and pruritis from intrathecal opioids]
3. Place Spinal after OBGYN listens to FHR.
4. Lay pt down and administer 1cc phenylephrine to mitigate oncoming sympathectomy.
5. Assess pt airway position & capacity for neck extension – appropriate ramp if needed.
6. Apply EKG pads, bair hugger blanket, and temp probe.
7. Q 1 min NIBP – treat with phenylephrine/ephedrine. Maintain tight BP to baseline until fetus delivered.
8. Administer antibiotics (slowly – they cause nausea w rapid admin)
9. Test block height w alcohol pads/tongue depressor
10. Reassure pt block is working, but she’ll still know people are touching her & feel pressure/tugging/movement – perfectly normal.
11. Manage nausea: HOTN is #1 cause: neo/ephedrine (8mg zofran total) Then can move to glyco if still nauseous despite normal BP.
12. Drapes go up. Allow mom to move arms behind drapes if she wants to touch/itch her face.
13. TIME OUT:
- ASA
- Allergies
- Antibiotics given
- Anesthesia type (spinal w fent & duramorph)
- Pitocin gtt ready
- Bair hugger in place.
- If not already mentioned: pt contraindications to uterotonics:
- No Methergine in: HTN (cHTN, PreE, HELLP, gHTN, SIPE) cardiomyopathy, pulm HTN
- No Hemabate in: Asthma, pulm HTN, cardiomyopathy
14. Skin incision
15. Pt support person/partner comes in after incision. They must remain seated and can take photos behind drapes, but no video while in OR.
16. Drowsiness common after spinal esp w intrathecal narcotics – reassure her this is normal.
17. Uterine incision – warn mom intense pressure/cramping expected – short lived.
18. Delivery of baby – start pitocin bolus as soon as baby delivered – see below for studies about delayed cord clamping and pitocin admin.
19. Placenta delivery (risk of hemorrhage, rare VAE if uterus higher than heart, AFE) don’t get distracted by baby – watch mom.
20. WATCH MOM HERE: titrate off pressor gtt (if running) to assess bleeding and not mask hypovolemia (pitocin bolus can also cause transient SVR dip – can ask about uterine TONE (code for bleeding). AUTOTRANSFUSION OCCURING: ~ 700cc are rushing back to heart from continuously contracting uterus. Fragile cardiac pts can go into heart failure. PFO pts can R-> L shunt (Eisemengers) from high RV pressure. Pulm edema if diastolic dysfunction (HTN/PreE)…etc etc etc.
21. Normal for CS babies to need suctioning in the crib/warmer after delivery. Fluid in little lungs isn’t squeezed out in birth canal like in a vaginal delivery. Reassure mom as baby is being suctioned/assessed that this is common.
22. Manage mom bleeding/hemodynamics – can move to Q3min NIBP if stable.
23. Nausea common here as uterus is EXTERIORIZED (pulled up and out of abdomen) for better visualization to suture it closed. – Visceral tugging can also cause shoulder pain in mom. [can give glyco 0.2mg, haldol 0.5-1mg, and/or 1-2mg versed as additional anti-emetics]
24. Document in a quick note: any 2nd line uterotonics the RN/surgeon gives (Intrauterine pit, IM methergine, IM hemabate), or if we give TXA..
25. Shivering/shaking is normal after delivery – result of hormone shifts and catecholamines. Usually lasts about an hour and is not related to hypothermia. [If profound hypothermia IS noted, esp in bleeding pt – 0.5mg IV ativan, or just 1-2mg versed will reverse hypothermia caused by intrathecal morphine* – discussed at bottom of page in post-op section]
26. Skin-to-skin: adjust EKG pads, help facilitate RNs placing baby on mom’s chest, let her move her arms out from under bair hugger straps.
27. Closing: Ketorolac 15-30 mg IV – always check with surgeon – 99% of the time they want it, unless oozing/bleeding concern. (Ketorolac shown to have ceiling effect at 15mg for analgesia)
28. Chart UO. (OB team adds QBL to chart, not us. EBL not used since blood in suction mixed w amniotic fluid)
29. Moving to PACU bed: pit gtt and IVF come with us, off pump, just disconnect and clamp tubing. Plug in bed in PACU and get a set of vitals. Pitocin re-started in PACU.
30. Hand off RN report.
Ondansetron Is Effective to Treat Spinal or Epidural Morphine-induced Pruritus
Delayed Cord Clamping
Pitocin timing after delivery with delayed cord clamping and pitocin’s affect on placental perfusion:
- Can still start pitocin immediately after delivery. Not shown to affect neonate perfusion in delayed cord clamping.
- IV transfer to fetus is not problematic : IV pitocin is molecularly identical to endogenous pitocin* which every fetus is obviously exposed to in labor (but IV allows a higher plasma concentration than endogenous stores.) Also women are routinely on IV pitocin for hours through vaginal deliveries – fetal transfer not shown to be problematic.
————————————————————————
PDPH can happen with spinal needles too! Especially if you accidentally poke through dura with the long local “finder” needle without realizing… (larger bore cutting needle)
Physiologic Responses to Neuraxial
** spinal surgical block should have even coverage bilaterally, whereas an epidural surgical block can have windows and different block heights/density bilaterally – b/l block assessment is important.
Helpful presentation on Slideshare – brief, simple summary of management for all kinds of spinal & epidural issues/troubleshooting/emergency responses:
COMPLICATIONS OF SPINAL & EPIDURAL ANAESTHESIA
PHYSIOLOGIC RESPONSES:
Can expect INCREASED HR:
- Baroreceptor reflex response to HOTN & decreased preload (HR x SV = CO), MAP = CO x SVR
- Lower SVR from sympathectomy-induced vasodilation (blocking sympathetic chain) AND lower CO via lower preload (SV)
- *Also tachy if she got terbutaline* (B2 agonist)
- Anxiety as block sets in/surgery about to start/ pt feels heavy, numb, paralyzed, and nauseous – sounds fun 😓
Q: If CSE performed – when should you test dose if HR is so variable for different reasons? False(+)?
A: We don’t test dose epidural catheter until we need to use it.
- There’s no time – the hyperbaric spinal dose we administered is settling sacrally with each passing second – Just thread the catheter, throw one dressing/tegaderm on, and lay them down before the spinal dose settles in the sacrum. You can aspirate catheter w pt supine for blood/CSF and if (+) we don’t use the catheter. Womp Womp…such is life
- Many other reasons exist for tachycardia during this time that interfere w epi test dose evaluation – eg: anxiety, baroreceptor reflex. We don’t need to use the epidural until the spinal wears off, and can test at that time.
More on tachycardia:
- Adrenaline may be a factor, or some IV epi from bolus (I’ve taken a few catheters out where the tip or one orifice is bloody- so pt gets most of the lido/epi in the epidural space from the other 2 orifices and had an adequate block, but a small amount also goes IV)
- However if you’ve just bolused an epidural for c/s with lido/epi and she’s tachy and HTN without an adequate block – suspect IV epi (and therefore IV LIDO) and monitor for s/s L.A.S.T
- When severe tachycardia happens right at the start of the case – and BP is otherwise stable, and it’s before you’re ruling out blood loss as a cause for tachycardia, beta blockers are ok. (Labetalol given all the time as ACOG protocol for HTN in PreE (along with hydralazine and nifedipine) – so it’s fine pre-delivery. BUT I usually start with a small dose of esmolol (5-10mg) in BB-naive pts under neuraxial so I don’t dig myself a hole. But don’t over-do it esp if she’s asymptomatic…. healthy women can absolutely tolerate some tachycardia for a little while… Generally the nerves settle out after baby delivered, and then there will be an expected SVR drop from IV pit, as well as the usual potential for hypovolemia from uterine bleeding, which will be exacerbated with anti-hypertenisives onboard. IF you must, give small dose, short acting BBs, as the sympathectomy from neuraxial will continue for 2+ hours. Sympathectomy + BBs = BP in toilet.
- So if she’s asymptomatic, let things settle for a little while – be judicious and conservative if treating and don’t dig a HOTN hole you can’t get out of. You also don’t want to mask/ignore a compensatory tachycardia response to hypovolemia from hemorrhage with long-acting Beta blockers.
If HR DECREASED shortly after spinal:
- Vagal? – Glyco mild, atropine +/- , epi severe (~10-20 mcg at a time).
- Beta blocked pt? (Labetalol commonly given for severe HTN)
- may be less capable of mounting baroreceptor reflex response
- Is the block high? T1-T4 = cardiac accelerator fibers – if pt develops whispering voice the block is high. Put pts head up and check grasp strength. Don’t reverse trend the whole bed – it’ll increase venous pooling and worsen preload/BP
- high spinal s/s = likely low HR from T1-T4 block, can see LOC with rapid desaturation & HOTN —> Intubate
- If LOC or pt codes from high spinal – intubate. You don’t need to push induction drugs. Secure airway. Don’t mask too much without cricoid pressure – she’s a full stomach. And ALWAYS use an oral airway to gently mask to reduce risk of gastric insufflation
- High/total spinal more likely if spinal performed after failed epidural 20cc bolus. Epidural volume compresses spinal canal CSF and pushes spinal block higher.
- DO NOT reverse trend bed if high/total spinal s/s, or spinal* block too high – it’ll just cause more venous pooling and decrease preload more. You CAN lift her head up though** just don’t put her whole body into reverse trend
- A high block is not the same as saying “high/total spinal” high/total spinal implies LOC, respiratory arrest, etc.
- Additionally, under spinal anesthesia, the degree of sympathectomy is greater than the degree of parasympathectomy. This increase in vagal tone, combined with fluid shifts, hormone shifts of term pregnancy and delivery, etc, can become a PVC playground. Ectopic beats are not uncommon, bigeminy can be seen, etc. As long as this isn’t a high-degree block, this is usually not something you have to treat or worry too much about. As long as mom is asymptomatic and perfusing well, just wait for the spinal to wear off and this will more than likely disappear. Unless she’s symptomatic in PACU, I don’t even get an ECG/labs if it’s just a few PVCs or in&out of bigemeny. If in the OR – I’ll give some glyco and ephedrine for bradycardic rhythms to limit the Ach/parasympathetic response, and boost the adrenergic response and override this vagal tone.
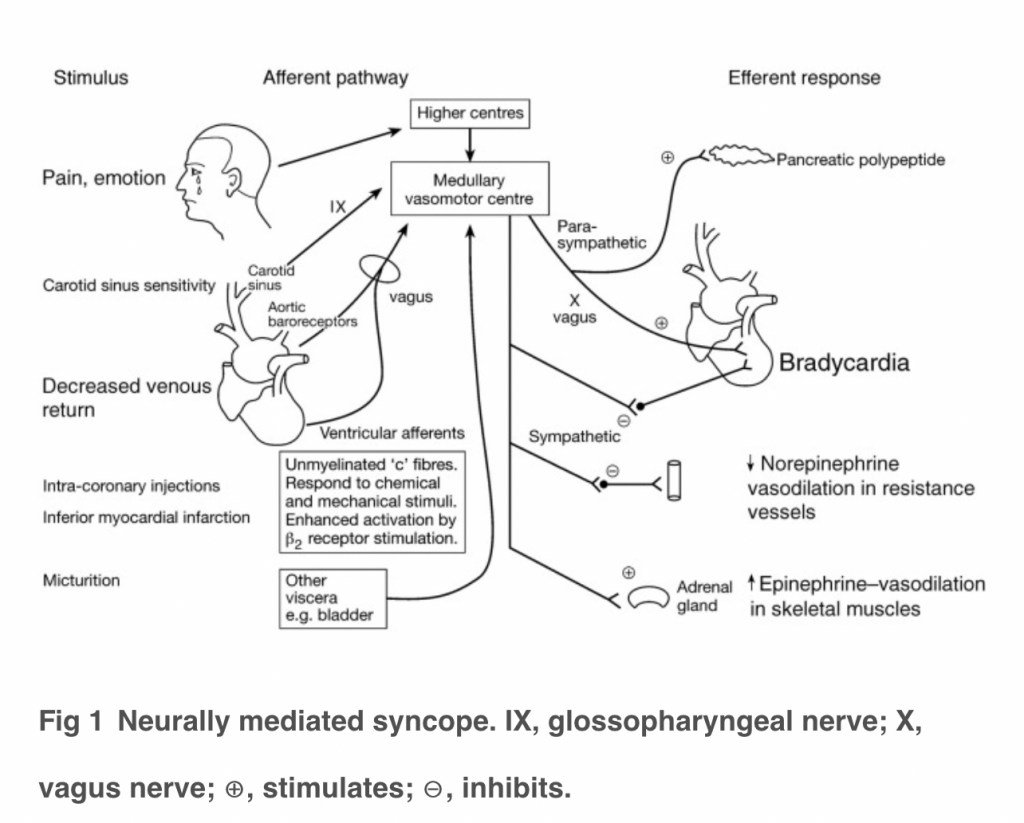
- Benzold-Jarisch reflex: Vagally mediated cardioinhibitory reflex: mechanoreceptors in LV are offloaded from decreased preload shortly after spinal sympathectomy. HR will reflexively slow down *drastically* to allow diastolic filling time. Can see long pauses between beats and asystole.
- can also happen with hemorrhage 2/2 profound rapid hypovolemia.
- ATROPINE 1mg (will help mitigate brady reflex, but won’t help increase blood flow to central circulation, which is the cause of the reflex)
- *EPI ~100-200mcg. (benefit of alpha* and beta* response)
- EPHEDRINE (alpha & beta, but longer time to onset than epi)
- Increase left uterine displacement (to increase preload) if baby not out yet.
- keep in mind profoundly bradycardic rhythms will not circulate meds quickly, may need CPR.
- Can be difficult to assess BJR vs total spinal – manage s/s as they develop. Total spinal will also have bradycardia as T1-T4 cardiac accelerator fibers are knocked out, but pt may complain of high block beforehand. Both can manifest as LOC and cardiorespiratory arrest: total spinal causes an anesthetized brianstem, and BJR asystole patients are not going to be breathing either. Either way – manage airway and circulation.
- LEFT LATERAL TILT/ UTERINE DISPLACEMENT
- Atropine & begin CPR to circulate it
- EPI if unresponsive to atropine —> full ACLS
- Secure airway
HYPOTENSION:
(HIGH BLOCK vs HIGH SPINAL/TOTAL SPINAL discussed more in detail further down)
- NOT tolerated in baseline HTN pt (preE, gHTN, cHTN, SIPE, HELLP)
- *Low BP = low placental/fetal perfusion
- Spinal causes sympathectomy from T4 down.
- Can be severe in pts being treated for HTN (preE) (intravascularly dry 2/2 third spacing, and often have labetalol, nicardipine, or hydralazine onboard)
- HTN 2/2 preE, which despite HTN, causes intravascular hypovolemia. The HOTN can be very severe in these pts s/p sympathectomy. We are now vasodilating a hypovolemic pt. PreE & all HTN pts should have a phenylphrine gtt running as soon as spinal is placed.
- *****^^^^the answer here to this relative hypovolemia is NOT to flood them w fluids – just give neo. (Discussed later in Cardiac Disease in Pregnancy – but preE pts are at higher risk of diastolic dysfunction, and the massive preload about to hit them from autotransfusion after delivery can cause cardiac compromise/pulm edema if they are already volume overloaded. Just use phenylephrine until delivery and then titrate it off.
- side note: neo gtt not necessary in labor epidurals for these HTN pts bc it’s a much lighter block w slow onset to allow for HD compensation. Spinals cause rapid sympathectomy w a surgical block density. Dosing a surgical-level epidural for c/s, though, may warrant a neo gtt in these pts. (Also L&D doesn’t run pressors on the floor – it’s Med-surg level)
- Not only does existing HTN mean the fetus is used to a higher perfusion pressure: (max uteroplacental vessel dilation at term pregnancy – no autoregulation – perfusion is MAP-dependent) but PreE is assc w poorly developed uteroplacental vasculature. So any decreases in placental perfusion can mean dramatic decreases in fetal perfusion.
- Fetal acidosis and hypoxemia.
- Anaphylaxis to LAs is very rare, especially with amides (bupivicaine). Higher incidence of allergic rxns with esters (e.g. chloroprocaine) due to metabolite: para-aminobenzoic acid (PABA), which is structurally similar to methylparaben. Esters are not used for spinal anesthesia for cesarean due to their shorter duration of action.
DROWSINESS
- CNS effect from opioids in spinal. CSF oscillates with arterial pulsations to move medications/narcotics around spinal cord/brain. Duramorph* especially (hydrophilic) will linger around in solution and circulate around cns 12-24 hrs providing some post-op pain relief.
- The fentanyl is more for a quick dense neuraxial block onset (lipophillic – diffuses rapidly across nerve cell membranes) doesn’t have long-lasting effects – maybe just some initial nose/face itchiness
NAUSEA:
- (usually 2/2 HOTN, or from exteriorization of uterus)
- rapid IV antibiotic dosing also causes n/v – slow ancef admin & azithromycin gtt.
- 1) ONDANSETRON:
- 5HT3 serotenergic mediators released from hypo-perfused GI tract – prophylactic zofran can help a little w/ symptoms, but root cause is BP. Neo usually 1st choice since HR usually increases with the decreased BP.
- BP is relative to pt. Maintain pt at pre-op BP (preE, GHTN, etc) The placenta/fetus is used to this perfusion pressure ** esp if fetus is already stressed/uteroplacental insufficiency. NEO gtt appropriate for pts with baseline HTN whether chronic or from preE/gHTN, etc.
Regulation of serotonin release from the intestinal mucosa – ScienceDirect
- 2) GLYCO/ATROPINE:
- Given if n/v persists despite normal BP
- Sympathetic outflow to GI tract arises from T5 to T12, while parasympathetic innervation = vagus nerve. Sympathectomy assc w/ neuraxial block in the mid- to low-thoracic levels results in unopposed vagal tone. S/S: increased peristalsis, relaxed sphincters, an increase in GI secretions, and, likely, more rapid restoration of GI motility in the post-op phase. N/V commonly accompany hyperperistalsis and can be treated effectively with IV atropine (or glyco). (NYSORA)
- T4 block causes sympathectomy: (block adrenergic receptors A1, A2, B1, B2) = unopposed parasympathetic (Ach) innervation below T4. GI tract is major player (rest/digest) mediated by Ach. Unchecked Ach in gut = hyper motility. —> n/v
- Glycopyrrolate (Anti-Ach) (or Atropine) can help block muscarinic Ach receptor sites on smooth muscle of GI tract, mitigating nausea 2/2 hypermotility.
- Can start with 0.1mg or 0.2mg.
- I’ve found 0.1 sometimes takes the edge off without causing an awful dry mouth or significant tachycardia, but I’ve often had to give the full 0.2mg anyway)
- This can generally be given irrespective of HR (Vomiting causes tachycardia too).
- Can start with 0.1mg or 0.2mg.
- 3) HALDOL: (Once baby is out)
- can be administered 0.5mg.
- 4) MIDAZOLAM (Once baby is out)
- 1mg as a last resort anti-emetic can do the trick if it’s relentless n/v. (The 2nd mg midaz if they need it, but again always go low and slow with these pts. And I always warn them this might affect their memory. Usually memories of barfing aren’t too cherished anyway.)
Exteriorizing the uterus
- (to sew it closed more easily) also a common cause of N/V – fundal and peritoneal/visceral traction releases Ach/5HT
- Uterine exteriorization increases micro Venous Air Emboli
- VAE – however small the emboli may be, has been found t occur in up to 97% of c/s!!!!
- While usually micro & is inconsequential in healthy pts, but if uterus is lifted up/out and is above level of heart, there is a possibility of a larger volume of entrained air (VAE), especially in pts with high risk (eg: Placenta previa).
- In pts with existing pulmonary HTN/PFO, ASD/VSD R–>L shunt/eisenmengers, cardiac pts etc as these micro emboli can be problematic as they cause pulmonary vasoconstriction. Can discuss leaving uterus in situ for closure in these pts.
Venous Air Embolism during Surgery, Especially Cesarean Delivery
Lethal Air Embolism during Cesarean Delivery for Placenta Previa
Panic attack after spinal*
- I mean can you blame her? Spinals sound awful.
- Try to talk mom off the ledge, reassurance.
- Consider we’ve just rendered her completely immobile with no control over her body while flat on her back. Then we stretch her arms out on arm boards and tie them with the Bair hugger straps. This can be a terrifying, trapped feeling that may, understandably, be very triggering for some women:
- Psychosocial Considerations:
- Rape and Sexual assault: 1 in 6 women have experienced rape or attempted rape in their lifetimes. (14.8 % rape, 2.8% attempted) (RAINN.org)
- Hx abuse and partner violence: As of 2019 “Homicide is a leading cause of death during pregnancy and the postpartum period in the United States. Pregnancy and the postpartum period are times of elevated risk for homicide among all females of reproductive age.”Obstet Gynecol. 2022. PMID: 35104077
- Midazolam 0.5 – 1 mg prior to delivery should have no effect on neonatal outcomes/apgar scores, however it’s considered best to avoid any narcotics/benzodiazepines, esp if there’s a stressed fetus.
- ***** JUST DON’T CONFUSE ANXIETY WITH HEART FAILURE OR HYPOXIA/PULM EDEMA.****
- If lying down flat suddenly makes her feel like she can’t breathe, or if after delivery (when autotransfusion is occuring and CO doubles, she suddenly feels anxious/impending doom – THIS MAY NOT BE ANXIETY – SHE MAY BE GOING INTO HEART FAILURE +/- FLASH PULMONARY EDEMA (OR VAE or AFE or PE etc!) So know your pt’s pre-op status and don’t take every “anxiety” claim at face value. Investigate further. [PreE pts also can have diastolic dysfunction and higher risk of pulm edema, as well as pts receiving MgSO4, and terbutaline.]
- But anyway, if it’s just after spinal at beginning of case [with no cardiac or higher pulm edema risk factors: r/o heart failure, pulm hypoxia?], and mom really needs anxiolysis, sometimes it’s worth giving midaz in small doses. If she’s having a terrible experience, she doesn’t have to remember every second of it. Versed should have no significant effect on airway reflexes or APGARs
- Also N2O for appropriate pts is safe for mom & baby 50/50 mix, ensure mom SpO2 remains > 95%. The mask might make claustrophobia worse. An already stressed fetus can’t tolerate decreased PaO2. Switch to higher or 100% FiO2, and figure out why mom’s sats are insufficient – r/o cardiopulmonary etiology of anxiety…
- Links below to Midazolam in c/s studies: safety and APGAR scores:
- https://pubmed.ncbi.nlm.nih.gov/24565384/
- https://pubmed.ncbi.nlm.nih.gov/16371613/
- https://pubmed.ncbi.nlm.nih.gov/27746564/
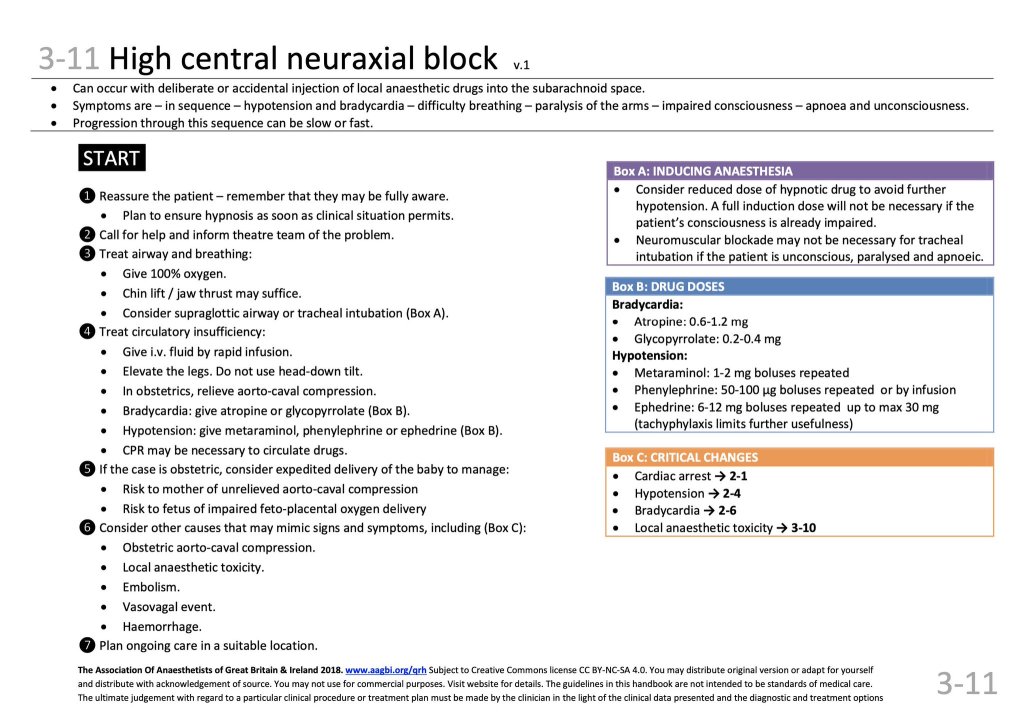
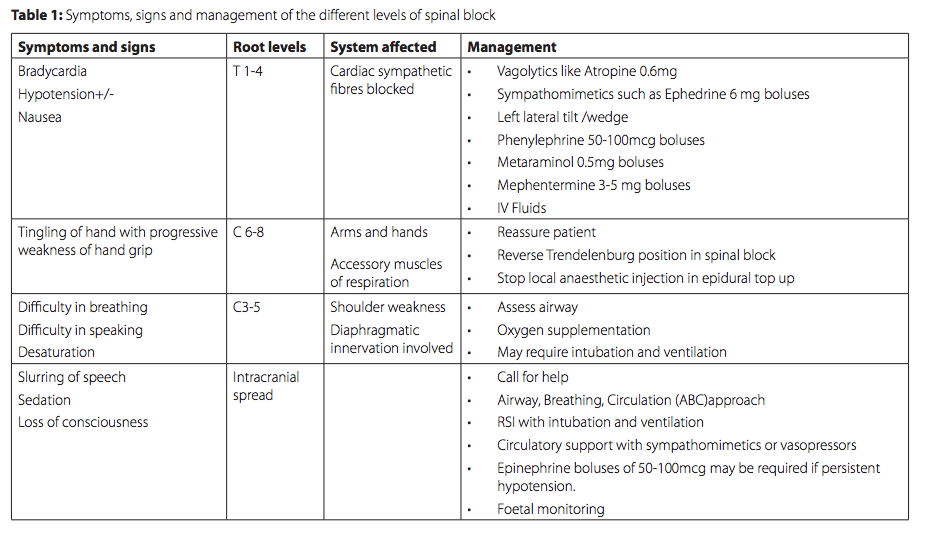
HIGH SPINAL/TOTAL SPINAL:
- This can be sudden LOC, or progress rapidly from a high block to a total spinal.
- HIGH BLOCK: usually be accompanied by:
- upper extremity weakness, hoarse voice/whisper, pt feeling heaviness in their chest “cant take a deep breath.” HOTN, bradycardia from T1-T4 cardiac accelerator fibers knocked out (unable to mount baroreceptor response of increased HR –> further HOTN on top of high sympathectomy and peripheral vasodilation), nausea/vomiting, significant patient anxiety, and akathisia(restlessness).
- If the block continues to rise to total spinal:
- brainstem dysfunction from LAs leading to LOC and apnea, and can lead to complete cardiorespiratory arrest
- Patients with a total spinal will have fixed, dilated pupils.
- cranial nerves involvement (CN2 – optic nerve, pupillary reflex)
ANESTHETIC MANAGEMENT HIGH/TOTAL SPINAL:
Call for backup – can progress to LOC/code
- If still conscious:
- Keep mom talking to assess for neurological changes/apnea etc while you treat HOTN and bradycardia:
- NYSORA: reverse trendelenburg does not prevent cephalad spread and may cause CV collapse 2/2 venous pooling from sympathectomy.
- Atropine, Phenylephrine, EPI (5-10mcg at a time) [*ephedrine indirect and takes too long]
- For small epi doses: 1mg vial epi shot into a 1L bag = 1mcg/cc, or into a 100cc bag = 10mcg/cc. LABEL the bags well.
- Manual Left Uterine Displacement to improve preload
- IVF bolus 500-1L (careful in cardiac pt or PreE pt – risk of flash pulm edema)
- Keep mom talking to assess for neurological changes/apnea etc while you treat HOTN and bradycardia:
- If Loss Of Consciousness:
- Immediate airway management & securement to prevent aspiration:
- Have SUCTION – high aspiration risk
- Cricoid pressure should be held and OPA used while masking/ventilating to minimize gastric insufflation and aspiratio risk. Apnea will cause rapid desaturation.
- NO induction agents – just intubate.
- Immediate airway management & securement to prevent aspiration:
- If CARDIORESPIRATORY ARREST:
- Normal CPR/ACLS, with uterine displacement. Secure airway with ETT, with cricoid pressure until cuff inflated/ during masking, NO induction agents needed.
- If no ROSC within 5 minutes: STAT C/S wherever you are in the hospital – do not move patient (i.e if high spinal occurs from inadvertent intrathecal catheter placement during epidural and total spinal code blue occurs in L&D room, CPR initiated and stat c/s performed in L&D room)
- (Maternal cardiac arrest algorithm in L.A.S.T page as well as Cardiac disease & Dysfunction In Pregnancy page) (Obstetric Difficult Airway management also has its own page)

A case of total spinal anesthesia
FAILED EPIDURALS & SPINALS for C/S
FAILED EPIDURAL for C/S:
- Long-duration > 24h epidural sometimes take a a little extra time and local to get to the surgical level (if time allows in non-emergent situations). Can switch lido and chloroprocaine dosing. Tachyphylaxis? Unknown what causes this I’ve just observed it.
- Also sometimes epidurals just need a little bit more time (again if this isn’t a crash section – a few more minutes of patience can avoid general)
- If true failure (no level, no sympathectomy) and non-emergent, can sit pt back up and re-attempt epidural/spinal. (They can re-prep and re-drape it’s not a big deal. Safer than needlessly instrumenting a high-risk airway.)
- If emergency —> convert to GA.
- If planning spinal, the incidence of high block and high spinal will now be higher due to the increased pressure/expansion of the epidural space with the bolus we just gave. (epidural space expanding into/compressing intrathecal space —> increases spinal block height)
- we can maybe give smaller spinal dose to accommodate for higher block height. ~ 1cc , and leave them sitting up a little longer.
- Spinal dose after failed epidural —> expect high block, can also cause high spinal: sometimes hoarseness first, can progress to LOC requiring ETT. Will have profound HOTN —> pressors
FAILED SPINAL for C/S:
Dose is either in epidural or subdural space.
Repeat procedure.
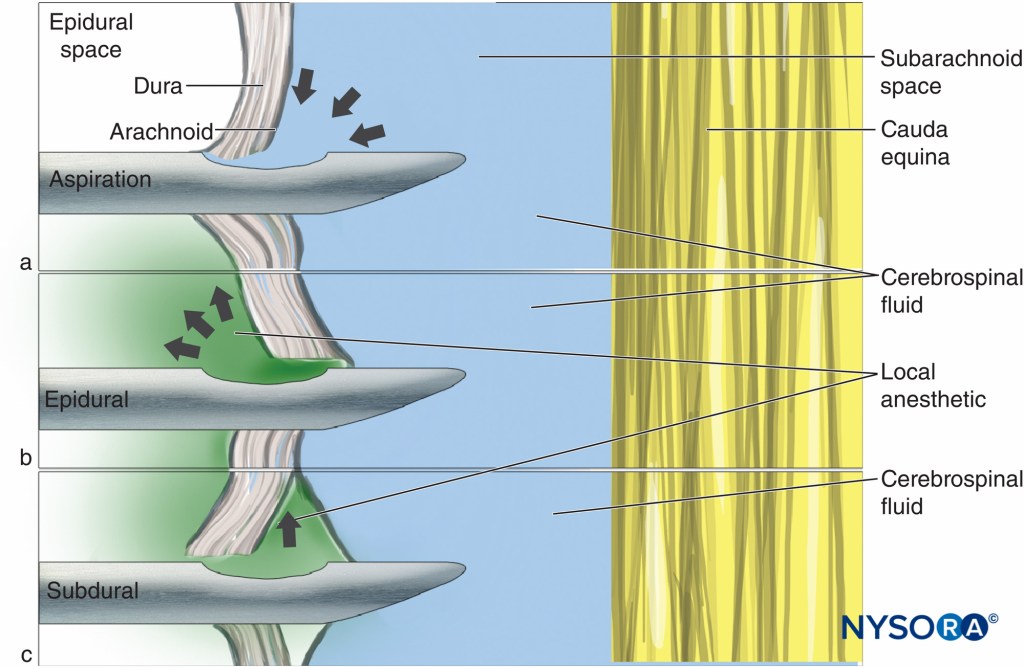
Subdural* injection will be a patchy block
https://academic.oup.com/bja/article/85/3/474/247839
PHYSIOLOGIC CHANGES AFTER DELIVERY
This is the most critical time of a c/s. This is where massive fluid shifts happen (as uterus continuously contracts down), as well as massive hemorrhages (when placenta is removed to expose open uterine spiral arteries inside uterine wall that were previously feeding placenta). Oxytocin can cause a brief decrease in SVR and drop in BP, at the same time a hemorrhage can cause a drop in BP. CAREFUL monitoring of pt during this time. If the pts on a neo gtt, start titrating down to avoid masking hypovolemia from hemorrhage with pressors. If there is a hemorrhage, the patient needs volume resuscitation – not pressors. (discussed further down in hemorrhage management)
- Cardiac pts can decompensate 2/2 CHF and develop pulmonary edema
- HTN (preE/HELLP) pts at higher risk of pulmonary edema 2/2 endothelial damage and diastolic dysfunction
- IF BP drops from baseline in hypertensive pt post-delivery – no fetus to perfuse anymore – if mom is asymptomatic (n/v) and “tone is good” aka bleeding is controlled – it’s OK. No need to continue super-tight BP control.
- If BP drops in cardiomyopathy pt – may be decompensating from fluid overload – consider inotrope. (ephedrine, low-dose epi, dobutamine, dopamine) and lasix.
**Autotransfusion**
Immediately After Delivery:
1.) Great vessels esp IVC now offloaded when baby is out. Large preload can now easily rush back to heart
2.) ~750cc/min of blood vol that was supplying massive gravid uterus now is returned to central circulation as uterus contracts down in a continuous systole.
3.) Compounded by the 999mL/hr IV pitocin bolus we are running ~ 200cc
- Can cause huge strain on compromised heart or fluid-overloaded patient. Can tip balance:
- flash pulmonary edema, left or/and right heart failure, congestive heart failure (covered in more detail in cardiomyopathy/high risk OB pages 5)
- If pt exhibits new sudden s/s panic, SOB, impending doom, air hunger, squirming, “NEEDS to sit up” —> possibly going into flash pulm edema/cardiorespiratory failure from fluid overload.
- O2, POCUS lung, POCUS TTE,+/-lasix, +/- Nitroglycerine +/- inotropes)
- Terbutaline (B2 agonist: tocolytic) carries risk of pulm edema. B-agonists alter alveolar-capillary permeability 2/2 increased hydrostatic pressure of increased HR & CO. Terb also places pts at higher risk of airway swelling (& easier obstruction)
Shivering: “The birthquakes”
- Starts just before or just after delivery, should only last 1 hour or so postpartum
- Treatment will begin post-op or post-partum, as this usually runs it course for an hour or so and resolves soon afterward.
- If it seems more like a dystonic rxn from the 10mg preop reglan (and then maybe she got PONV haldol after delivery ) Tx w/ Benadryl 12.5-25mg IV (ACh & dopamine out of balance. Too much CNS ACh after dopamine blockers reglan & haldol. (Glyco won’t help block Ach in this case as it doesn’t work centrally (quarternary amine doesn’t cross BBB) – no CNS effect. Benadryl (1st gen antihistamine & Ach-blocker crosses BBB) will decrease ACh.
- If it’s the normal birthquakes and they’re lasting > 1hr and are distressing to mom, can give Demerol (meperidine) 12.5mg IV (kappa- opioid receptor agonist – reduces shivering threshold). We rarely give Demerol except in severe, unrelenting shivering that is very distressing to mom. Giving lowest possible dose limits known negative side effects of meperidine.
- Meperidine metabolites cause cns excitability & decrease seizure threshold.
- metabolites pass to fetus and cause somnolence, can decrease seizure threshold (esp pre-term)
- Not for pts with seizure hx. The shivering will eventually subside on its own.
- Can also treat with PRECEDEX/dexmedetomidine in pts for whom meperidine is inappropriate: Effective doses studied from 0.3-1mcg/kg. Should start on lower end ~0.3 – 0.5mcg/kg.
- Meperidine metabolites cause cns excitability & decrease seizure threshold.
Optimal Dose of Prophylactic Dexmedetomidine for Preventing Postoperative Shivering – PMC
* How to Manage a Spinal Wearing Off*
~ VERSED & KETAMINE ~
+ glyco if you’re worried about Ketamine secretions…


- Epidurals can be re-bolused with LA 5-10cc at a time, and additional 50-100mcg epidural fent can be administered if necessary. Pain after delivery usually visceral from exteriorization of uterus and traction. Also cramping from pitocin gtt strongly contracting the uterus may be uncomfortable. This visceral discomfort is sometimes hard to cover with neuraxial anesthesia, so small doses of versed & ketamine can be warranted even with an epidural in place during the C/S. (If additional LA epidural doses are not working to cover pain)

- Do NOT let the dark inner voices tempt you into using propofol. Caution even throwing IV fent into the mix – they have swollen pregnant airways (esp if they’ve been pushing at all) and they can get obstruct/hypoventilate/apnea, and their FRC doesn’t tolerate ANYTHING. You do NOT want to be jaw-thrusting and masking a woman in front of her awake support-person. And you shouldn’t mask a full stomach. DO NOT give propofol. You will be so tempted. RESIST!
- Stay strong if the OBGYNS try to pressure you into GA for non-emergencies. They will try. Hold your ground and protect your patient. Ketamine will get you through 99% of the time. This is a high risk airway that they honestly have zero responsibility for if it goes to sh*t. GA is not a magic wand. Bless their hearts but they do not manage airways.
- If everything’s stable and they’re just closing (usually when this situation arises), and pt is feeling them touch her more than she’d like to – ask surgical team if they can “please pause briefly until you have pt in a more comfortable place.”
- You can do *ANYTHING* with *Ketamine* if you give enough. You can do the entire surgery under ketamine (once baby out). Definitely not ideal but .. it WILL get you through literally anything. It’s the top military med for severe field injuries. Traumatic amputation? Ketamine. It’s been used successfully and safely for ENTIRE surgeries as a sole anesthetic worldwide in remote/emergent situations for decades. Its on the WHO list of essential medicines. It’s safety profile is very, very well tested.

Ketamine Use in Operation Enduring Freedom
Ketamine Pharmacology: An Update (Pharmacodynamics and Molecular Aspects, Recent Findings)
Ketamine Quick Review
- NMDA blocker, phencyclidine derivative (cousin of PCP)
- Dissociative agent: sensory input may reach cortical receiving areas, but fail to be perceived in some association areas.
- Analgesic effects persist for plasma concentration 1/10th hypnotic concentration
- Powerful bronchodilator for intractable bronchospasm
- Causes secretions (glyco if needed)
- Can cause hallucinations (Versed give 1st always)
- Crosses BBB (and placenta): Not recommended during pregnancy, but after delivery is fine.
- concern during pregnancy is uterotonic effect, as well as potential fetal neurodevelopmental effects based on rodent data: cognition & memory impairment after single dose found in rats. (Mickley et al., 2004)
- OK for breastfeeding – minimal transfer and low oral bioavailability
DOSING VERSED & KETAMINE
GO LOW & SLOW
Even though midazolam & ketamine maintain spont resp, this is a swollen airway at term pregnancy, made worse by preE/HELLP , tocolytics*(terbutaline) and PUSHING in labor. If this c/s was after laboring/pushing, expect ++ airway swelling. Even tiny doses of sedation can obstruct them alarmingly easily.
Go LOW and SLOW. Slamming these meds in all at once can still cause this crappy airway to obstruct. Even a quick 2 of versed can make them obstruct (from personal experience). Preggo airways are scary. Do not mess with them. Do not underestimate them.
- Start with 1cc each: 1 mg versed & 10mg (1cc) ketamine. Warn them they might feel funny. ALWAYS give versed FIRST . START LOW. Wait a few minutes for this dose to really kick in.
- If not enough, 10mg/1cc more ketamine, wait another few minutes.
- If not enough 10mg more ketamine
- Then 1mg more versed. ADD 0.2 GLYCO IF ++ SECRETIONS
- If not enough, 10mg more ketamine….
- If not enough, 10mg more ketamine….
- Keep following this incremental dosing – it may take 5-10 minutes but OKAY. Keep waiting for each dose to take effect and see how far you can get with the least amount. .
- Pts rarely need a full syringe, but some need even more!
- These women haven’t even had a drink in 9 months, they’re sensitive – start low & slow. They may feel very strange with these meds.
- KEEP dosing INCREMENTALLY. Wait for effect, assess efficacy.
GO SLOWLY BUT BRAVELY INTO THE K-HOLE.
IN KETAMINE WE TRUST.

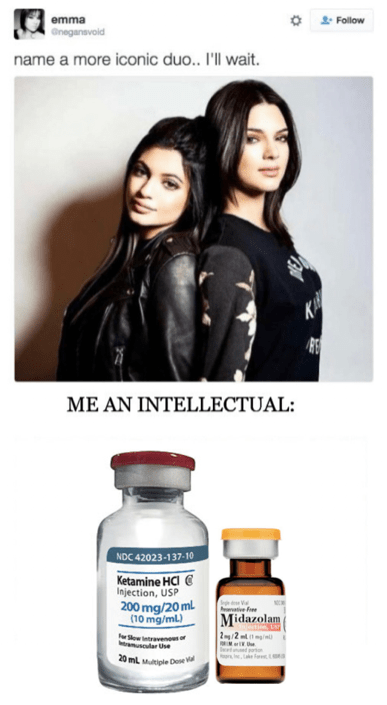
If you still must ultimately convert to GA for some crazy reason – baby is now out.
(GA for CESAREAN outlined in separate page)
- RSI still but don’t need to dramatically announce when you’re through the cords.
- Maintain same principles outlined below of 1/2 Mac sevo, with versed after bc we’re still not going full MAC sevo (uterine tone) and want to ensure no recall with lower gas.
- Usually don’t need to maintain paralysis. Place bite block after intubation (oral airway) & get them back breathing first, THEN titrate small narcotic doses to RR (you have intrathecal narcotics in place as well)
- Neuraxial order set still ok bc intrathecal opioids are still active.
- I use propofol pushes for periods of stimulation to keep them a little deeper – spare narcotics and paralysis, and it’s quick on and off.
- Gentle* OGT placement to drain stomach and decrease aspiration risk. Avoid oropharyngeal trauma and increased swelling.
POST-OP
- Any issue with hemorrhage? If so – wait for coags/PLT to pull epidural (if in place). PLT > 70-100, Fibrinogen > 300 (normal 200-400, pregnancy ~ 500)
- Any issue with the placenta? Did it come out easily and completely? If any doubts – DON’T PULL THE EPIDURAL (if in place) – you can use it if pt needs to go back to OR for evacuation of retained products, and avoid having to do GA if it’s emergent.
PRURITIS
Central vs Peripheral?
Spinal vs Epidural narcotics?
Nubain (Nalbuphine) vs Benadryl?
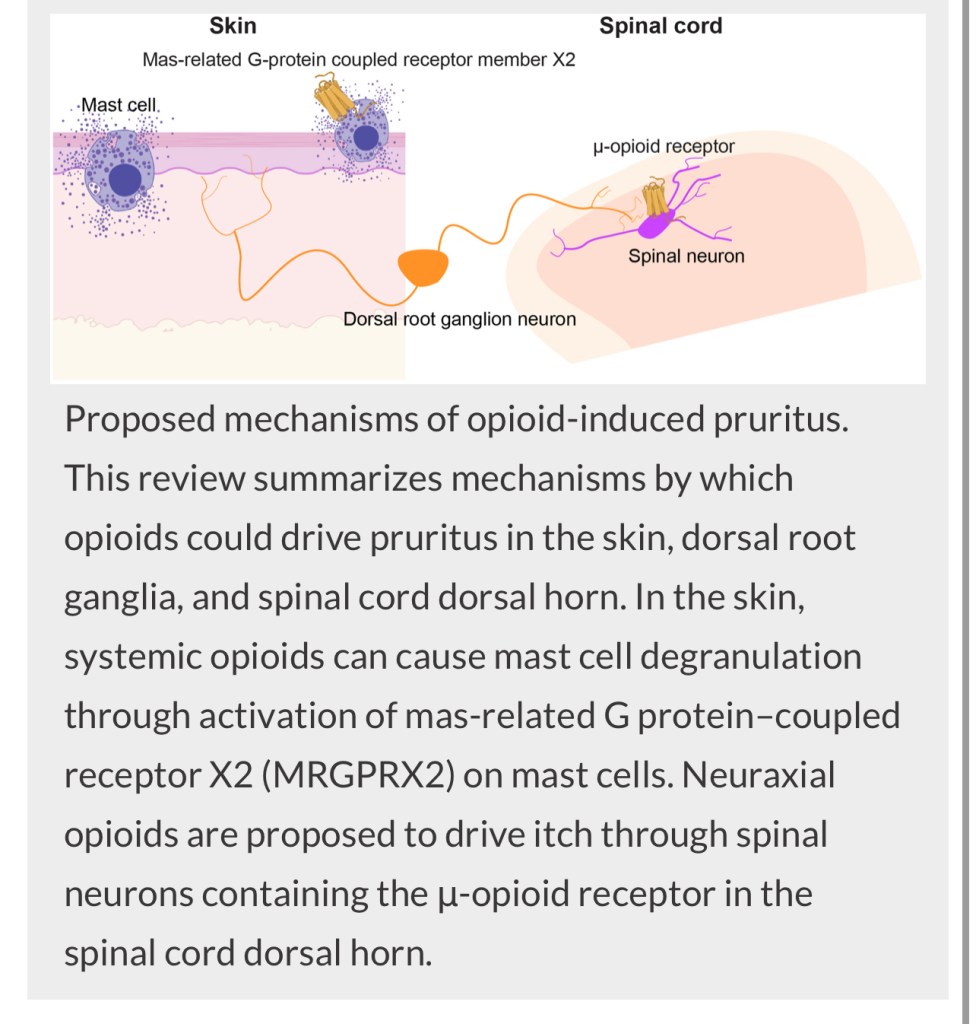
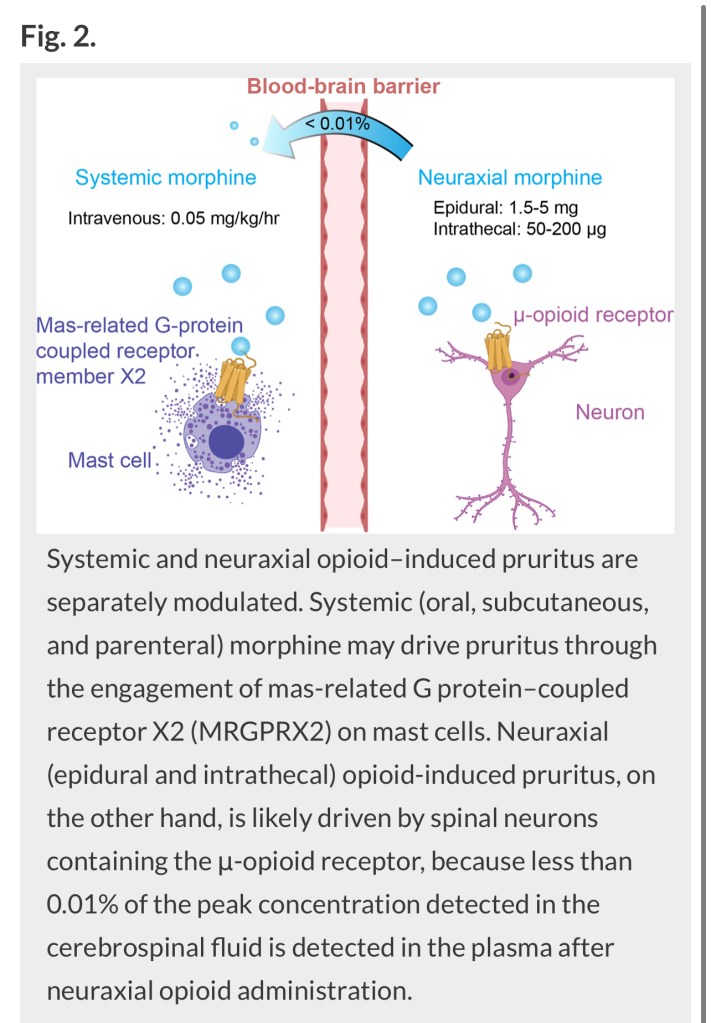
Pruritis after Epidural
Benadryl can help pruritis from peripherally administered opioids (IV) by stabilizing mast cells. The epidural opioids (100mcg fent and 3mg morphine) may show some combined peripheral and central pruritis as some systemic uptake occurs. Pt may still need Nubain if Benadryl ineffective.
Pruritis after Spinal
With intrathecally administered opioids (10 mcg fent, 100 mcg duramorph) systemic absorption is negligible & unlikely to have peripheral mast-cell-mediated pruritis, rendering Benadryl ineffective.
Nubain is therefore tx of choice for pruritis after intrathecal opioids*
Post-op HYPOTHERMIA
Not the same as “The Birthquakes” discussed in the previous section.
- Post-op Hypothermia is often asymptomatic/no shivering, but temps can be as low as low 90s F, and can be attributed to intrathecal morphine impairing thermoregulatory control.
- Hypothermia can increase bleeding via impairment of enzymes regulating coagulation factors, inhibiting thrombin generation, and impairing fibrin function.
- TREATMENT: LORAZEPAM +/- Nalbuphine or naloxone.
- Lorazepam 0.5-1mg IV as a single dose has been shown to rapidly correct temperature (starts working within ~ 10 minutes) Midazolam 1-2mg IV works too, but its short duration of action limits efficacy and practicality. Diazepam is not recommended due to the excessively long Et1/2 and active metabolites which can pass to the newborn and cause somnolence.
- Nalbuphine / naloxone usually not necessary
Coagulopathy by Hypothermia and Acidosis: Mechanisms of Thro…