re: Anesthesia
REVIEW MATERIALS & RESOURCES
Some general OB reviews & guides from different sources (ASA, MGH, University medical centers) that are helpful to read over/cross-reference.
- You’ll see a ton of overlap to read the same thing a few different ways
- You’ll get a better sense for our own institutional culture of how we do things vs. how other institutions do things, which are also safe and fine.
- There are many ways to safely and effectively deliver care:
OB Anesthesia Survival Guide | Renaissance School of Medicine at Stony Brook University
Open Anesthesia has A TON of OB resources, including various recorded SOAP lectures (also embedded throughout this website):
https://www.openanesthesia.org/sections/obstetric-anesthesia
Practice bulletins in ACOG Clinical for *Everything*:
OBGYN Resources and practice guidelines: ObG Project Homepage:
NORMAL CHANGES IN PREGNANCY BY SYSTEM
CARDIAC
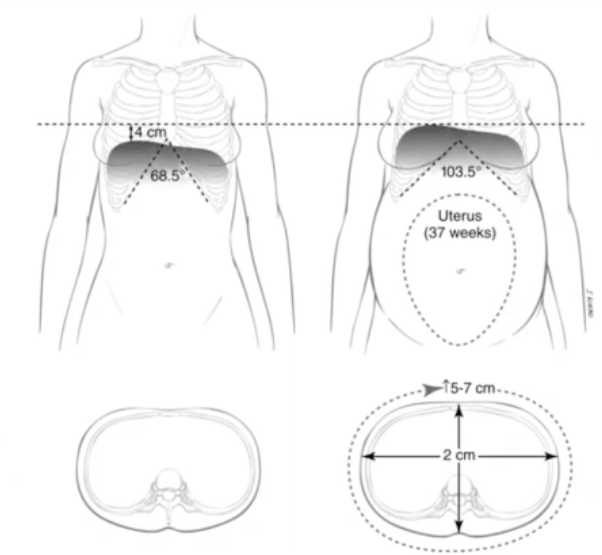
- Heart displaced cephalad & laterally by gravid uterus.
- EKG changes of pregnancy include:
- 1) sinus tachycardia
- 2) other dysrhythmias: atrial & ventricular ectopic beats
- 3) ST depression: inferior & lateral leads
- 4) T wave flattening/inversion in inferior & lateral leads
- 5) LVH and
- 6) LAD.
- 7) Small Q wave, and inverted T wave in Lead III
- Just wanna throw this in here: under spinal anesthesia, the degree of sympathectomy is greater than the degree of parasympathectomy. This increase in vagal tone, combined with fluid shifts, hormone shifts of term pregnancy and delivery, etc, becomes a PVC playground. Ectopic beats are not uncommon, bigeminy can be seen, etc. As long as this isn’t a high-degree block, this is usually not something you have to treat or worry too much about. As long as mom is asymptomatic and perfusing well, just wait for the spinal to wear off and this will more than likely disappear. Unless she’s symptomatic in PACU, I don’t even get an ECG/labs if it’s just a few PVCs or in&out of bigemeny. If in the OR – I’ll give some glyco and ephedrine for bradycardic rhythms to limit the Ach/parasympathetic response, and boost the adrenergic response and override this vagal tone.
- EKG changes of pregnancy include:
- Cardiac O2 demand higher: pregnant ARDS pt may see additional benefit of ECMO over non-pregnant pt.
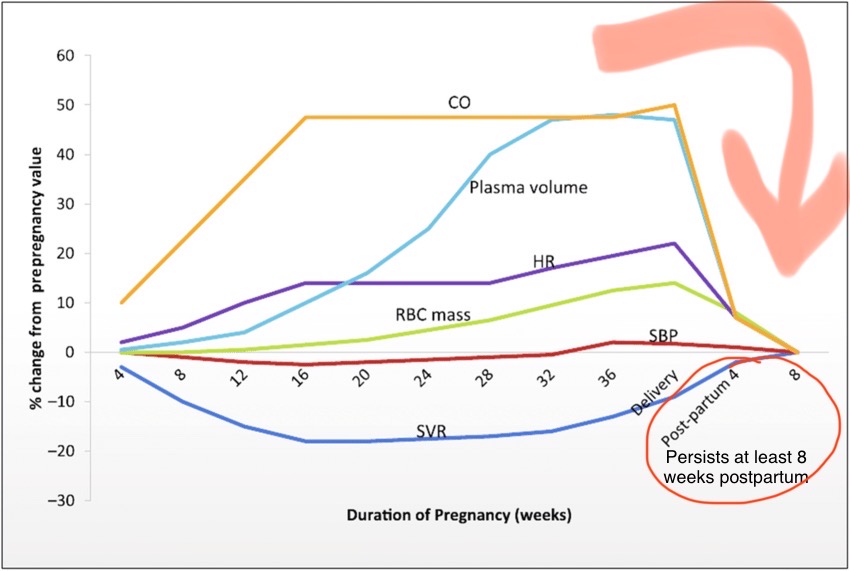
- Both SV and HR increase CO 40-50% by the 3rd TM (max at 24 weeks)
- Plasma volume increases throughout pregnancy, plateaus at 50% increase in 3rd TM
- SVR and PVR decrease, leaving central filling pressures unchanged, despite increased plasma volume and CO.
- BP drops approx 10 mmHg by 2nd TM despite 30-50% increase in intravascular volume
- Decreased SVR reduces SBP (8- 15%) and DBP (20%)
- 2/2 changes in estradiol, progesterone, nitric oxide, & prostacyclin.
- Increased venous capacitance & myocardial remodeling attenuate increased blood volume so CVP remains constant
- Relaxin: peptide hormone produced by corpus luteum, decidua, & placenta – stimulates endothelin which mediates vasodilation through N.O. synthesis
- Resistance to Angiotensin II
- SVR and PVR decrease, leaving central filling pressures unchanged, despite increased plasma volume and CO.
- Decreased serum colloid-osmotic pressure (15%) placing pregnant pts at higher risk of pulmonary edema and third spacing (airway swelling):
- compounded in setting of increased preload (IVF/autotransfusion) and/or increased membrane permeability (PreE 2/2 endothelial damage, Magnesium sulfate) & increased hydrostatic pressure from ^^CO 2/2 Terbutaline (B-Agonist)
- Enlargement of both atria and both ventricles by the end of pregnancy.
- LV mass increases by up to 50% by 3rd TM
- Eccentric hypertrophy noted w/ increases in LV mass & septal thickness.
- Cardiac imaging (TTE/MRI) show cardiac remodeling occurs, and many of the pregnancy changes are often reversed 6 – 8 months postpartum.
- Places cardiac/HF/PPCM pts at longer-term risk post-partum for further complications, continued HF.
- Systolic regurgitation murmurs (usually mitral or tricuspid in origin, can also be pulmonic) can develop in normal pregnancy from fluid overload.
- Mild regurg can be normal physiologic finding.
- In HOTN, pt may benefit from adding IV push ephedrine over just neo, as beta inotropy can help LV overcome SVR and decrease regurgitant fraction. If known MR pt continues to be HOTN/tachy – beta agonism may improve SV&CO and decrease HR
- Mild regurg can be normal physiologic finding.
- AFTER delivery through 48-72h postpartum, CO is the highest – CO is 80% higher than before delivery.
- Uterine invlolution = ~700cc autotransfusion, PLUS the removal of vena caval compression from previously gravid uterus = increased prelaod.
- They’re now 150% above pre-pregnancy levels ~ twice as high as term pregnancy which was already 50% above baseline.
- This increased CO can be detrimental to women with baseline cardiac dysfunction: pulmonary HTN, valvular lesions (ex. stenotic lesions) or cardiomyopathy. Pts can go into heart failure.
- Aortocaval compression decreases venous return & causes maternal HOTN —> fetal acidosis from hypo-perfusion, and can cause maternal HOTN & syncope
- Normal hemoglobin is 12 g/dL.
- Plasma vol ^ 45% at term, RBC vol ^ 20%,
- relative dilutional anemia – so no change in MCV/MCHC
- slightly elevated WBC/leukocytosis can also be a normal finding in term pregnancy, and in labor. Elevated lactate can also be normal finding in labor
- Epidural vein engorgement (Batson’s plexus) reduces the available epidural & CSF space, causing higher neuraxial LA spread.
Cardiovascular Physiology of Pregnancy
HEMODYNAMIC AND VOLUME CHANGES
POST-PARTUM HEMODYNAMICS
- CO remains elevated for the first few days after delivery to compensate for the intravascular fluid mobilization.
- Blood volume decreases by about 10% in the 1st week after delivery.
- SVR and HR return to normal within 2 wks postpartum
- SV and CO gradually decrease over several months
- For cardiac patients, these persistent postpartum physiologic changes make heart failure & arrhythmia continued risks in the days & weeks after delivery
PULMONARY & AIRWAY
- Mucosal capillary engorgement can compromise airway (use smaller ETT: 6.0-7.0)
- Oropharyngeal and glottic edema & increased vascularity
- Avoid nasal airways/ instrumentation – friable mucosal membranes are prone to significant bleeding & would complicate airway management
- Mallampati scores increase one grade higher in 33% (and 2 grades higher in 5%) of women after labor, as compared to before labor – pushing in labor increases airway swelling.
- Minute ventilation increases by ~ 50% via increased TIDAL VOLUME (Vt). (stimulated by progesterone (resp stimulant). RR doesn’t increase much.
- increased MV is 2/2 increased fetal metabolic demands
- Accessory muscle and chest wall compliance increases early in pregnancy, so ABG changes and ventilatory changes would be seen in early termination D&C/D&E as well.
- O2 consumption increases by 20%, while FRC decreases by 20%.
- Contributes to rapid desaturation
- Places pregnant women at higher risk of shock & acidosis with hemorrhage and loss of carrying capacity – underscores importance of replacing blood with blood in OB hemorrhage to maintain carrying capacity to meet O2 needs, and of limiting IV crystalloid (which does not increase O2 carrying capacity).
- FRC & closing volume:
- Contributing to rapid desaturation:
- Chest circumference increases 2/2 Elevation of diaphragm, which occurs w/ an increased uterus size. ERV, RV, & FRC decrease by 3rd TM. However, bc there’s also an increase in IRV, TLC remains unchanged. A decreased FRC is typically asymptomatic in healthy parturients. Those with preexisting alterations in closing volume 2/2: smoking, obesity, scoliosis, or other pulmonary disorders may experience early airway closure w/ advancing pregnancy, leading to hypoxemia. The Trendelenburg & supine positions exacerbate the abnormal relationship btwn closing volume & FRC.
- The residual vol & FRC return to normal shortly after delivery ~ a few days, but not immediately after.
- PREOXYGENATE prior to induction if GA required, then RSI with cricoid pressure
- Aspiration risk 2/2 progesterone relaxing lower esophageal sphincter tone and decreasing gastric pH. Generally after ~12 weeks, but ANY time she reports heartburn, even in early pregnancy, she should have ETT. RSI maintained postpartum 48-72 hrs, and then until any continued reported reflux resolves – may even take a few weeks. The full stomach 2/2 specifically slower gastric emptying really applies to active labor. However the decreased LES tone and decreased gastric pH (more acidic) is throughout basically all of pregnancy, with cephalad displacement of stomach, and increased intragastric pressure both increasing with gravid uterus.
- RSI, cricoid pressure, OGT (no NGTs, no nasal instrumentation), + pre-op bicitra & reglan (reglan/metoclopramide specifically increases LES tone by up to 10mm Hg)
- MAC decreases 20-30% in pregnancy
- Normal pCO2 is 32 mm Hg
- during labor, maternal pCO2 may fall as low as 17 mm Hg 2/2 hyperventilation. This resp alkalosis can cause acidosis in the fetus, bc the uterus, like the brain, dilates in response to pCO2, thus a hypocapneic uterus can vasoconstrict, potentially causing uteroplacental insufficiency.
- yay for epidurals reducing hyperventilation from pain
- during labor, maternal pCO2 may fall as low as 17 mm Hg 2/2 hyperventilation. This resp alkalosis can cause acidosis in the fetus, bc the uterus, like the brain, dilates in response to pCO2, thus a hypocapneic uterus can vasoconstrict, potentially causing uteroplacental insufficiency.
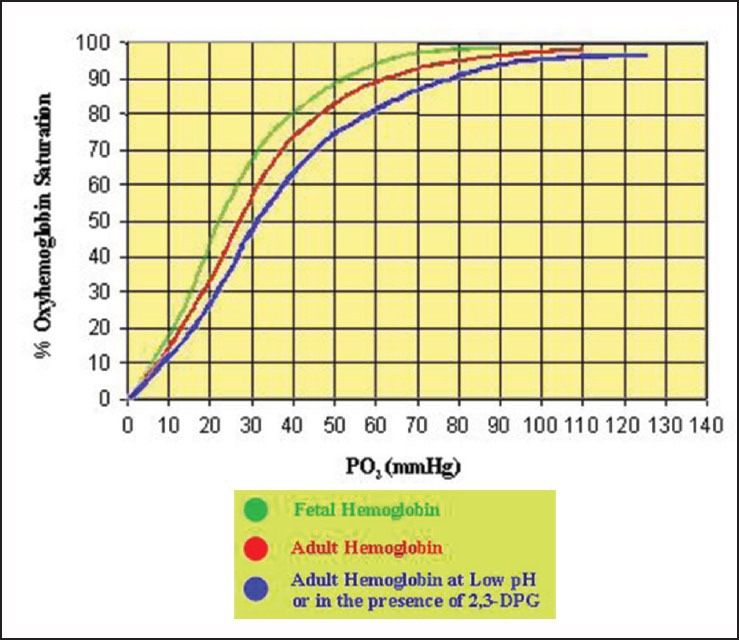
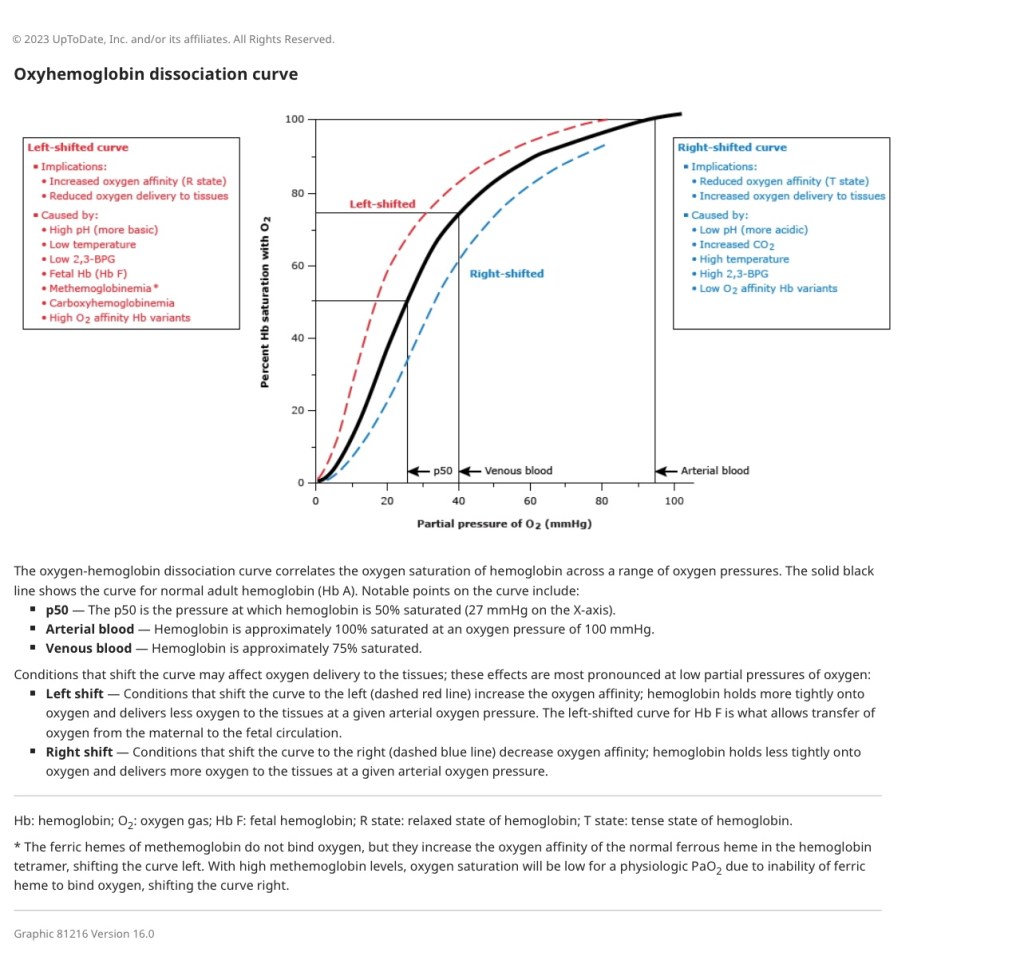
- Goal for pregnant pt: SaO2 > 95, PaO2 > 70 due to drop in fetal oxygenation below these levels based on fetal Hgb dissociation curves. [While many places do not routinely use supplemental O2 for c/s, it can always be added if SpO2 < 95%.]
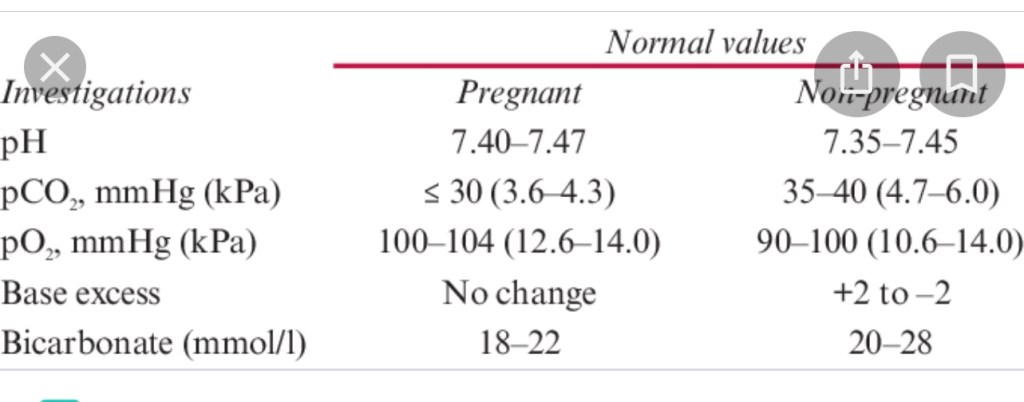
NORMAL ABG: PREGNANT VS NON-PREGNANT:
RENAL
- Renal blood flow increases by ~ 50% (same as CO)
- Increased GFR & CrCl by 10 wks
- Lower BUN/Cr (0.4-0.6 umol/L)
- (ex: 14wk abortion Cr 0.9 would be abnormally high) – question ketorolac, & renal workup)
- Lower BUN/Cr (0.4-0.6 umol/L)
- Kidneys excrete more bicarb in urine to match respiratory alkalosis
- HCO3- 18-22 in normal pregnancy, 20-28 non-pregnant
- diarrhea/bicarb loss could impair maternofetal pH balance
- HCO3- 18-22 in normal pregnancy, 20-28 non-pregnant
- Physiologic hydronephrosis common
- Increased GFR & CrCl by 10 wks
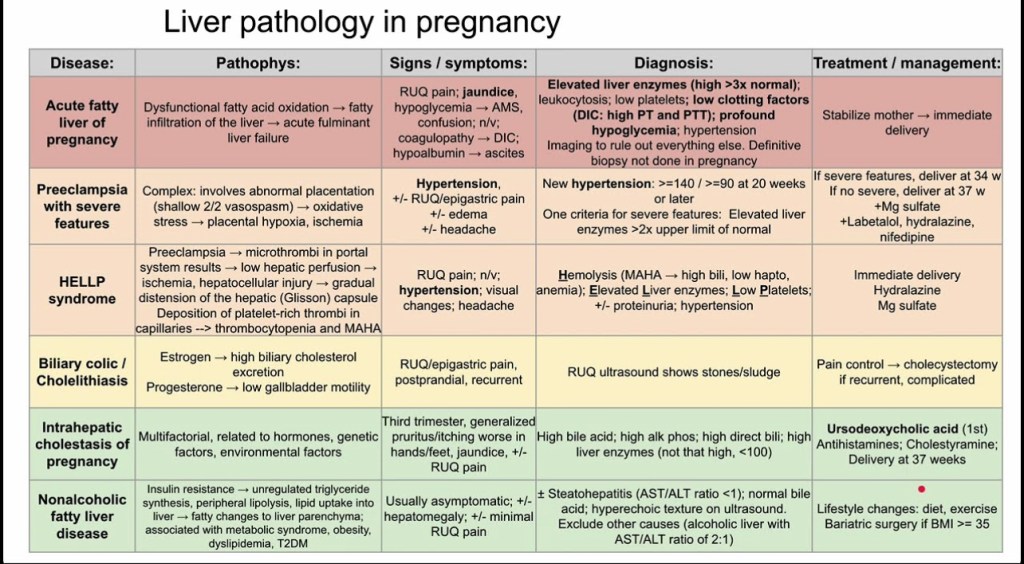
HEPATIC
- Serum proteins decreased 2/2 hemodilution, increasing medication potency.
- Plasma cholinesterases decreased ~ 25% at 10 wks, can prolong Succinylcholine.
- Only Alk phos is normally elevated in pregnancy (2-3x higher) from placental & fetal bone isoenzyme release. Increases through pregnancy as placenta and fetal bones develop.
- Other LFT elevations are suspect: significant AST/ALT increase is abnormal.
- preE, HELLP, Acute Fatty Liver of Pregnany (AFLP), cholestasis, viral hepatitis?
- Decreased gallbladder emptying in pregnancy –> cholestasis
- Liver failure in pregnancy will usually occur > 20wks 2/2 AFLP, PreE, or HELLP
- Prolonged PT/abnormal coags may be seen in setting if liver dysfunction.


The Liver in Normal Pregnancy – Madame Curie Bioscience Database – NCBI Bookshelf
COAGULATION
- THROMBOCYTOPENIA most common coagulation abnormality:
- hemodilutional effects but ^^ mean platelet volume suggest platelet destruction as well.
- Newly made PLTs are larger than older platelets, so a high number may signal that your bone marrow’s making a lot of new platelets.
- otherwise pregnancy is a HYPERCOAGUABLE state, with high VTE risk
- hemodilutional effects but ^^ mean platelet volume suggest platelet destruction as well.
- Factors (1, 2, 7, 8, 10 12, vWF fibrinogen) increase
- 4 -10x increased risk VTE/PE throughout gestation and the postpartum period.
- Protein S (anticoagulant) decreased, and acquired resistance to protein C (anticoagulant).
- Decreased fibrinolytic activity during pregnancy (returns to normal ~1hr after delivery)
- mainly caused by increased plasminogen activator inhibitor type 1 (PAI-1). PAI-1 = main inhibitor of plasminogen activators, eg: tissue-type plasminogen activator (tPA) and urokinase-type plasminogen activator (uPA). In human placentas, PAI-1 is expressed in extravillous interstitial trophoblasts and vascular trophoblasts.
- FACTOR 7 and FIBRINOGEN show highest increases, possible link to high VTE risk
- Normal fibrinogen level 350-600 by term.
- Pregnancy is a perfect storm of Virchow’s Triad:
- Venous stasis, increased coagulability factors, & increased endothelial damage.
- Left leg higher risk venous stasis 2/2 vascular anatomy. Left iliac vein compressed by left iliac artery & left ovarian artery. (on Right side, iliac artery does not cross the vein)
- additional risk factors: obesity, smoking, multiple gestations, AMA, increased parity, C/S, thrombophilia (F5Leiden, Antiphospholipid syndrome, Protein C/S deficiency).
- Unfractionated heparin and LMWH are 1st line tx.
- Venous stasis, increased coagulability factors, & increased endothelial damage.
So how are parturients not developing PEs left and right?
- Highest risk for VTE is still postpartum through 6wks PP. Obese pts, higher risk pts, Mild Factor 5 Leiden, etc may receive prophylactic LMWH POST-partum, despite not needing it during pregnancy.
- consider LMWH & hematoma risk if blood patch needed post-partum
- However only ~ 1hr after delivery, fibrinolytic activity returns to normal
- may offset some hypercoagulability and explain rarity of PE despite hypercoagulable state.
- Increases in:
- plasminogen
- alpha2-antiplasmin
- D-dimer concentrations (suggests ^^ fibrinolytic activity)
GASTROINTESTINAL
- Full Stomach 10-12 weeks through 48h (at least) postpartum. RSI until any continued acid reflux resolves post-partum – may be a few days.. May be a week..
- Aspiration risk 2/2 progesterone relaxing lower esophageal sphincter tone and decreasing gastric pH. Generally after ~12 weeks, but ANY time she reports heartburn, even in early pregnancy, she should have ETT. RSI maintained postpartum 48-72 hrs, and then until any continued reported reflux resolves – may even take a few weeks. The full stomach 2/2 specifically slower gastric emptying really applies to active labor. However the decreased LES tone and decreased gastric pH (more acidic) is throughout basically all of pregnancy, with cephalad displacement of stomach, and increased intragastric pressure both increasing with gravid uterus.
- RSI, cricoid pressure, OGT (no NGTs, no nasal instrumentation), + pre-op bicitra & reglan (reglan/metoclopramide specifically increases LES tone by up to 10mm Hg)
- Gastric emptying is reduced by cephalad pylorus and progesterone-mediated decrease in gastric motility *during labor.
- Nausea/vomiting:
- ondansetron and metoclopramide safe to administer while pregnant.
- Stomach acid has lower pH during pregnancy 2/2 progesterone
- Higher risk of constipation and hemorrhoids – narcotic doses exacerbate this – non-narcotic pain medicine helpful when possible.
ENDOCRINE
- Increased insulin resistance – GDMA as common as 1 in 12 to 1 in 7
- Increased thyroid hormones – higher normal ranges for TSH, free T3 & T4
- upper limit TSH raised to 5.5 μmol/l, vs 4.0 μmol/l non-pregnant.
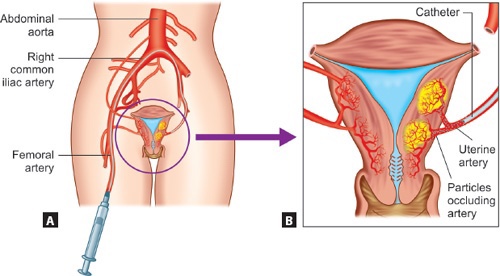
UTERINE VASCULAR ANATOMY
- Uterine arteries branch off the internal iliacs (whereas ovarian arteries branch off the aorta)
- Uterine arteries can be embolized in IR (usually elective for uterine fibroids) but also to stop hemorrhage.


Changes in the uterine vasculature during pregnancy
Maternal UTERINE *SPIRAL* ARTERIES
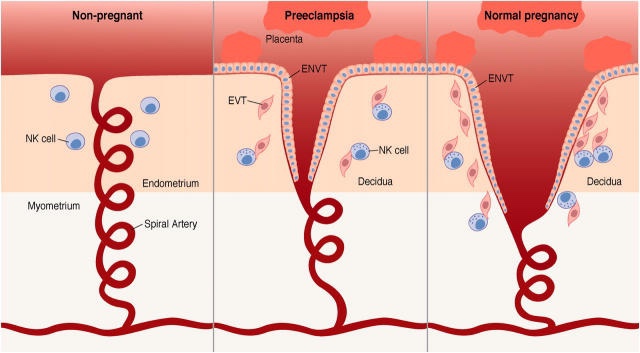
- We will come back to these again and again. They are a huge player in OB hemorrhage and in Preeclampsia.
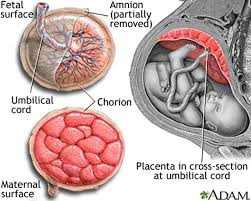
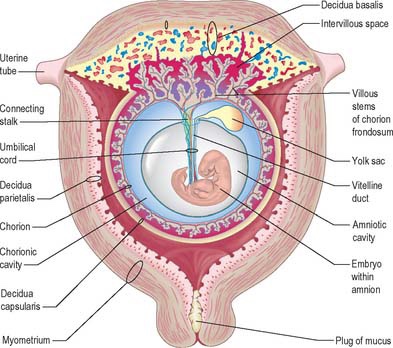
- Uterine spiral arteries run through the decidua (aka endometrium when non-pregnant) to directly supply the placenta. During normal pregnancy, spiral artery lumens undergo radical structural transformation by trophoblasts to become wide open, high flow, low-resistance vessels to supply the placenta (with a ton of blood: 500-700cc/min by term)
- Spiral arteries are a distal branch of uterine radial arteries. Pitocin keeps these spiral arteries from bleeding by making the uterine muscle/myometrium contract and physically clamp down on/around the arteries supplying these wide-open spiral arteries:
- Uterine blood flow is MAP-dependent by term as these arteries are maximally dilated and lose their inner arterial smooth muscle lining through normal trophoblastic remodeling, leaving them unable to vaso-react.
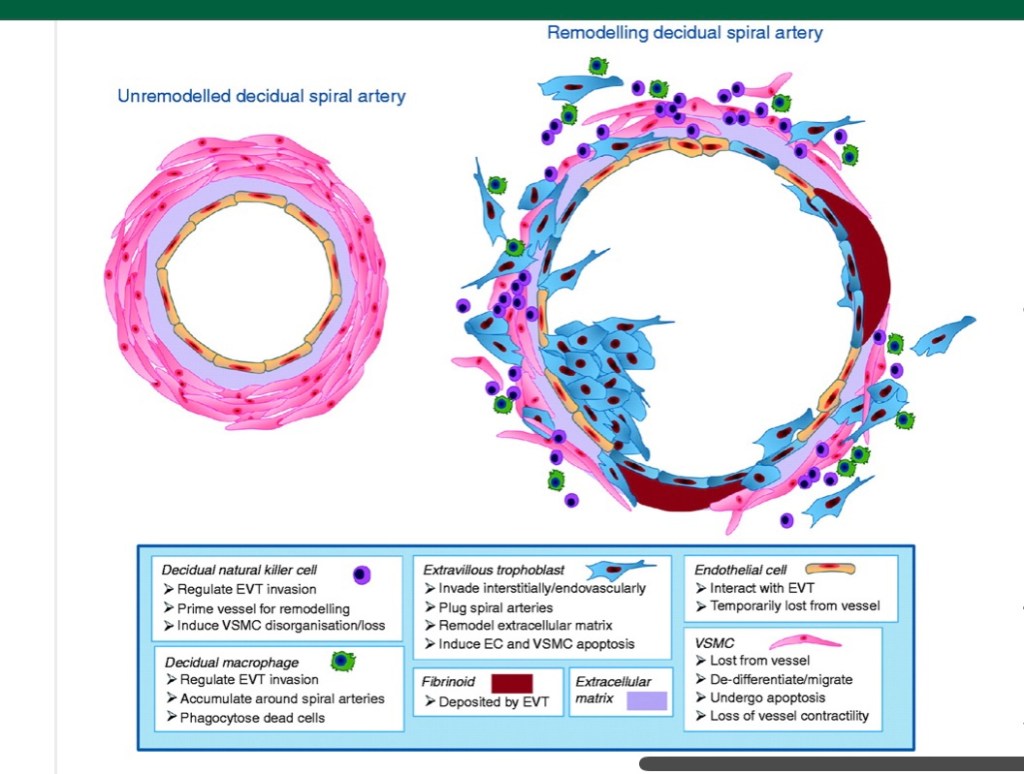



NORMAL AND ABNORMAL TRANSFORMATION OF THE SPIRAL ARTERIES DURING PREGNANCY
The maternal spiral arteries aka “utero-placental” arteries in the decidua (formerly endometrium) are normally transformed into large dilated vessels 2/2 dramatic structural changes in their vessel wall as part of normal pregnancy. The key findings of physiologic transformation are:
1) dilatation of the lumen
2) trophoblast invasion of the vessel wall: media & endothelium
3) replacement of the muscular and elastic tissue of the arterial wall by a thick layer of fibrinoid material.
- These structural changes, esp the destruction of muscle in the media, would likely lead to loss in vasomotor control. Collectively, these changes are thought to maximize delivery of maternal blood to the intervillous space by making the arterial lumen wider and reducing the responsiveness of these vessels to vasoconstrictor agents.
- Failure of maternal spiral arteries to remodel appropriately is the leading theory for etiology of preeclampsia & fetal growth restriction (further discussed in the HTN disorders of pregnancy)
Physiological changes in pregnancy
Physiologic Changes of Pregnancy