Content:
- OB Hemorrhage
- Uterotonics and Hemostasis Devices & Procedures
- Labs/TEG
- TRALI vs TACO

——————————————-
OB HEMORRHAGE
Can happen anywhere: in labor room or triage before delivery, in labor room after delivery, in OR during C/S, in the PACU, on the postpartum maternity floor, in the ED pre or post-partum, in the main OR as a stat case as late as 6 wks postpartum, etc.
On L&D floor, the hemorrhage stages & locations are announced overhead.
OB Hemorrhage has high risk of DIC. If epidural catheter is in place during hemmorhage, leave the catheter in place until labs prove safety of removal. If no neuraxial in place, do not place unless updated labs prove safety (plt > 100, & fibrinogen >300+ at least..)
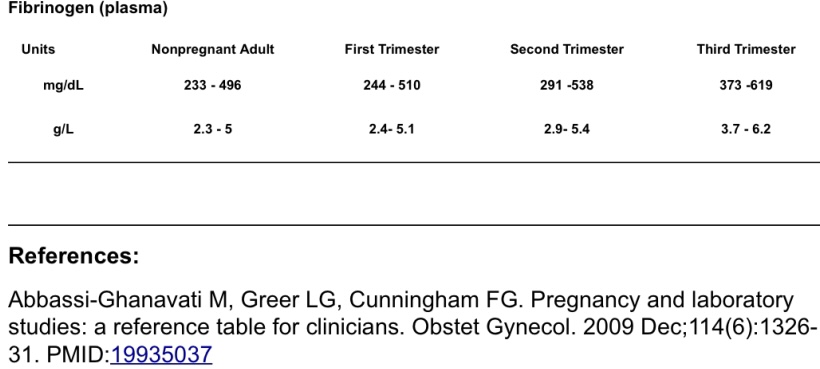
*FIBRINOGEN* IN PREGNANCY
Normal PREGNANT fibrinogen = 350-650 mg/dL**
- Normal non-pregnant fibrinogen value is 200-400 mg/dL
- so a “normal” fibrinogen of ~200 in a PREGNANT patient is ABNORMALLY LOW and suggests DIC!
IMPORTANT POINTS IN OB HEMORRHAGE
- KEEP IN MIND:
- ~40% of postpartum hemorrhage occurs in low-risk women. EVERY woman giving birth is at risk for obstetric hemorrhage (ACOG).
- YOUNG OTHERWISE HEALTHY PTS WILL COMPENSATE IN HEMORRHAGE….UNTIL THEY CANT ANYMORE. TACHYCARDIA or HYPOTENSION IS 2/2 HEMORRHAGE UNTIL PROVEN OTHERWISE, AND REQUIRES CONTINUOUS REASSESSMENT.
- Baroreceptive HR response to hypovolemia can be blunted by BBs (PreE pts) or neuraxial anesthesia for c/s (T4 blockade – cardiac accelerator fibers T4-T1) or just youth and good health! Healthy people can mask hypovelmia pretty well. Unexplained HOTN absent frank tachycardia still DOES NOT rule out hemorrhage. VS often don’t change until ~20 -30% blood volume lost.
- Bleeding can occur for reasons OTHER THAN UTERINE ATONY: eg: vaginal/cervical lacerations, coagulopathy, etc. EXTRAUTERINE BLEEDING INTO ABDOMEN OR RETROPERITONEAL BLEEDING WILL NOT DISPLAY VAGINAL BLEEDING/LOCHIA, AND PERSISTS REGARDLESS OF UTERINE TONE. UTERINE CLOTS CAN ALSO CONCEAL A HEMORRHAGE. “ADEQUATE UTERINE TONE” IS ALSO SUBJECTIVE AND DOES NOT RULE OUT HEMORRHAGE AS CAUSE OF CHANGE IN VITALS.
- Weight-based QBL can by underestimated if ++BLOOD CLOTS present. Clots contain greater concentration of lost RBC/PLT/FACTORS weight-wise than liquid blood ***
HH Anesthesia Guide to Hemorrhage Response
OB MATERNAL HEMORRHAGE: Anesthesia Guide – Link for download:
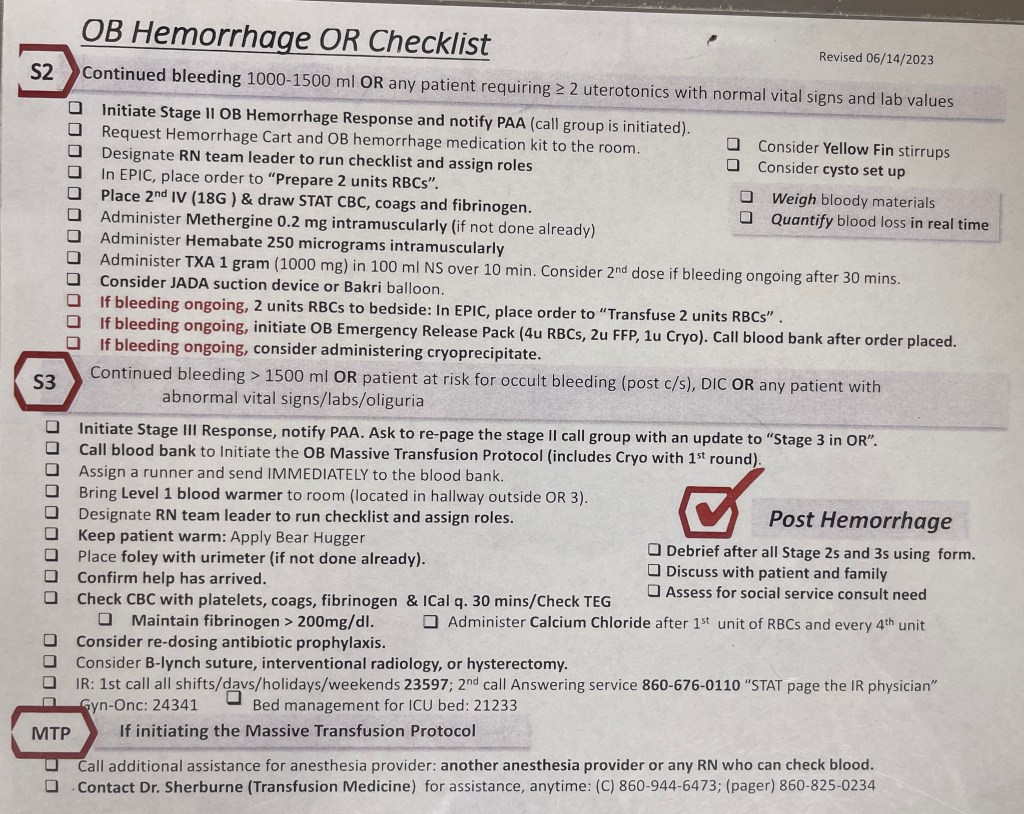
OB Hemorrhage OR checklist: starting with Stage 2
Articles:
Quantitative Blood Loss in Obstetric Hemorrhage
Postpartum hemorrhage: When uterotonics and sutures fail
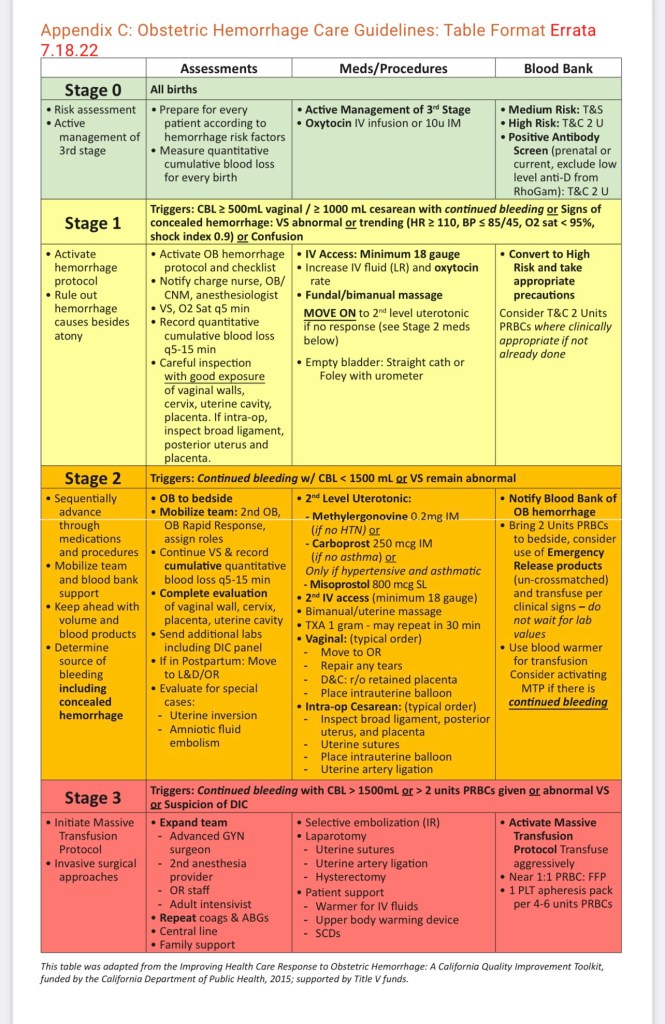
Hemorrhage Stages
Stage 1:
- sometimes more of a formality/heads up & just additional uterotonics given. But can progress RAPIDLY…
Stage 2:
- mobilize team & prepare products for transfusion, assess pt for possibility of HD instability and GA – progressing towards massive hemorrhage.
Stage 3:
- MTP —-> OR, GA (etomidate/ketamine/versed & RSI)… cardiac stable induction
OUT-OF-OR HEMORRHAGE
- If hemorrhage occurs out of OR, it’s announced overhead and anesthesia goes to Stage 2 (to assess pt in case GA needed)
- ANESTHESIA ROLE in Stage 2 OUTSIDE of OR:
- Go to room and ask RN in charge to run the list. (OB Hemorrhage Checklist)
- Once Anesthesia arrives, this is a recap & regroup for everyone to get on the same page as the hemorrhage is progressing.
- In the heat of the moment, the stages are called based on visual EBL, and protocol components get missed.
- RUN. THE. CHECKLIST.
- THEN assess patient: airway/GA concerns in case of emergency
- THEN assist with IV access if needed, ordering blood products, whatever support the team needs. May have to go to OR if severe or for removal of retained placenta.
- Usually, mom is totally awake and alert and “looks fine.” This swarm of people can be overwhelming for her – then we come in and talk about anesthesia, which may really freak her out. Reassure her this is a safety protocol and these are precautions we have to take, regardless of how “ok she looks” or stable she is.
- Once Anesthesia arrives, this is a recap & regroup for everyone to get on the same page as the hemorrhage is progressing.
- Go to room and ask RN in charge to run the list. (OB Hemorrhage Checklist)
- Retained Placenta anesthetic management further down in Uterotonics and hemostasis devices & procedures section.. Can either dose an existing epidural catheter if no HD instability, or spinal, or GA.
- NO sedation in labor room for retained placenta – can dose catheter (chloroprocaine or lido/bicarb) or go to OR for proper anesthetic and airway management
- again, labor pushing = airway swelling
OB HEMORRHAGE CHECKLIST:
1st STEPS IN INTRA-OP HEMORRHAGE MANAGEMENT:
- Get backup if available for extra hands in room.
- Fluids open
- 2nd large bore PIV
- Blood line set up w/ warmer (if in OR)
- *if under GA, lower/turn off sevo, as sevo relaxes uterine smooth muscle & increases bleeding. We usually use 60/40 N2O as well to decrease sevo requirements… OR just switch to TIVA prop gtt with 60/40 N2O/O2 (per FiO2 tolerance)
- Acronym: FITTT : Fluids, IV, Tone, TXA, Transfuse [in reality this is all happening at once]
- Open fluids, get large bore access, uterotonics, txa, blood.
- Once blood transfusing, minimize crystalloid and replace blood loss with blood. Excess crystalloid will contribute to dilutional coagulopathy, third spacing, and higher risk of pulmonary edema.
- Resist urge to add high-dose pressors when hypovolemia from blood loss is the clear cause of instability. Pt needs blood loss replaced with blood products. Pressors will mask volume deficit and worsen acidosis in hypovolemic patient.
First-line Hemorrhage Meds Are Uterotonics
(After 1st IV pit bolus)
1) Pitocin:
- 10u rapid IV bolus over 10 min or 10u IM if no IV access, then 10u intrauterine(by Obgyn).
- SFX: ↓ SVR
2) Methergine: (ergot alkaloid)
- INTRAMUSCULAR* 0.2mg. Aspirate syringe. Cannot go IV => HTN
- Can repeat Q2-4h, max 5 doses. Onset time: 2-5 min, Et1/2 3.4h.
- SFX: HTN crisis –> stroke. Avoid in: HTN/PreE, CAD, cardiomyopathy, protease inhibitors, caution w/ ephedrine use (can exaggerate HTN).
3) Carboprost/hemabate (prostaglandin F2 alpha [PGF2a])
- INTRAMUSCULAR* 0.25mg. Aspirate syringe. Cannot go IV => HOTN
- Can repeat Q15-90min, max dose: 2g.
- SFX: baseline doubles PVR & PAP, diarrhea/vomiting.
- Contraindicated in: asthma (bronchospasm risk), RV strain/failure, pulm HTN, caution in R –> L shunt ASD/PFO/VSD
*TXA stabilizes fibrin clots by inhibiting their breakdown. TXA inhibits conversion of plasminogen to plasmin. Plasmin degrades fibrin clots.
- First dose TXA is 1g over 10 mins
- If continued bleeding, second gram is infused over 8 hrs (can mix in 100-250cc NS)
- TXA should be administered within max 3 hrs of hemorrhage onset, with highest efficacy if administered within 1 hr of hemorrhage onset.
TRANSFUSING OB HEMORRHAGE
Ideally 1:1:1 [RBC] : [FFP] : [PLT + CRYO]
Actual Transfusion:
6 : 6 : 1 : 1 = 6 RBC : 6 FFP : 1 pooledPLTpack + 1 CRYO
RUN ONLY BLOOD & FFP through warmer, NOT PLT/CRYO – hang PLT/CRYO at room temp!
- (1 pooled PLT = 6 packs combined)
- So more like 6 RBC : 6 FFP : 1 pooled PLT pack: 1 cryoprecipitate
- Failure to match CRYO&FFP&PLT (clotting factors) to RBC #s will result in dilutional coagulopathy and worsening hemorrhage.
- CRYO is ESSENTIAL in OB hemorrhage*
- SUPPORT MTP WITH:
- TXA (1g over 10 min), 2nd dose: 1 gram over 8 hrs.
- Calcium
- Warming measures:
- blood/fluid warmer
- DO NOT GIVE PLTs or CRYO THROUGH WARMER – give at room temp.
- bair hugger, increase OR temp
- IV benzo if intrathecal morphine given*
- blood/fluid warmer
- MINIMIZE CRYSTALLOID!! (dilutional coagulopathy, +3rd spacing)
- Antibiotic re-dose every 1500mL transfused or lost
(*BUT WHOLE BLOOD is always best, if available* – WB has > 2x higher Hgb per unit, less anti-coagulant preservatives than component therapy, and no need to match product ratios*)
CRYOPRECIPITATE IS ESSENTIAL IN OB HEMORRHAGE to reduce dilutional coagulopathy and DIC. CRYO provides concentrated essential factors **F8, VWF, Fibrinogen** (more than FFP, as Cryo is pulled off of FFP as it thaws.). MTP parturients are more susceptible to pulmonary edema from fluid overload, especially PreE/HELLP pts as their capillary endothelium is already damaged and leaky from the disease process. *MINIMIZE CRYSTALLOID.*
LARGE BORE IVs NEEDED
HUGE BORE (8.5g) IV INSERTION video (if needed for MTP):
Insertion technique for huge IV – the Rapid Infusion Catheter #shorts
- Just like in traumas, HD instability from hemorrhage is hypovolemia, don’t start high dose pressors when hypovolemic. They lost BLOOD. They need BLOOD products.
- Pressors in under-resuscitated patients only increases acidosis
- Give TXA early on (so all clotting factors given in FFP, PLT, and CRYO to produce final fibrin clots aren’t broken down by plasmin)
- CRYO is key in MTP: it’s pulled off FFP as it thaws – 10x as many clotting factors as FFP, super concentrated factors without all the volume. Volume overload can cause T.A.C.O and pulmonary edema
- Cryo has specifically high F8, VWF, Fibrinogen**, while FFP has high F2, 5, 7, 9, 10, 11
- Hemorrhage can rapidly progress to requiring MTP.
- We have an OB HEMORRHAGE PACK that *RN can also order!! It’s ready to go in blood bank 24/7.(Prior to full MTP) you’ll be busy enough when this is needed – delegate this order set!!!
- Calcium to support coagulation cascade and stabilize myocardial membranes in setting of hyperkalemia 2/2 acidosis and RBC Transfusion
- Re-dose Ancef after 1500mL blood loss (same as traumas)
- Fibrinogen concentrate: if available at HH (?) expensive product, but it’s similar to cryoprecipitate in that it has very high fibrinogen concentrations with minimal volume, to avoid volume overload.
- Intrathecal morphine can dramatically decrease basal temp through CNS dysregulation, which is non-responsive to traditional warming measures. BENZO reverses this (2mg midazolam or 0.5mg ativan – midaz may need re-dose due to short ET1/2 compaed to IT morphine)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8015778/
https://www.perinatology.com/Reference/OBPharmacopoeia-Public/Postpartum%20hemorrhage.htm
^^ nicely formatted, easy to read CMQCC checklist summary
Balancing Recuscitation vs Volume Overload & Pulmonary Edema vs TACO vs TRALI
- Pulmonary edema mamagement in “PULMONARY EDEMA IN PREGNANCY” page
- Lasix consideration for volume overload: NORMAL Pregnant pts at higher risk of pulm edema 2/2 decreased plasma colloid osmotic pressure and increased hydrostatic pressure 2/2 normal plasma volume (~50%) increases of pregnancy.
- Many conditions placing pts at higher risk of uterine atony/hemorrhage ALSO place pts at higher risk of pulm edema:
- So patients you’re more likely to be transfusing are also more vulnerable to pulmonary edema and fluid overload, including:
- PreE/HELLP hemorrhage 2/2 consumption of clotting factors & liver damage
- terbutaline (uterine relaxant = increased bleeding risk) 2/2 fetal intolerance of contractions (can be seen in PreE 2/2 insufficient maternoplacental vasculature) Terbuatline is also independent risk factor for pulmonary edema likely 2/2 increased hydrostatic pressure from inotropy of beta2 agonism.
- MAG gtt for eclamptic seizure prevention in preE /HELLP (also relaxes uterus)
- …ALSO all further increase alveolar-capillary membrane permeability (PreE 2/2 endothelial damage, Mag is independent risk factor for pulm edema: theory is 2/2 direct cardiac depression or direct capillary damage)
- So pregnant pts with conditions that make them already more likely to hemorrhage (preE, HELLP) are also likely to have meds on board/physiology that put them at even higher risk of pulmonary edema with volume overload. (even higher risk than normal pregnancy, which is much higher risk than non-pregnant. Oy!)
- So patients you’re more likely to be transfusing are also more vulnerable to pulmonary edema and fluid overload, including:
- Many conditions placing pts at higher risk of uterine atony/hemorrhage ALSO place pts at higher risk of pulm edema:
May need to convert to GA:
- Careful airway management. You have multiple people in the room to help you position as best as you can beneath drapes prior to induction. Preoxygenate as much as possible.
- Careful w/ induction in hypovolemic pt – Etomidate may be better induction agent. Vent PPV may drop BP further via decreased preload in severe HD compromise.
- After delivery: fent, versed, & N2O and ketamine can facilitate lower sevo %, or just full TIVA with prop/fent/ketamine/versed is ideal.
- GA for C/S described in seperate page
> LETHAL TRIAD <
hypothermia, acidosis, & coagulopathy
Hypothermia & acidosis decrease thrombin generation & fibrinogen availability
Thrombin generation:
- Hypothermia inhibits the initiation phase
- Acidosis severely inhibits the propagation phase.
Coagulopathy by Hypothermia and Acidosis: Mechanisms of Thro…
Fibrinogen Availability:
- Hypothermia & Acidosis affect fibrinogen metabolism.
- Hypothermia inhibits fibrinogen synthesis
- Acidosis accelerates fibrinogen degradation. *Coagulopathy 2/2 acidosis cannot be immediately corrected by pH neutralization alone.
- Limit crystalloid to avoid hemodilutional coagulopathy
- Pressors in hypovolemia will only cause worsening metabolic acidosis —> further worsening coagulopathy.
- ROOM TEMP can be turned up if pt hypothermic. And always fluid warmer. hypothermia—> further worsens coagulopathy.
- TXA inhibits fibrin degradation
- CALCIUM to support coagulation cascade and maintain cardiac myocyte membrane stability
- CRYO has highest fibrinogen concentration.
- Fibrinogen concentrate (if available) same idea as cryo for maximum fibrinogen and minimal volume to avoid overload
- Lasix to manage volume overload
IF PT RECEIVED INTRATHECAL MORPHINE IN SPINAL PRIOR TO HEMORRHAGE AND IS HYPOTHERMIC – GIVE BENZODIAZEPINE TO REVERSE HYPOTHERMIA (0.5-1mg ativan/lorazepam OR 2mg midazolam and re-dose as needed. Intrathecal* morphine can impair CNS thermoregulation and can cause intractable, profound hypothermia non-responsive to traditional warming measures!! Benzo reverses this within minutes. This is unique to IT morphine*
OB HEMORRHAGE CONSIDERATIONS:
Can progress to DIC via consumption of all clotting factors. Draw and send cbc & coags to assess h/h, INR & fibrinogen levels. TEG can be drawn to assess speed, strength, and stability of clot formation and breakdown.
- If epidural catheter is in place, do not remove until coags & PLT are stable. Can be left in place for days if necessary.
- Massive hemorrhage code is commonly a PEA arrest: CPR and Epi. Hemorrhage usually happens after placenta delivered, so uterine displacement not as critical considering uterus less gravid compressing great vessels.
CAUSES OF HEMORRHAGE:
4 Ts : Tone, Trauma, Tissue, Thrombin
- Tone: Uterine Atony (70%)
- Trauma: Lacerations (20%)
- Tissue: Retained placental tissue/ invasive placenta (accreta spectrum)(10%)
- Thrombin: coagulopathies: thrombocytopenia, coag/factor disorder, preE/HELLP, (1%)
INCREASED RISK OF ATONY: (70% of hemorrhages)
- GA
- uterine overdistention (twins or polyhydramnios)
- prolonged labor, oxytocin use during labor (decreased receptor responsiveness)
- uterine leiomyomas
- operative delivery and intrauterine manipulation
- previous hemorrhage in the third stage of labor
- uterine infection** Chorioamnionitis
- extravasation of blood into the myometrium (Couvelaire uterus)
- intrinsic myometrial dysfunction.
- use of tocolytics: MgSO4-, terbutaline
HEMORRHAGE FROM TISSUE (Placental) ABNORMALITIES:
- Accretas
- Previas
- Abruption
- Retained Placentas – if there’s any issue taking placenta out, leave the epidural catheter in so it can be re-dosed if an OR take-back is necessary.
HEMORRHAGE FROM TRAUMA (Lacerations):
- Postpartum hemorrhages can also be from cervical lacerations.
- Cervical lacerations bleed like crazy as its highly vascularized with no smooth muscle to clamp the blood vessels down.
- Any cervical tumor, ectopic pregnancy implanted in the cervix, case involvement requiring cervical surgical instrumentation – will be a potentially HIGH BLOOD LOSS case.
- Excessive bleeding from episiotomy or lacerations in uterus, cervix, vagina, and vulva can result from precipitous or uncontrolled delivery, or operative delivery of large infant. Can also occur after delivery.
Quick Tocolytic review:
BETA-2 AGONISTS (Terbutaline)
- (Ritodrine only FDA approved med in this class, but not available in US). So terbutaline is used. B agonists relax smooth muscle (myometrium.) Bindis receptor ^^^ intracellular CAMP —> activates protein kinase —>inactivates myosin light-chain kinase,—>decreases myometrium contractility.
- Side effects: Tachycardia, HOTN, palpitations, SOB, chest pain, *pulmonary edema* hypOK+, hypERglycemia. Contraindications include tachycardia-sensitive maternal cardiac conditions (AS/MS/HOCM, WPW, SVT, etc.)
- *Terbutaline (1mg/mL vial) can also be used for refractory bronchospasm as bronchodilator.
- SUBQ dose (0.25 pedi, 0.5mg adult). – or can give 0.5mg aerosolized down ETT (less reliable uptake)
- *Terbutaline (1mg/mL vial) can also be used for refractory bronchospasm as bronchodilator.
MAGNESIUM SULFATE
- Given for maternal seizure prophylaxis in PreE/Eclampsia/HELLP and for fetal neuroprotection in pre-term delivries
- NOT as anti-HTN med, NOT as tocolytic, but has uterine relaxant effect.
- MOA unclear, probably decreases availability of Ca2+ by blocking membrane & intracellular Ca2+ channels, decreasing contractility.
- NOT as anti-HTN med, NOT as tocolytic, but has uterine relaxant effect.
- Side effects: HOTN, can potentiate all NMBDs, pulmonary edema, nausea, flushing, headache, lethargy. Myasthenia Gravis is a contraindication to the use of mag sulfate.
- Mag has toxicity: (*Tx Ca++ Gluconate). If a woman HAS REFLEXES (DTR) there is no lethal mag level yet. If pt has cardiac/resp arrest with intact DTRs – arrest must be attributed to something else.
- reduction of DTR assc w/ resp depression, but LOSS of DTR comes right before resp ARREST(resp paralysis)—> cardiac arrest
- Mag gtt for PreE continues running through c/s. Mag also given in preterm deliveries for fetal neuroprotection (from cerebral palsy) as bolus dose – does not run through c/s
- Mag & corticosteroids for preterm are risk factors for maternal pulm edema
- Pre-term uterus also has lower response to oxytocin, may need methergine as 1st line.
- Mag & corticosteroids for preterm are risk factors for maternal pulm edema
Obstetric critical care podcast:
Massive Transfusion and the Lethal Triad
The Hemodynamics of Hemorrhage
Episode 159: Postpartum hemorrhage with Juanita Henao
Acute Postpartum Hemorrhage – StatPearls – NCBI Bookshelf
REVIEW OF UTEROTONICS
~ and hemostasis devices & procedures ~
- Different uterotonics each work on different receptors to cause uterine smooth muscle contraction.
- Pitocin is IV, while methergine & hemabate are always IM. Aspirate the IM needle to make sure it doesn’t go IV —> severe hemodynamic reactions.
PITOCIN
synthetic oxytocin
- Increased Na+ permeability of uterine myofibrils —> indirectly stimulates contraction of uterine smooth muscle
- GPCR stimulation —> release of IP3—> activation of volt.gated Ca2+ channels —> Ca2+ influx —> depolarization of muscle fibers (uterine contraction)
- Mammary-alveoli-myoepithelail cells —> contraction-milk ejection
- Oxytcin causes vascular smooth muscle dilation –> transient SVR drop with high doses. (post-delivery IV pit bolus)
- Increased uterine response to oxytocin with increased duration of pregnancy.
- Response increases with up-regulation of oxytocin receptor density and sensitivity from 20-30wks, reaches plateau at 34 wks, then becomes even more responsive during labor.
- Very pre-term uterus < 34wks or 2nd TM abortion may have decreased response to pitocin –> methergine may be 1st line uterotonic.
- Esp a very pre-term c/s: less natural oxytocin receptor up-regulation has happened, AND pt has not been in labor yet to up-regulate those receptors.
- If pre-term delivery 2/2 severe PreE/HELLP/HTN d/o, methergine is contraindicated.
- Esp a very pre-term c/s: less natural oxytocin receptor up-regulation has happened, AND pt has not been in labor yet to up-regulate those receptors.
ACOG 2nd TM abortion: clinical practice guidelines for hemorrhage in pre-term uterus:
Mechanical Stretch Up-Regulates the Human Oxytocin Receptor in Primary Human Uterine Myocytes
I.M. Methylergonovine maleate
“METHERGINE”
DOSE:
- 0.2mg (200mcg) I.M. or I.U.
- Can be continued as a series: 200mcg IM x 4 additional doses Q6hrs
- Given IM to prevent severe HTN with IV administration
MOA:
- Maleate salt of methylergonovine, a semisynthetic ergot alkaloid w/ vasoconstrictive & uterotonic effects.
- Methylergonovine:
- STIMULATES: serotonergic, dopaminergic, and adrenoreceptors
- INHIBITS: the release of endothelial-derived relaxation factor –> arterial vasoconstriction & increased uterine smooth muscle cxns.
CONSIDERATIONS:
- CONTRAINDICATED IN CARDIAC PTS and uncontrolled HTN (preE, HELLP, eclampsia), as well as Pulm HTN, significant cardiomyopathy, etc.
- (gHTN, cHTN are gray areas) If massive hemorrhage though in any circumstance, you can probably still give methergine if really needed, as they’d likely be hypotensive in hemorrhage anyway. BUT instead of full (0.2mg/200mcg) IM, can instead dilute dose in 20cc saline = 10 mcg/cc and give in small, slow, controlled IV pushes to effect – can always treat HTN with IV meds)
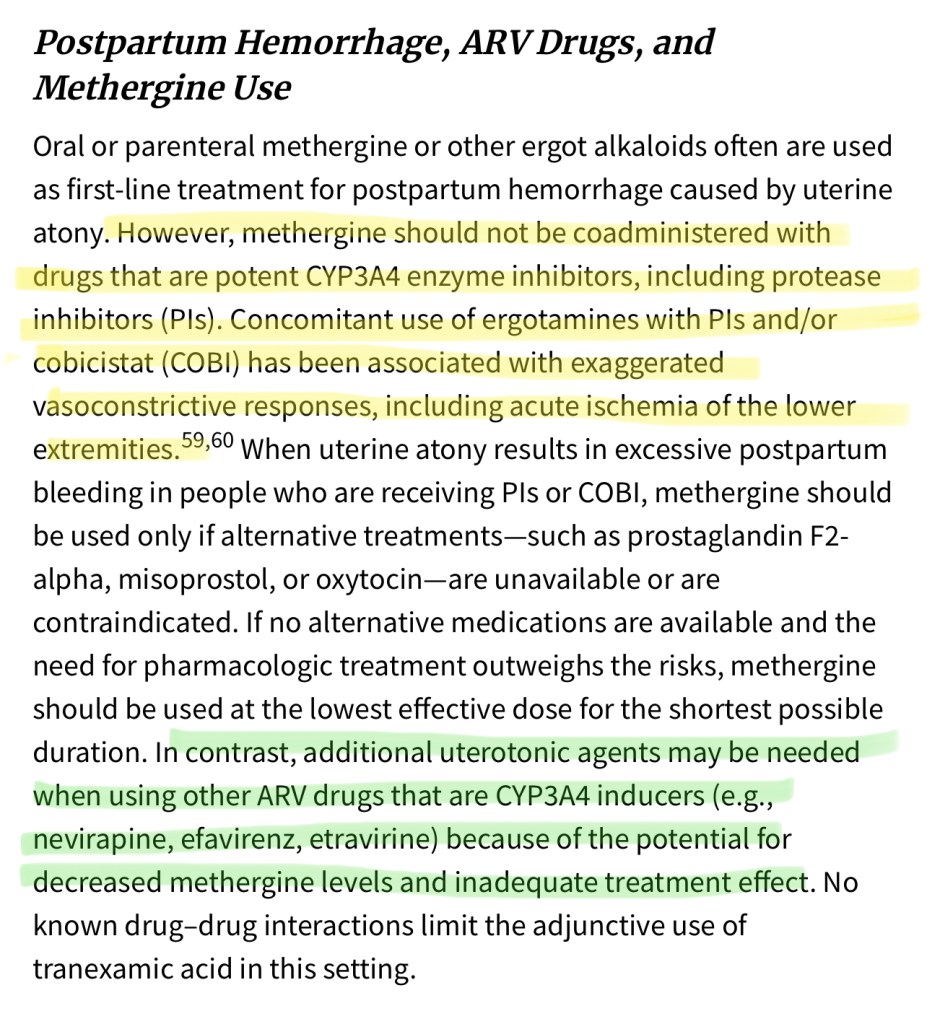
- Methergine contraindicated in HIV+ pts on Protease inhibitors [“-avir“] (HTN crisis 2/2 CYP3A4 inhibition –> disruption in methergine metabolism and exaggerated vasoconstrictive response)
- Side note: Fentanyl metabolism reduced by CYP3A4 inhibitors (eg: protease inhibitors) as well, but in the small *neuraxially administered doses we use for spinal or epidural anesthesia (2mcg/cc epidural pump solution, 100mcg epidural bolus for pressure or c/s conversion, 10-20mcg intrathecal for spinal) are not likely to have any real respiratory consequence.
- Methergine contraindicated in HIV+ pts on Protease inhibitors [“-avir“] (HTN crisis 2/2 CYP3A4 inhibition –> disruption in methergine metabolism and exaggerated vasoconstrictive response)
- (gHTN, cHTN are gray areas) If massive hemorrhage though in any circumstance, you can probably still give methergine if really needed, as they’d likely be hypotensive in hemorrhage anyway. BUT instead of full (0.2mg/200mcg) IM, can instead dilute dose in 20cc saline = 10 mcg/cc and give in small, slow, controlled IV pushes to effect – can always treat HTN with IV meds)
METHYLERGONOVINE MALEATE AND THE RISK OF MYOCARDIAL ISCHEMIA AND INFARCTION
Intr apartum Care for People with HIV | NIH
I.M. CARBOPROST
“Hemabate”
DOSE:
- 0.25 mg (250 mcg) I.M or I.U
- Can repeat dose Q 15 min x 8 doses for max total dose of 2mg
- Given IM/IU to prevent severe hypOtension if IV
- 2/2 systemic vasodilation from prostaglandin receptor on vascular smooth muscle
MOA:
- Synthetic prostaglandin E2 (prostaglandins occur naturally in body and act at several sites, including the uterus)
- mimics PGF2-alpha, and binds E2/F prostaglandin receptor, which causes myometrial contractions, induces labor, & expels the placenta.
- Smooth muscle on GI tract activation —> nausea/vomiting, diarrhea
- (Glycopyrrolate can help to block ACh in GI smooth muscle, as well as the usual antiemetics: zofran, decadron, benadryl 12.5mg, prochlorperazine or haloperidol 0.5mg are great too! OB will usually Rx immodium or something to help with diarrhea)
- Can also cause flushing and temp rise ~ 2o
- CONTRAINDICATED IN ASTHMA, pulm HTN, Cardiomyopathy, RV dysfunction, ASD/VSD, etc (resolved childhood asthma is fine – I mean diagnosed adult asthma)
- Hemabate should be avoided in cardiomyopathy pt, RV dysfunction, PFO, & pulmonary HTN
- Hemabate/carboprost increases PVR IF BRONCHOSPASM, CAN INCREASE PVR BY 100%, AND PAP BY 125%!!.. HUGE problem in pulm HTN, VSD/ASD/cardiomyopathy, RV dysfunction, etc..
- Right heart can’t tolerate any more strain from increased afterload. Can cause bronchospasm: esp in asthmatics, which would be catastrophic in right heart strain/failure/cyanotic shunt.
- PGD2 is potent broncoconstrictor:
- myocontraction from thromboxane receptor on bronchial smooth muscle (broncoconstriction) –> HPV reflex –> pulmonary vasoconstriction
- PGD2 is potent broncoconstrictor:
HEMABATE® (carboprost tromethamine) Adverse Reactions
Rectal or Buccal: MISOPROSTOL
“Cytotec“
DOSE:
- Come as pills that can be given buccal (800mcg) or rectally-inserted by OBGYN (1000mcg).
MOA:
- Prostaglandin E1 analogue that causes cervical softening and dilation, and uterine contractions.
- Slower onset of action, not for emergent hemorrhage, but given as additional med to maintain uterine tone postpartum.
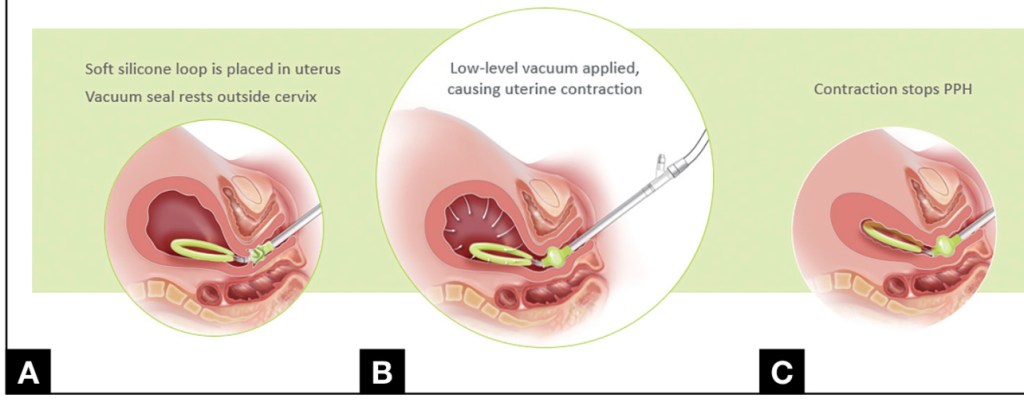
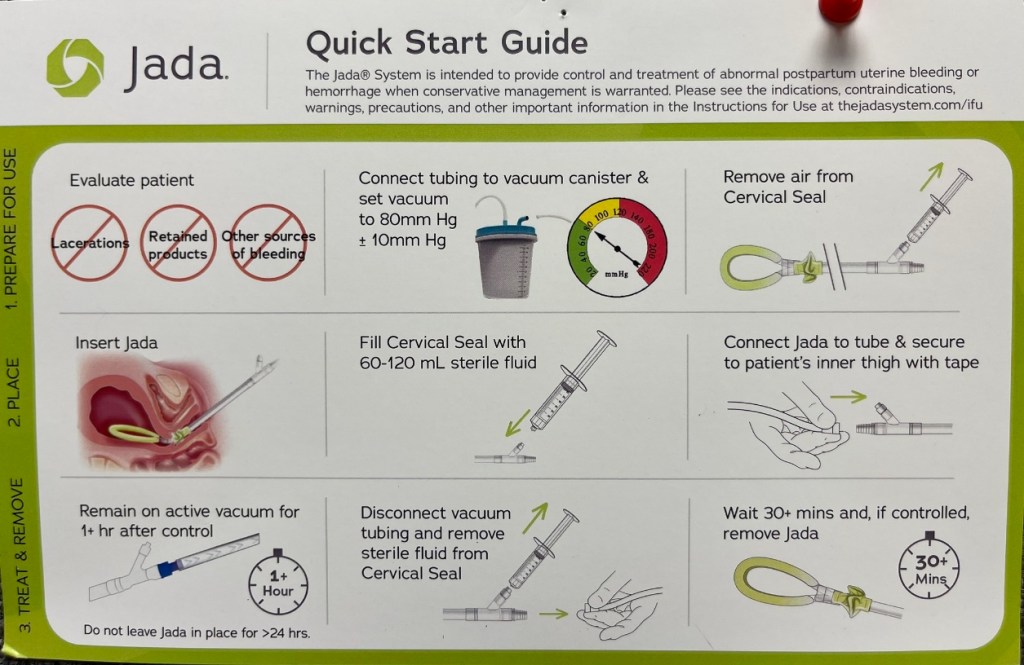
NEW: JADA Device
Inserted into uterus – can be considered a post-partum “uterotonic” for ATONY
- Not for non-atony sources of bleeding: not for retained products, lacerations , or non-atonic sources of bleeding
- Can be inserted emergently, or non-emergently.
- Considered another uterotonic as it continuously applies vacuum to suction the uterus down & contract it/clamp down the uterine vasculature.
- Can be used prophylactically in pts who the OBGYN feels may be at a higher risk of bleeding postpartum.
- Also great for pts w contraindications to 2nd line IM uterotonics Methergine (HTN/CV dx) and Hemabate (asthma, RV dysfunction/pulm HTN)
JADA website with videos:
Postpartum Hemorrhage Control | The Jada® System
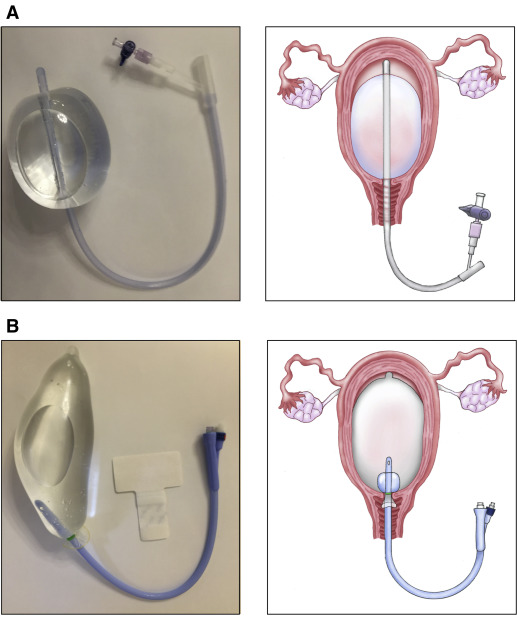
BAKRI BALLOON
Emergent Uterine Tamponade Device
- Bakri intra-uterine tamponade balloon was previously the only intra-uterine emergent hemorrhage device, but the JADA is new and having great results.
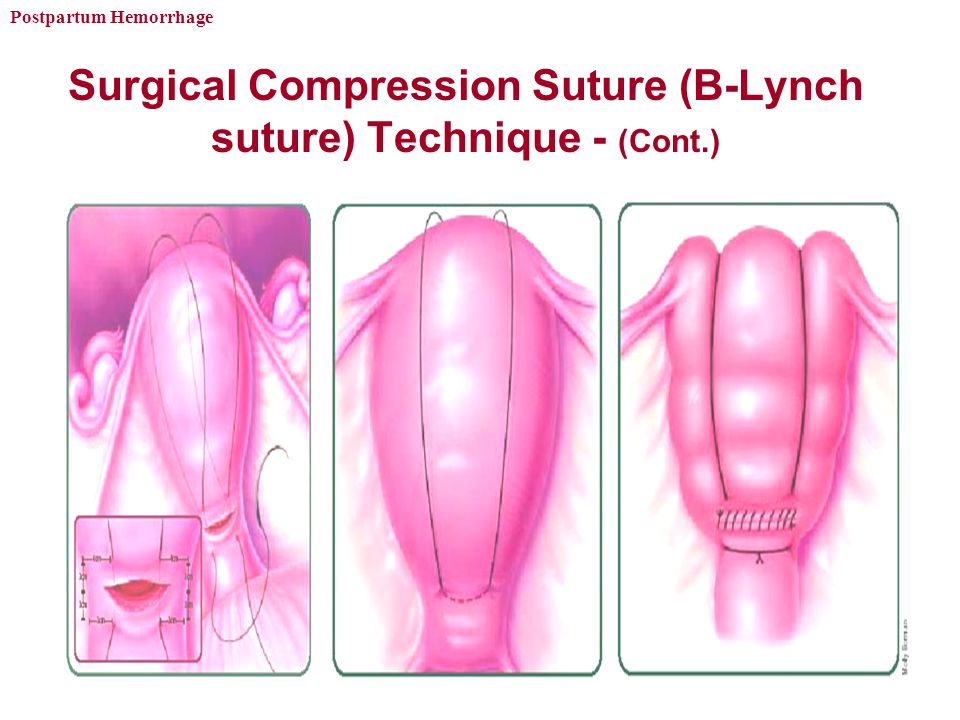
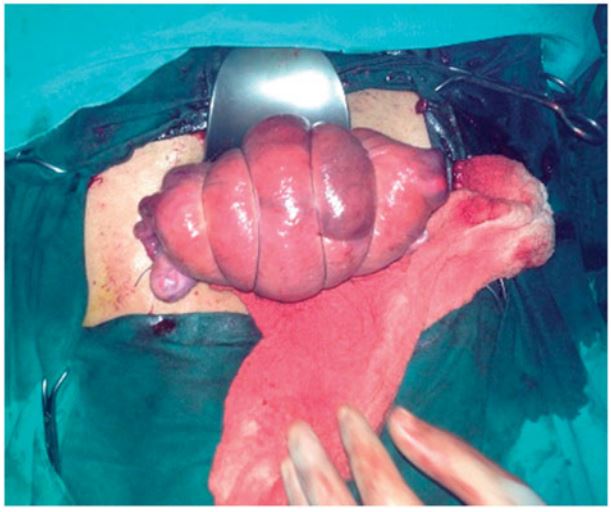
B-LYNCH COMPRESSION SUTURE
for intractable hemorrhage
UTERINE ARTERY EMBOLIZATION
Interventional Radiology
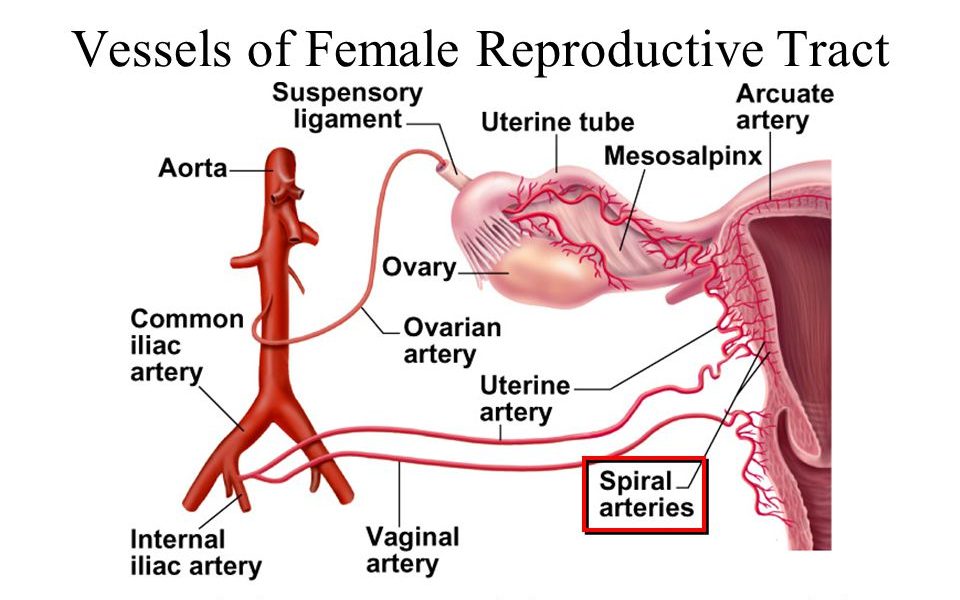
UTERINE VASCULAR ANATOMY:
- Uterine arteries branch off the internal iliacs (whereas ovarian arteries branch off the aorta)
- Uterine arteries can be embolized in IR (usually elective for uterine fibroids) but also to stop hemorrhage.
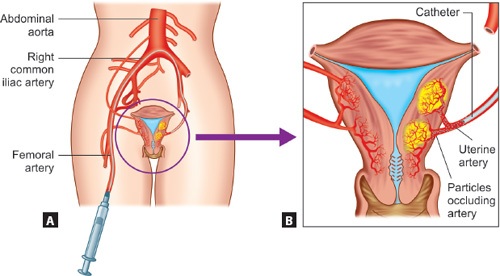
Case study of parturient who needed TWO rounds of UAE (uterine. art. embolization) after hemorrhage and DIC:
Pt OB hemorrhage —> UAE —> hemostasis —> DIC —> 2nd hemorrhage —>2nd UAE —> hemostasis
O.R. take-back for Retained Placenta
- Check H/H. Retained placenta problematic bc uterus can’t contract down fully, so it continues bleeding. Check EBL. Watch for HOTN on induction/epidural dosing. May need blood products.
- Sometimes these are pts who have +++ bleeding, but sometimes totally stable, but unable to tolerate the US-visualized retained placenta manual extraction (ouch) in the labor room without anesthesia (either no epidural in place or epidural failed)
IV NITROGLYCERIN
- ~100mcg IV can be used to rapidly and briefly relax uterus for retained placenta extraction
- (or difficult fetal extraction, or relaxation during ECV)
- Caution in hypovolemic/HOTN patient – chase immediately with ~10mg ephedrine & 100-200mcg phenylephrine.
ANESTHETIC MANAGEMENT of retained placenta:
- Usually a quick procedure < 10min. OBGYN will manually reach into uterus under ultrasound and pull out any retained products.
- If they still have epidural, just dose it to pt tolerance – watch for sympathectomy in hypovolemic pt…manage with pressor pushes or blood products/fluids if ++EBL
- Ideally we dose epidural or do lower-dose spinal (~7.5-10mg should be OK)- lateral spinal option too. Depends on severity of situation/hemodynamics of pt.
- No spinal in hypovolemic/high blood loss pt – won’t tolerate sympathectomy
- GETA: RSI with etomidate
- No spinal in hypovolemic/high blood loss pt – won’t tolerate sympathectomy
- IF GA NEEDED:
- Still considered full stomach for at least 48-72h postpartum*
- RSI w/ full prophylaxis w/ Bicitra & Reglan is still warranted.
- If ANY continued acid reflux past 48h —> continue to perform RSI w/prophylaxis for procedures/surgery.
- Still swollen airway tissues
- Ketamine & versed sedation maintain airway reflexes & spontaneous ventilation in setting of no epidural & bad airway – clinical judgement*
- Make sure this pt gets Metocloprimide (Reglan) to tighten LES and help empty stomach**
- Pt goes into lithotomy for procedure – if BP soft, watch for another BP drop at end of procedure when pt comes out of lithotomy.
If under GA:
- There is no longer a fetus to consider.
- Shouldn’t need to re-paralyze for most cases. Soft bite block/oral airway in place if not re-paralyzing to prevent NPPE if they bite tube
- Propofol TIVA better than sevo for mom to minimize bleeding 2/2 sevo-mediated uterine smooth muscle relaxation.
- GA maintenance w: Prop/N2O/fent ideal. Versed is great* ketamine also great*
- Less than 1/2 Mac sevo 0.7/0.8 OK with the added N2O- if persistent bleeding/atony, switch to prop gtt with N2O/O2 60/40, + ketamine for HD stable anesthetic.
————————
LABS in Hemorrhage
- iStat – CBC, CHEM, ABG
- DRAW: Coags: PT/PTT/INR/FIBRINOGEN, & TEG
Coagulation changes in pregnancy
Normal pregnancy fibrinogen: 350-650.
Levels lower than this in a bleeding OB pt suggest DIC

Fibrinogen for the management of critical obstetric hemorrhage
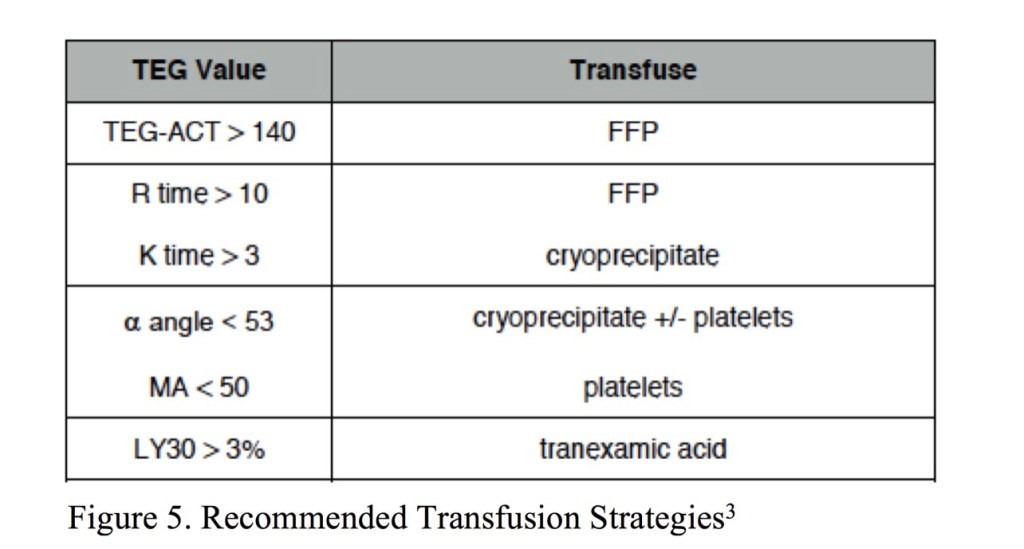
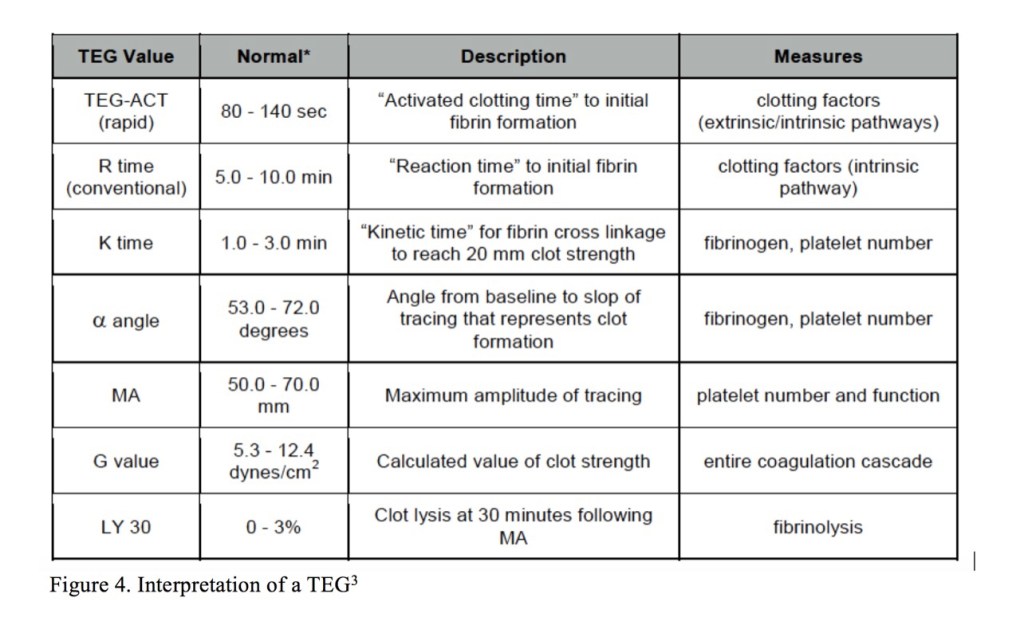
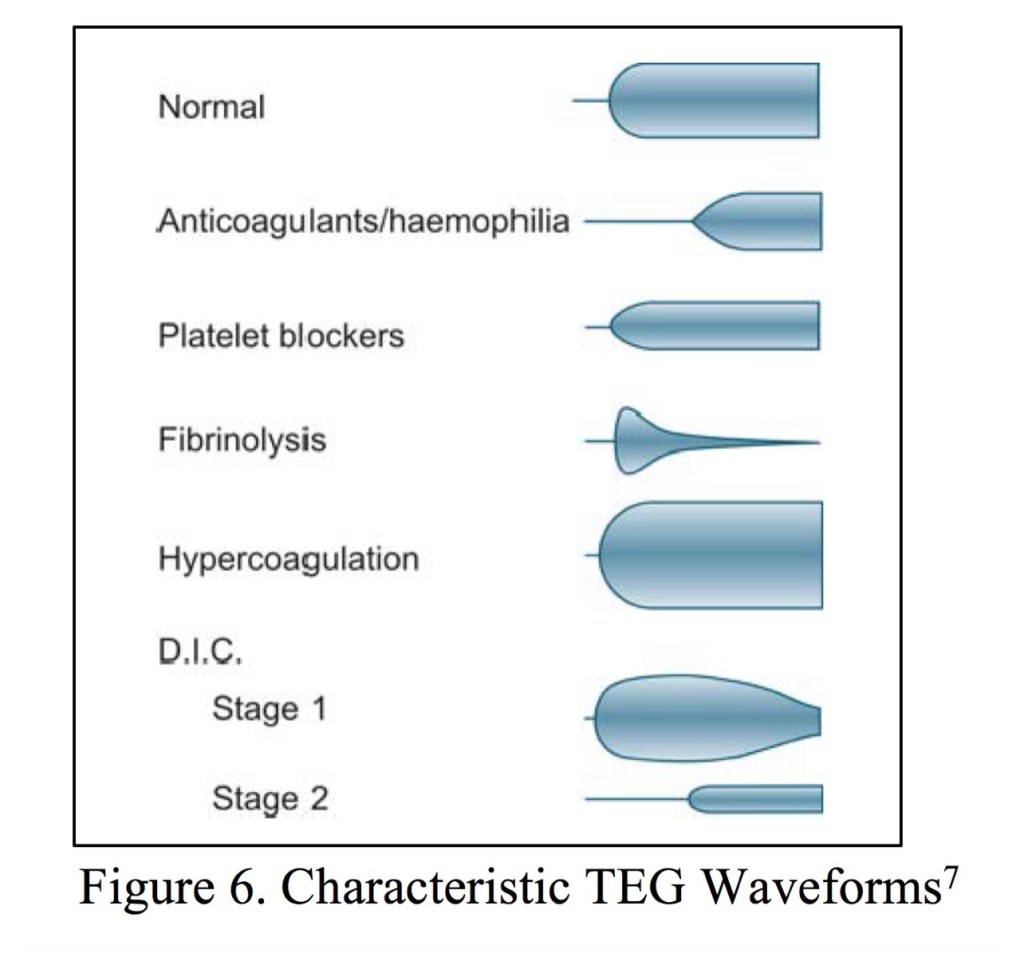
TEG
THROMBOELASTOGRAM
- Useful in guiding resuscitation in severe hemorrhage/MTP/DIC
- Useful in cases where thrombocytopenia is complicated by liver dysfunction, other coagulopathy, or pseudothrombocytopenia.
- Useful to determine DIC progression, recovery, and appropriateness of neuraxial interventions or catheter removal.

——————————————
TACO vs TRALI:
———————-
- TACO = pulmonary hydrostatic (cardiogenic) edema
- TRALI = pulmonary permeability edema (noncardiogenic).
- The pathophysiology of both syndromes is complex & incompletely understood.

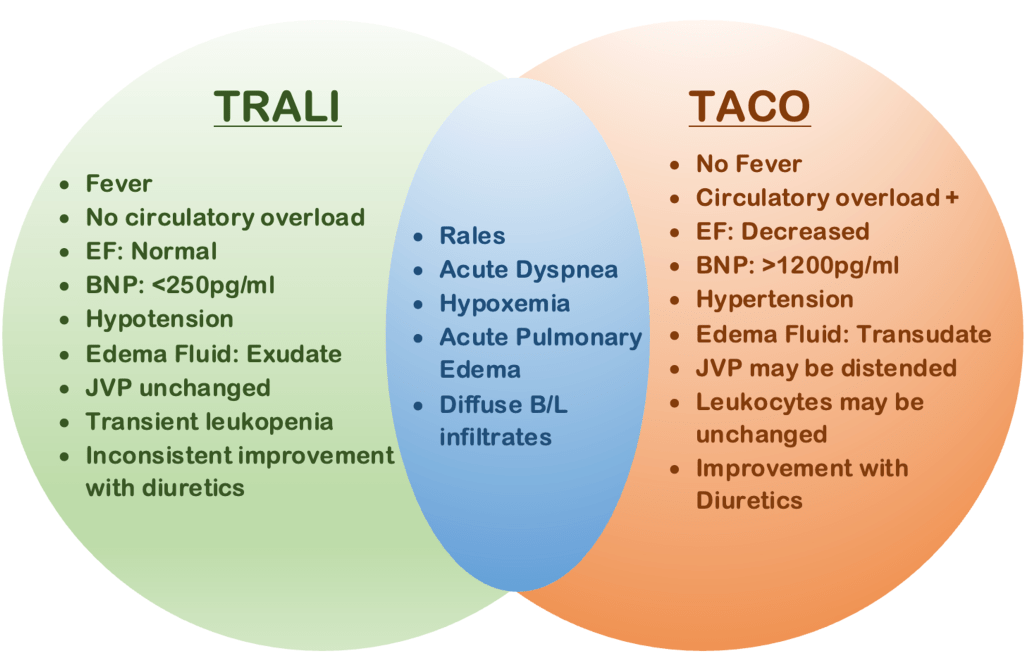
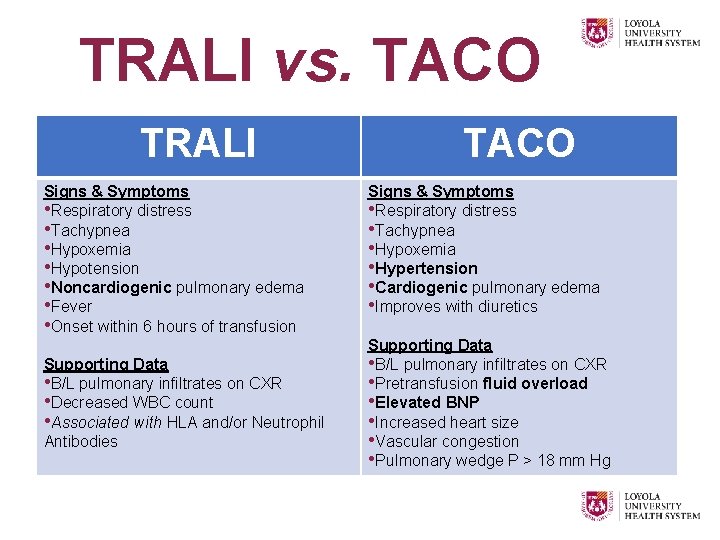
Transfusion-associated circulatory overload and transfusion-related acute lung injury