CONTENTS:
- Nerve injury vs delayed recovery
- Epidural hematoma signs/symptoms
- PDPH & Epidural Blood Patch
- There’s a difference between sensation never fully returning, and sensation returning – then receding again.
- The latter should set off alarm bells.
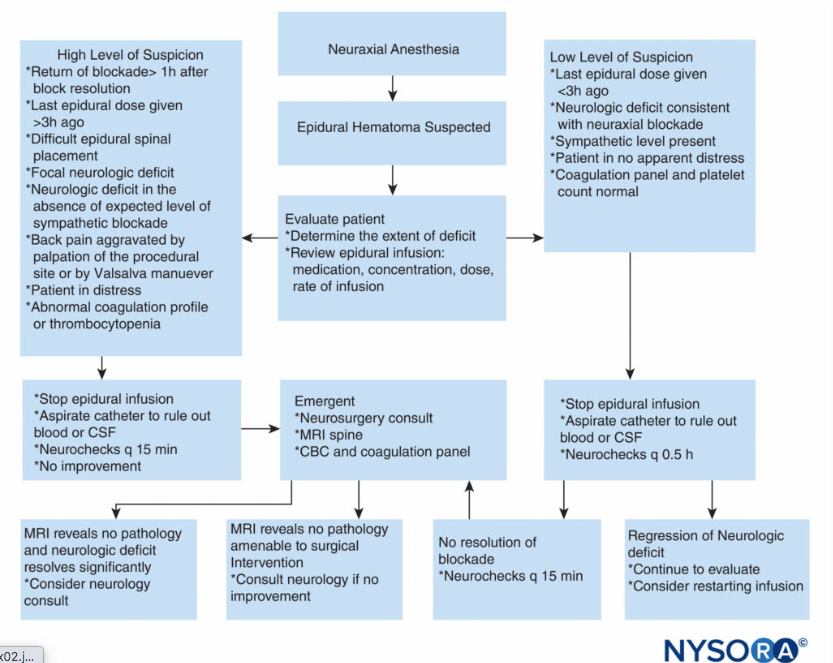
SUSPECTED EPIDURAL/SPINAL HEMATOMA NEEDS A STAT MRI
NYSORA pages on Spinal/Epidural Hematomas SUMMARIZED in pdf:
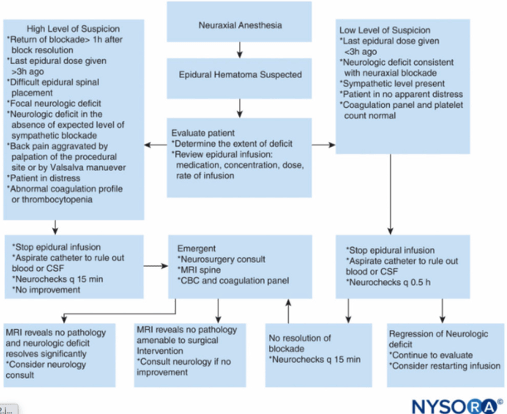
HEMATOMA WORKUP QUICK SHEET:
SENSORIMOTOR ASSESSMENT:
- Determine delayed recovery of select dermatomes vs recovery followed by return of sensorimotor loss/NEW ONSET of s/s: NEW onset numbness, NEW onset motor loss –> STAT MRI
- Pt on blood thinners? Higher index of suspicion for hematoma
- Isolated dermatomes sensory deficit that never recovered – likely delayed recovery – was block one-sided? (more common w/ heavy top-offs) – reassure pt it should continue to improve, but if worsens, alert anesthesia immediately.
- new or worsening sensorimotor loss? –> STAT MRI
- Motor involvement? – further workup: new motor deficit (esp if + back pain) –> STAT MRI
- Motor involvement? – further workup: new motor deficit (esp if + back pain) –> STAT MRI
- Loss of bowel and bladder control? –> STAT MRI
- New/progressive sensorimotor loss w/ back pain: Does it radiate down leg(s)? Unilateral or bilateral? –> STAT MRI
- Isolated back pain/radicular pain without sensorimotor loss – neuro consult.
- Foot drop? Assess for CPN injury from stirrups, if used.
- Just soreness over/around site? – Check for infection/inflammation at site. Soreness is normal.
- Thoracic back pain/soreness? If muscular in nature soreness/strain? – likely 2/2 labor.
- Tx: Can use NSAIDS+/-Flexeril (cyclobenzaprine) 5mg. NO diazepam/valium in breastfeeding.
- 5mg just as effective as 10mg for muscle relaxation, but without the CNS effects ++drowsiness of 10mg**
- Tx: Can use NSAIDS+/-Flexeril (cyclobenzaprine) 5mg. NO diazepam/valium in breastfeeding.
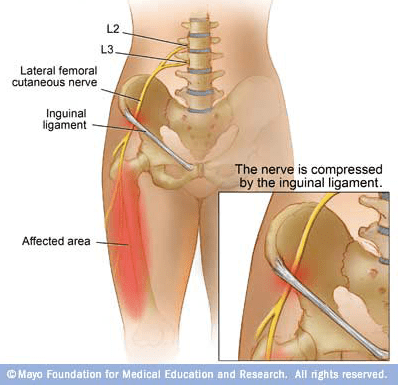
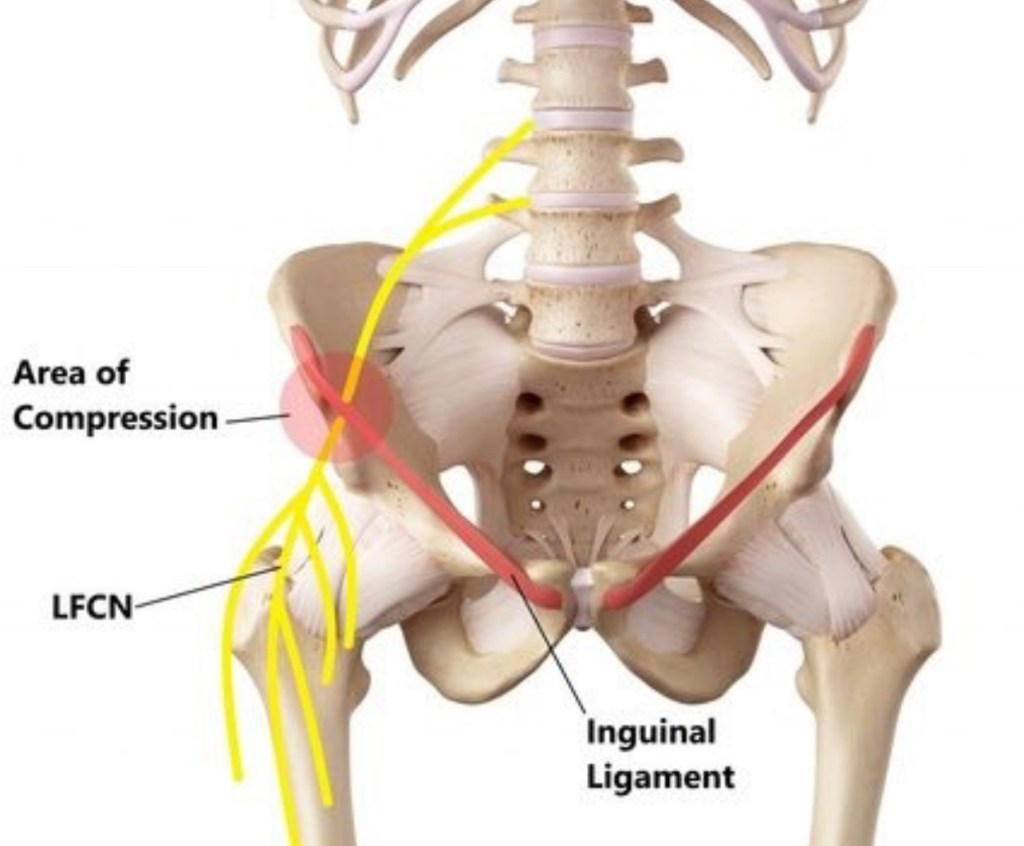
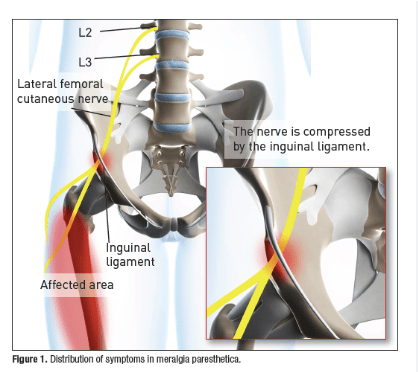
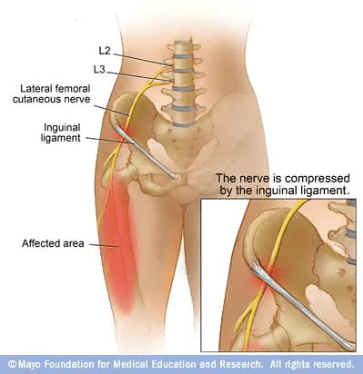
- Burning leg pain: Meralgia Paresthetica?
- Injury from pushing: LCFN (sensory only) entrapment under inguinal ligament as hips pulled back with pushing/lithotomy. Usually resolves within max 3-6 mos.
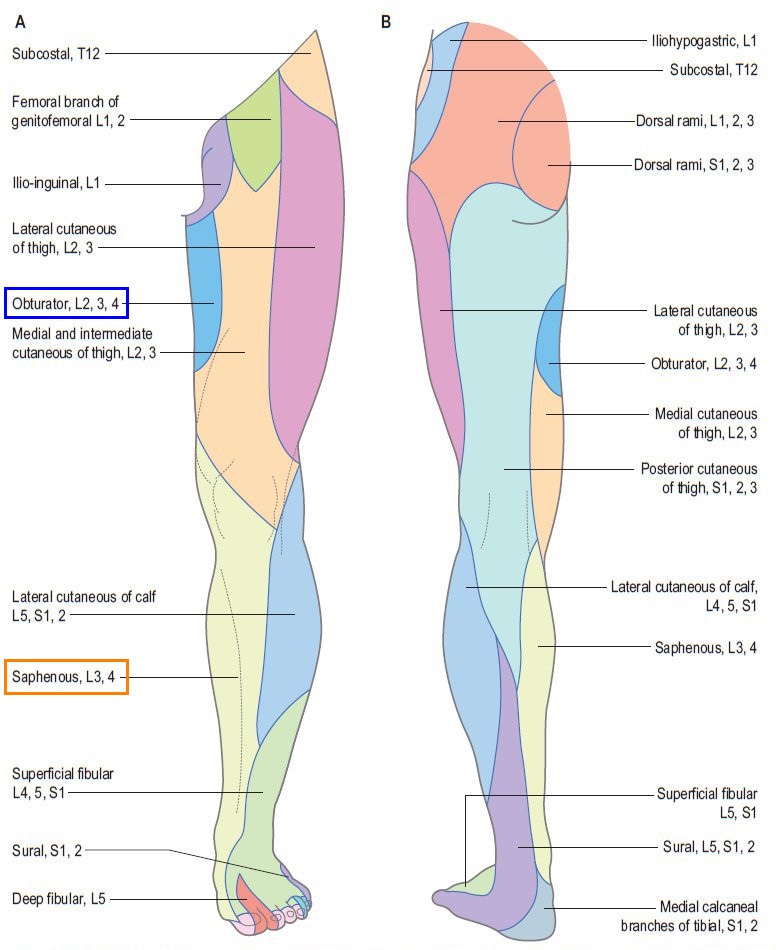
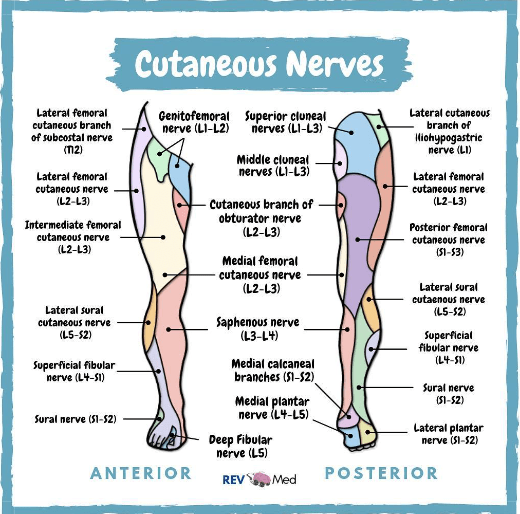
- S/S: burning pain over LFCN innervation: anterolateral thigh (L2-3) No motor involvement. – Usually one-sided but can be b/l if both LFCNs each compressed.
- Leg pain that is NOT meralgia paresthetica, and requires further workup:
- If pt had c/s with no lithotomy and no pushing – M.P. unlikely
- pain not localized to lateral thigh – M.P. unlikely
- Any motor deficit is NOT M.P. (LFCN sensory only)
DERMATOMES OF LEG
- Delayed *recovery* is just a local sensory deficit.
- A dermatome/leg that hasn’t fully recovered is different from one that recovered & then lost sensation again. As long as the sensory deficit never got worse and it slowly getting better, likely it never fully recovered vs an epidural hematoma causing new/worsening symptoms)
- So if no pain, no worsening s/s, no worsening motor deficit, just some unrecovered sensory defecit = probably delayed recovery – reassurance pt should keep improving. If any significant motor loss is present, it should more likely be b/l in setting of hematoma, but unilaterality is still possible. Small amount of motor deficit that never recovered on same side as unrecovered sensory deficit – if one sided – likely just a delayed recovery. Ask if block was one sided – sometimes one side just gets absolutely doused in LA, and those spinal nerve roots need a little more time to come back – esp when people are giving repeated high-concentration top-offs of 5cc/5cc lido2%/bupi0.25%
- Ask if it’s improved at all. Sometimes it’s just a very slow recovery in one area. Improvement, however slow, is reassuring, whereas worsening symptoms are VERY concerning, and warrant STAT MRI.
LOVENOX is a MAJOR risk factor for Epidural Hematoma
Not only is meticulous timing of restarting 1st dose of lovenox important, but timing the 2nd dose is just as important. Need FULL 24HRS between 1st, 2nd, and subsequent doses when re-starting lovenox
- USE ASRA COAGS APP. Link to app:
LOVENOX HOLD/RESTART times:
- Prophylactic vs Therapeutic doses!!! Different guidelines!!
- Consult and double check ASRA coags guidelines for all cases – they have all the different *specific* scenarios.
- Ex:) *Therapeutic* = 1.5-2 mg/kg/day- wait 24 hrs before neuraxial placement, and 24-72 hrs after placement to restart.
- Then another full 24hrs before second dose.
- At least 24h on either side of neuraxial procedure. Up to 3 days after for high-risk-bleeding-procedures.
Prophylactic vs therapeutic doses have different guidelines.
- Prophylactic = 40mg/day – wait at least 12hr before placing neuraxial, 12h to restart lovenox after PROCEDURE placement.
- + additional 4h after catheter removal, with minimum 12 hrs since procedure time:
- So if 11h after procedure, epidural catheter is removed, wait another 4h to restart prophylactic LMWH.
- If epidural catheter is removed 2 hrs after procedure, 12h after procedure is ok, bc 4 hrs have passed since catheter removal, and at least 12 hours since procedure placement.
- then another 24 hours before second dose.
Nerve Injury vs Hematoma Suspicion w/ Sensorimotor Complaints:
Meralgia Paresthetica
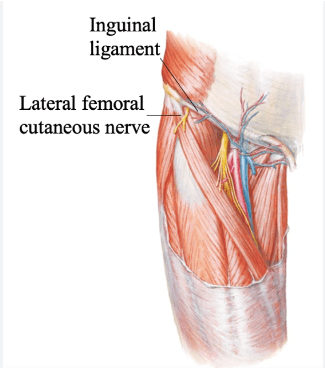
- Positioning nerve INJURY to Lateral Femoral Cutaneous Nerve (LFCN). LFCN is a SENSORY nerve with no motor innervation. LFCN injury 2/2 nerve being compressed under the inguinal ligament as it exits the pelvis.
- In OB patients, can be caused by legs being pulled back while PUSHING, or in lithotomy during c/s.
- Neuraxial anesthesia numbs pain of positioning/abnormal stretching/nerve injury – can go unnoticed until LA wears off
- If unmedicated, the pain of labor probably overrides this nerve compression pain – can go unnoticed until after delivery.
- In OB patients, can be caused by legs being pulled back while PUSHING, or in lithotomy during c/s.
- Will have cardinal S/S: tingling, numbness, &
burning painin anterolateral/outer thigh (L2-L3 dermatomes) with NO motor involvement. - Often one sided, but can be b/l if b/l LFCNs compressed.
- Sensory involvement in anterolateral thigh only in MP. LFCN does not have motor component, and does not innervate other areas besides anterolateral thigh.
Meralgia paresthetica affecting parturient women who underwent cesarean section -A case report-
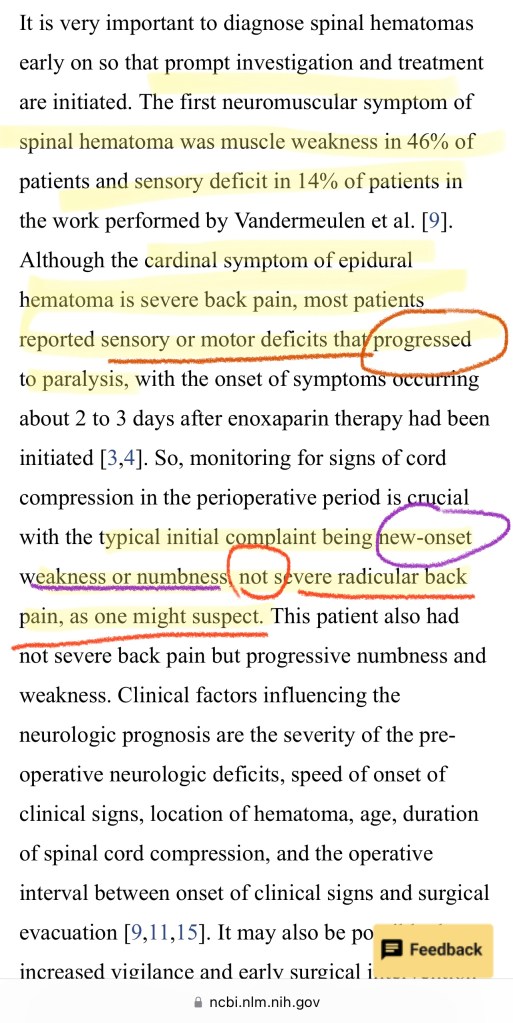
Versus s/s EPIDURAL HEMATOMA:
NYSORA Epidural Hematoma page:
- Recent studies on the incidence of spinal hematoma in patients without overt risk factors showed an increase to 1:18,000 after epidural and 1:3600, even 1:1000, in elderly patients undergoing lower extremity surgery.
- Hemorrhage into the spinal canal most commonly occurs in the epidural space because of the prominent epidural venous plexus.
- SEH may be spontaneous or may follow minor trauma, such as lumbar puncture or neuraxial anesthesia.
- SEH occurs primarily in anticoagulated or thrombocytopenic pts.
NEURO CONSULT & CAREFUL MONITORING:
- Pt may c/o severe, localized, constant back pain +/- a radicular component that may mimic disk herniation.
- Assc s/s may include wknss, numbness, & urinary/fecal incontinence.
- Return of sensory or motor deficit several hrs after spinal or epidural block has worn off (+/- back pain) is highly suspect —> work up & treat as hematoma until proven otherwise (STAT MRI)
- Neurologic recovery s/p conservative mgmt has been reported in pts with back pain & leg weakness without paralysis*.
- Neurologic recovery can occur if surgery and decompression is performed early enough (< 8-12 hrs.)
Diagnosis and Management of Spinal and Peripheral Nerve Hematoma
- In pregnant women, it’s been proposed that increased venous pressure 2/2 uterine enlargement, in association with hemodynamic changes of pregnancy, may predispose to rupture of the preexisting pathologic epidural venous plexus wall.
- Although a venous source is the most widely accepted, debate continues regarding a potential arterial source of SEH
- Proponents of this theory state that venous BP is less than intrathecal pressure, so although forward flow is possible into the low pressure epidural space, venous blood could not cause compression of the spinal cord.
** Suspected Epidural Hematoma = STAT MRI **
*spinal hardware is MRI compatible, if pt has had prior surgeries.
Online Lecture
Neurologic Complications in Obstetric Anesthesia – OpenAnesthesia
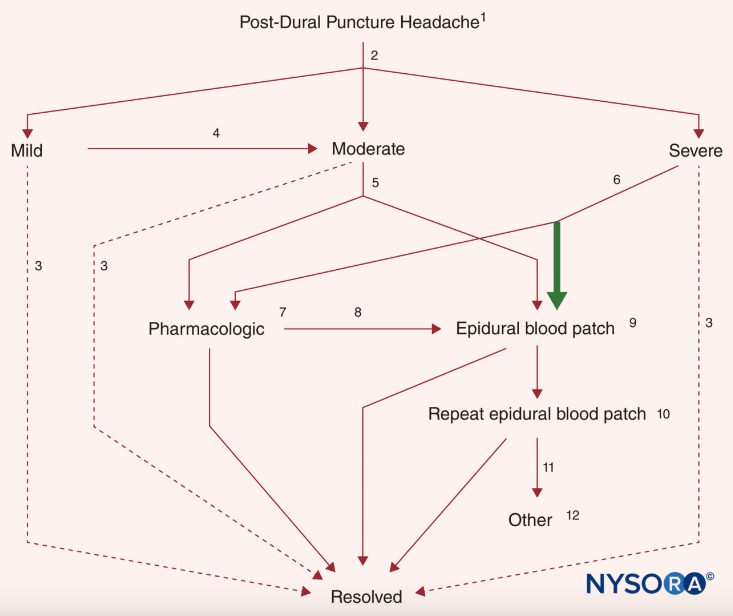
BLOOD PATCHES FOR PDPH

PDPH Usual S/S
- Brutal, incapacitating fronto-occipital headache
- Photophobia
- Postural headache pain changes
- Nuchal rigidity (++ pain when they flex neck and touch chin to chest)
- Neck Pain
- Tinnitus/ringing in ears
PDPH h/a and symptoms come from the cranium having less CSF in it, causing less pressure in the cranium = intracranial HOTN. Cerebral blood vessels dilate to increase blood volume which increase ICP to compensate for the cerebral HOTN. The cerebral vasodilation causes incapacitating headaches.
CSF
- CSF volume: ~150 cc [125cc (80%) in subarachnoid space, 25cc (20%) in ventricles]
- Produced at rate of ~20cc/hr, equaling 400-600cc/day
- PDPH headache from CSF loss would mean > 20cc/hr loss to create deficit and cause intracranial HOTN.
- Once dural hole is healed naturally, or closed/patched with EBP, it only takes a few hours to fully replete CSF (permanent relief from PDPH)
NYSORA pages on PDPH SUMMARY pdf:
PDPH QUICK NOTES:
POST-NEURAXIAL ROUNDING – RULE OUT PDPH
- – Pt should report no headache, no sensorimotor deficits, and be able to walk around.
Suspect PDPH IF:
1) HEADACHE: (usually delayed 12-48h post-procedure. H/A within 1hr is more likely pneumocephalus from AIR w/ LOR)
- H/A S/S in PDPH:
- Fronto-occipital – (Opth (CN51) nerve off trigeminal (CN5) = frontal pain, (CN9,10 = occipital pain)]
- Bilateral – Dull/aching, throbbing, or pressure-type
- Photophobia – Worsens w/ lights on – (CN 3, 4, & *6)
- Positional – Worsens sitting upright, improves lying down
- + Dizzy/vertigo: R/t diplopia/poor accommodation 2/2 CN palsy 3, 4, *6… (often unilateral)
- + Shoulder/neck pain&stiffness/nuchal rigidity: Cervical C1-3
- + Nausea/vomiting: CN10: vagal stimulation
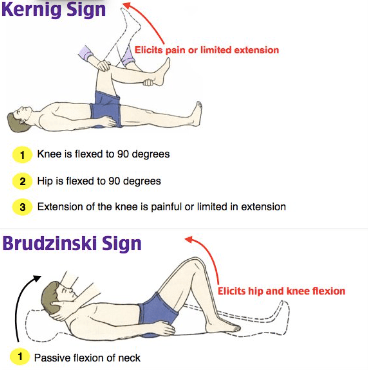
* * * * Headache must rule out: * * * *
– Postpartum PreE? : obtain BP
– Meningitis? : + Fever AND Kernig, Brudzinski, nucchal rigidity, n/v, dizziness, photophobia, or confusion –> neuro consult [CBC, LP, CT scan]
2) Visual changes? (often unilateral): double vision (diplopia) and poor accomodation [transient CN palsy 3, 4, 6 (extraocular eye muscles) esp CN6 (abducens: lateral rectus muscle)]
3) Auditory changes?: tinnitus [decreased perilymphatic pressures in inner ear –> imbalance btwn endolymph & perilymph]
ANY OF ABOVE AND Documented wet tap? Normotensive & afebrile? –> likely PDPH –> conservative tx +/- EBP
– Consult always indicated if serious non-PDPH h/a is suspected or cannot reasonably be ruled out. Lateralizing neurologic signs, fever/chills, seizures, or change in mental status are not consistent with a PDPH or benign h/a.
– Because PDPH generally resolve spontaneously, h/a that worsens over time and looses positional nature should be strongly suspected to be 2/2 to SDH (esp if focal neurologic signs or decreased mental status)
– Contraindications to the EBP similar to any neuraxial: coagulopathy, systemic sepsis, fever, infection at the site, and pt refusal. Theoretical concern of neoplastic seeding CNS in cancer pts – can use slower injections of smaller blood volumes in pts whose CNS may be vulnerable to injury from increased epidural pressures generated with EBP (eg: multiple sclerosis.)
– EBP has been safely provided to both acute Varicella and HIV pts.
– Although alternative/conservative tx has been proposed, EBP remains only proven tx for PDPH and therefore can be encouraged and performed early (within 24 hr of diagnosis) if symptoms are severe.
ASSESSING NEED FOR BLOOD PATCH
Is this a PDPH?
- Check NO HTN (r/o PreE/Eclampsia)
- Check NO FEVER (r/o meningitis)
** First get a BP. PreE & Eclampsia can both occur post-partum!!
- New h/a may be HTN/preE instead of spinal headache. If BP normal, then more likely spinal headache.
- Just like regular epidural we need CBC/plt +/- coags & TEG if pt had preE/HELLP/thrombocytopenia/AFLP/DIC etc etc etc
- If LOVENOX restarted (PDPH can occur > 24h after procedure), CANNOT place neuraxial until ASRA guidelines waiting period has passed.
Pt w/ FEVER : blood patch may be inadvisable if active bacteremia.
- could be meningitis – r/o source of infection.
- could be systemic infection we don’t want to potentially introduce to CSF (hole in dura from wet tap is there)
TREATMENT OPTIONS:
(bring yellow PDPH info sheet to pt – located in anesthesia OB office)
Conservative:
- PO Fluids, lights off, supine, Caffeine & Fiorcet (Butalbital 50mg, acetaminophen 325mg, caffeine 40mg)
- MOA Butalbital: barbituate CNS analgesic Et1/2 35hrs. Cafffeine induces cerebral vasoconstriction, and acts as analgesic adjuvant by enhancing efficacy of acetaminophen & aspirin by ~ 40%
- Unsuccefsul/ineffective —> perform EBP
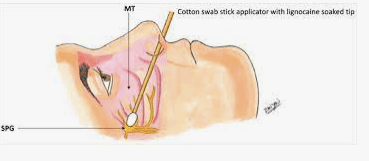
Sphenopalatine Ganglion Block (SPGB)
- Simple, minimally invasive procedure may help alleviate pain via local anesthesia as well as causing some cerebral vasoconstriction
- SPG is a junction which has sympathetic, parasympathetic, and sensory innervation overlapping in a tiny area. May explain how SPG block manages pain due to several etiologies.
- Parasympathetic activity is blocked, which inhibits the cerebral vasodilatation causing the PDPH symptoms.
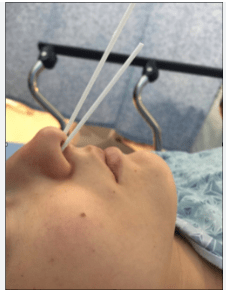
- TECHNIQUE:
- A long Q-tip applicator soaked with 2%-4% lidocaine or viscous lidocaine.
- Inserted parallel to floor of the nose until resistance met
- The swab will be at the posterior pharyngeal wall superior to the middle turbinate.
- Hold in place in the nostril for 5-10 minutes and then removed & repeat in the other nostril.
- The swab doesn’t come into direct contact with the SP ganglion, but the LA infiltrates around it in that position. The connective tissue and mucous membrane covering facilitates LA spread and penetration.
- SPGB PROS/CONS:
- PROs:
- May be helpful in pt on postpartum lovenox (DVT prophylaxis) to address pain in interim until EBP is possible 24h after last LMWH dose. Anticoagulated pts can still bleed from SPG, especially with engorged and fragile nasal mucosa & vasculature of pregnancy/postpartum period. However risk/benefit of pain relief vs epistaxis still better than high risk of EBP neuraxial hematoma.
- If pt refuses EBP, this may help.
- CONs:
- Doesn’t address closure of dural hole, as CSF continues to leak. Pt may get a few hrs of relief from SPGB, but once it wears off, h/a will return as CSF continues to leak – unless dural hole happens to heal while SPG is in place. Don’t want pt going home comfy with SPG and coming back in for PDPH treatment as SPG wears off. SPGB lasts ~8h, but variable as pdph improves.
- Still spending 20+ minutes procedural time in pt room as nares anesthetized for 10-15 mins. Might as well just do EBP if pt is appropriate and willing candidate, as EBP is shown to be more effective.
- PROs:

**EPIDURAL BLOOD PATCH (EBP)**
- Near-instant relief: comes from colloid, coagulated blood patch sitting in a little blood clot ball in the epidural space, and putting pressure on spinal canal to push CSF higher up into cranium, alleviating intracranial hypotension. (Raising water level for brain to float in). Once intracranial HOTN is reversed by increased CSF levels, the compensatory cerebral vasodilation (causing PDPH symptoms) is reduced. —> relief of symptoms.
- Since blood is a colloid, it won’t spread nicely through the epidural space like crystalloid would – so it’ll just kinda sit there around where you inject it and coagulate. This big fat clot may spread the epidural space a bit and create sensations of pressure, especially when lying down. (Compared to 20cc LA/saline/crystalloid which wouldn’t cause that pressure bc it spreads more evenly through the space) Reassure pt this pressure is normal.
- Continued relief: blood patch clots off hole in dura so CSF can regenerate without being lost and replenish normal volume.
- Normal adult CSF volume: ~150mL
- Generation: ~20mL/hr, 400-500mL/day
- Pt may have epidural space full of CSF – doesn’t necessarily mean you wet-tapped if a little bit of csf comes out through the Tuohy after LOR. Go slowly and carefully through ligamentum flavum to avoid another wet tap.
- EBP can be done in maternity room or triage area.
- Slow injection of ~ 20 cc sterile blood, inject until they feel some pressure in their back – then stop. May inject up to ~25 cc if pt feels no pressure at all (unusual)
- When pt lies down, they WILL NORMALLY feel lower back pressure, even if not felt during injection. This may last for a few hours. Reassure pt this is normal.
- USUALLY even if wet-tap occurred because the pt was a “difficult epidural,” 2/2 pt movement with discomfort, or anatomy issues and inability to properly position, USUALLY the EBP is MUCH easier to perform than the epidural was. Post-partum, there is no longer a giant belly in the way impairing proper positioning, and there are no contractions making her squirm and move.
EBP OFFICIAL PROCEDURE
Clinical Practice Reference: CPR.02.450 HH Dept of Anesthesia
Performing a Blood Patch on an Outpatient OB pt
- The attending anesthesiologist responsible for L&D will be notified when a patient with a postdural puncture headache (PDPH) may require an epidural blood patch (EBP).
- The anesthesiologist, or another member of the anesthesia team, can obtain a copy of the patient’s labor anesthesia record, evaluate the perioperative course, and then call the patient to evaluate if an EBP is the appropriate treatment.
- If an epidural blood patch is the appropriate intervention, and the patient agrees to
treatment, the anesthesiologist notifies the L&D Charge Nurse to discuss availability of a bed in the Triage area. Once a time has been agreed upon, the patient should receive a call notifying her what time to arrive and that she should come to N6/Triage. Once the patient arrives she will be admitted under “observation status” by the covering obstetrician for the patients group. - The patient should be instructed that she will: (1) need to have a ride to and from the hospital, (2) need to have someone care for her infant, if coming with her, and (3) that she will be here at least 1-2 hours.
- On arrival, the patient will be admitted to the observation unit and the triage secretary, or triage nurse, will notify the covering anesthesiologist of the patient’s location in triage. The Triage nurse will be responsible for:
a. Admitting the patient
b. Documenting baseline vital signs
c. Responding to her call button as needed
d. Instructing patient to use the bathroom, breastfeed, etc., prior to the EBP so
that she does not have to sit up or get out of bed during the first hours - The Anesthesia team procedural care responsibilities:
a. Starting a new “epidural blood patch” procedure in EPIC and completing the preanesthetic assessment on an anesthesia record
b. Explaining risks, benefits and obtaining consent for the procedure
c. Completing EBP, including obtaining blood using standard sterile technique
d. Completing a procedure note in EPIC
e. Discussing post procedure care with the nurse caring for the patient and placing a “nursing communication” order in EPIC with what is agreed upon (if necessary).
f. Writing the patient’s name and MRM on the PDPH list located in the OB anesthesia office so the day team can follow up with the patient.
g. Assuring that at least a pre-procedural and post-procedural set of vital signs are documented in the patients chart.
h. Giving the patient a PDPH information sheet and discharging the patient (as explained below).
- After the blood patch, the patient is instructed to remain supine in bed for approximately one hour. The anesthesia team will then evaluate for improvement in headache symptoms. If stable, the patient may be discharged home by notifying the nursing/OB team so the OB team can place the DC order.
- Patient should receive a PDPHA instruction sheet if she does not already have one. These yellow sheets are available in Triage, Bliss 6, and in the OB anesthesia office. The patient may continue conservative treatment as needed (fluids, caffeine, Fiorcet).
Performing a Blood Patch on a post-partum OB patient still admitted
The steps for performing a blood patch are the same except the blood patch can be completed in the patients private room on post-partum and any post-op instructions can be communicated to the patient’s nurse through a “nursing communication.”
Online Lecture:
Post-Dural Puncture Headache and Epidural Blood Patch – OpenAnesthesia
Epidural blood patch – MOA explained:
YOUTUBE SPG:
Sphenopalatine Ganglion Blocks for Postdural Puncture Headache
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5392662/
Case study for Tinnitus as only symptom:
Blood patch for the treatment of post-dural puncture tinnitus